Last Updated on November 17, 2025 by Ugurkan Demir
When dealing with complex blood disorders, knowing the bone marrow transplant types, especially autologous vs allogeneic bone marrow transplant, is key. At Liv Hospital, a trusted leader in this field, the focus is on patient-centered care and the latest advancements. The Bone Marrow Transplant Center at Liv Hospital provides autologous transplants, which use the patient’s own stem cells, and allogeneic transplants, which use donor cells from siblings, parents, or unrelated donors. They use state-of-the-art technology and collaborate with bone marrow banks locally and internationally to find the best matches. This comprehensive approach ensures personalized, effective treatment for various blood and immune system diseases, including leukemia, lymphoma, multiple myeloma, and aplastic anemia. The hospital’s experienced medical team and advanced facilities deliver high success rates and quality care tailored to each patient’s needs.
A bone marrow transplant puts healthy stem cells into your body. This replaces dysfunctional bone marrow. It’s vital for many blood-related cancers and disorders.
We know how important it is to understand the types of bone marrow transplants. This includes autologous and allogeneic transplants. We aim to give our patients the best care possible.

Bone marrow transplantation, also known as a stem cell transplant, is a treatment. It replaces a patient’s bone marrow with healthy stem cells. This is key for patients with bone marrow issues, like cancer.
By understanding bone marrow transplantation, we see how it helps. It restores normal blood cell production.
Bone marrow is the spongy tissue in some bones that makes blood cells. It’s vital for our health, helping fight infections and carrying oxygen. It also helps blood to clot.
If bone marrow is sick or damaged, it can’t do these jobs. That’s why bone marrow transplantation is needed. It replaces unhealthy bone marrow with healthy stem cells, fixing blood cell production.
Stem cells in bone marrow can turn into different blood cells. They can become red blood cells, white blood cells, and platelets. This process, called hematopoiesis, keeps our blood and immune system healthy.
Choosing between using a patient’s own stem cells or donor cells is important in bone marrow transplantation. For more details,
Medical Conditions Requiring Bone Marrow Transplants
Many blood-related disorders and cancers can be treated with bone marrow transplants. This method has become a key treatment for serious diseases.
We use bone marrow transplants for different conditions. These include various types of leukemia, lymphoma, and multiple myeloma. These cancers affect the blood and bone marrow, making transplantation a vital treatment approach.
Leukemia is a cancer of the blood and bone marrow, with abnormal white blood cells growing uncontrollably. Lymphoma affects the immune system, and multiple myeloma is a cancer of plasma cells in the bone marrow. Bone marrow transplants offer a potentially curative treatment for these conditions by replacing the diseased marrow with healthy cells.
Types of Leukemia Treated with Bone Marrow Transplants:
Non-malignant blood disorders, such as aplastic anemia, can also be treated with bone marrow transplants. Aplastic anemia occurs when the bone marrow fails to produce blood cells, leading to severe anemia, infections, and bleeding.
| Condition | Description | Treatment Approach |
| Aplastic Anemia | Bone marrow failure to produce blood cells | Bone Marrow Transplant |
| Leukemia | Cancer of the blood and bone marrow | Chemotherapy and Bone Marrow Transplant |
| Lymphoma | Cancer of the immune system | Chemotherapy, Radiation, and Bone Marrow Transplant |
Immune deficiency syndromes, such as Severe Combined Immunodeficiency (SCID), can be treated with bone marrow transplants. These conditions result from genetic defects that impair the immune system’s function, making patients highly susceptible to infections.
Bone marrow transplantation offers a cure for many of these immune deficiencies by replacing the defective immune cells with healthy ones from a donor.
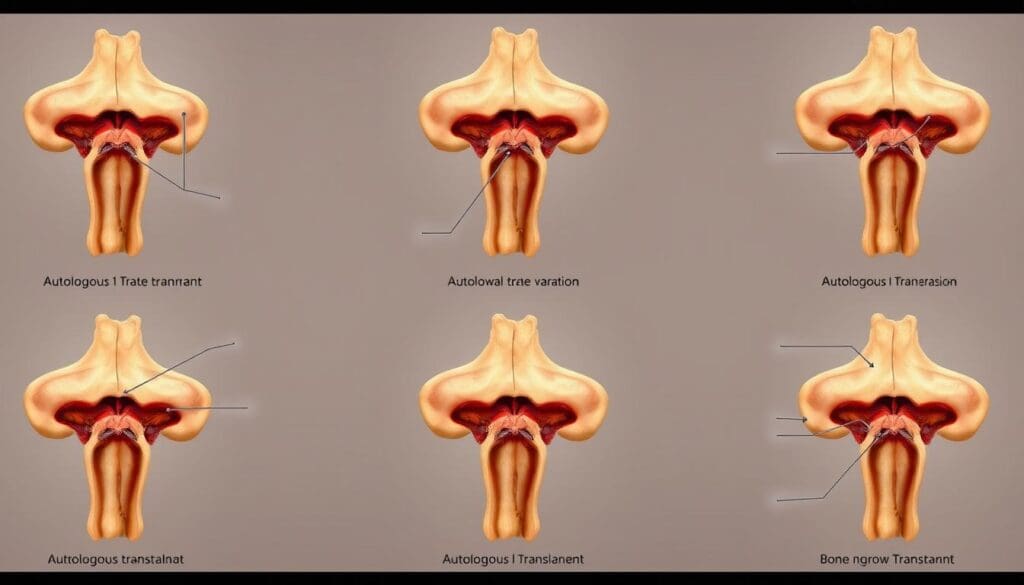
When it comes to bone marrow transplantation, knowing the difference between autologous and allogeneic transplants is key. This knowledge helps decide the best treatment path. Let’s dive into the main differences between these two transplant types.
Autologous bone marrow transplants use the patient’s own stem cells. These cells are collected, stored, and then given back after a treatment. This method avoids graft-versus-host disease (GVHD), a big risk with allogeneic transplants.
Allogeneic transplants, on the other hand, use stem cells from a donor. This can help fight cancer, but also risks GVHD.
Choosing between autologous and allogeneic transplants depends on several factors. These include the disease type, the patient’s health, and whether a suitable donor is available.
The disease type greatly influences the transplant choice. For example, autologous transplants are often used for multiple myeloma and some lymphomas. This is because the patient’s cells aren’t involved in the disease.
Allogeneic transplants are usually for diseases where donor cells can help, like some leukemias. We look at disease relapse risk and graft-versus-tumor effect benefits when picking a transplant type.
Immune system recovery varies between autologous and allogeneic transplants. Autologous transplants lead to quicker immune system recovery because the patient’s cells are used. Allogeneic transplants take longer because donor cells need to mature and work in the recipient’s body.
Grasping these differences is vital for setting patient expectations and ensuring proper care after the transplant.
Autologous bone marrow transplant, or autologous stem cell transplant, is a treatment. It involves giving patients their own stem cells after high-dose chemotherapy. This method is very helpful for some cancer patients.
The first step is to collect the patient’s stem cells. These can come from the bone marrow or blood. The stem cells are then stored until they’re needed after chemotherapy.
We use a method called apheresis to get stem cells from the blood. This involves:
Autologous bone marrow transplantation is often used for:
These conditions can get better with high-dose chemotherapy and the patient’s own stem cells. This helps rebuild the bone marrow and fix the immune system.
The recovery timeline can vary, but it usually takes weeks to months for the bone marrow to heal. Patients can expect:
We keep a close eye on patients during this time. We manage any complications and offer support as needed.
Allogeneic bone marrow transplantation uses donor stem cells. It replaces a patient’s bone marrow with healthy stem cells. This can cure many blood-related disorders.
HLA (Human Leukocyte Antigen) matching is key in allogeneic bone marrow transplantation. It helps avoid graft rejection and graft-versus-host disease (GVHD). We pick donors based on HLA compatibility for the best results.
We test for HLA alleles to find a match. The closer the match, the lower the risk of problems. We use advanced techniques to find donors, whether they’re related or not.
Managing graft-versus-host disease (GVHD) is a big challenge. GVHD happens when the donor’s immune cells attack the recipient’s body. We use immunosuppressive drugs and monitor the patient closely.
GVHD can be acute or chronic, needing different treatments. We customize our plans for each patient, balancing GVHD prevention and disease relapse risk.
The graft-versus-tumor (GVT) effect is a big plus of allogeneic bone marrow transplantation. The donor’s immune cells can kill cancer cells in the recipient. This is very helpful for some leukemia or lymphoma patients.
The GVT effect is linked to GVHD. By managing GVHD well, we can also use the GVT effect to help patients.
When a family donor isn’t available, the Be The Match Registry offers hope. It searches for a compatible donor through registries. This is a big help for those needing a bone marrow transplant without a family donor.
The National Marrow Donor Program (NMDP) and the Be The Match Registry lead in finding unrelated donors. The NMDP runs the Be The Match Registry, the biggest donor and cord blood unit registry. It now has millions of donors, making it easier to find a match for patients.
We know how vital these registries are. The Be The Match Registry not only finds donors but also supports patients and donors. It offers resources and guidance throughout the transplant journey.
The matching process for unrelated donors uses HLA typing. This is key to seeing if the donor and recipient are compatible. The transplant’s success depends on HLA matching, the recipient’s health, and the disease being treated.
Success rates for MUD transplants have gotten better over time. This is thanks to better HLA typing and matching, and improved care. But success can vary based on the transplant’s details.
While MUD transplants offer hope, they also face unique challenges. A big worry is graft-versus-host disease (GVHD). This is when the donor’s immune cells attack the recipient’s tissues. Managing GVHD is a key part of post-transplant care.
Finding a fully matched donor can also be tough, mainly for patients from diverse backgrounds. Work is being done to increase diversity in donor registries. This aims to improve the chances of finding a match for all patients.
We know that dealing with MUD transplant challenges can be tough. But, with the Be The Match Registry’s help and medical progress, patient outcomes are getting better.
For patients with an identical twin, syngeneic transplantation is a promising option. It offers a bone marrow transplant that closely matches the patient’s own biology. This is because of the perfect genetic match between twins.
The main advantage of syngeneic transplantation is the perfect genetic match between donor and recipient. This reduces the risk of graft-versus-host disease (GVHD) to almost zero. It makes recovery smoother and lowers the need for strong immunosuppressive drugs.
Genetic identicalness in syngeneic transplantation also means a lower risk of graft rejection. The recipient’s immune system is less likely to see the donor cells as foreign. This makes post-transplant care easier and improves the treatment’s outcome.
Despite its benefits, syngeneic transplantation has a drawback. It may lose the graft-versus-tumor (GVT) effect. The GVT effect helps fight cancer cells. But, with identical genetics, this effect might be weaker, affecting treatment success over time.
Syngeneic transplantation is rare because it requires an identical twin. Yet, for those who can, it’s a chance for a potentially life-saving treatment with fewer immune issues.
Tandem transplants are a treatment method that involves two transplants in a row. This is mainly for patients with multiple myeloma and other specific conditions. It aims to improve treatment results.
Tandem transplants are mainly for treating multiple myeloma, a blood cancer. It’s used when the disease is aggressive or has come back. This intense treatment is a last resort.
It’s also considered for some lymphoma and other blood cancers. In these cases, the benefits of a second transplant are seen as worth the risks.
The process for tandem transplants includes several steps:
The time between the two transplants is important. It depends on how well the patient recovers and their overall health.
Recovery between the two transplants is key. It needs close monitoring and supportive care. Patients are watched for signs of infection, graft failure, or other issues.
| Recovery Aspect | First Transplant | Second Transplant |
| Average Recovery Time | 2-4 weeks | 2-4 weeks |
| Common Complications | Infection, mucositis | Infection, graft failure |
| Supportive Care | Antibiotics, pain management | Growth factors, monitoring |
It’s important for patients and healthcare providers to understand tandem transplant protocols and recovery. This helps navigate this complex treatment effectively.
Haploidentical transplantation uses family donors who are only partially matched. This method is key in treating blood disorders. It also increases the chances of finding a bone marrow donor for patients.
Family members like parents, children, or siblings can be donors. They share half of the patient’s genes. This partial match is enough for a transplant when a full match isn’t found.
Using family donors means stem cells can be found faster. This is very important for patients who need a transplant quickly.
T-cell depletion is vital to prevent graft-versus-host disease (GVHD) in haploidentical transplants. It removes T-cells from the donor graft. This reduces the immune reaction against the recipient’s body.
There are different ways to deplete T-cells. One method is ex vivo T-cell depletion. This is when the donor cells are treated outside the body to remove T-cells.
The post-transplant cyclophosphamide protocol helps prevent GVHD. Cyclophosphamide is given after the transplant. It kills donor T-cells that could cause GVHD.
This protocol has been shown to work well. It reduces GVHD without harming the graft’s ability to fight cancer.
In summary, haploidentical transplantation is a valuable option for patients without a fully matched donor. Using partially matched family donors and strategies like T-cell depletion and post-transplant cyclophosphamide leads to successful transplants. This improves patient survival rates.
It’s important to know where stem cells come from for bone marrow transplants. They can be found in bone marrow, peripheral blood, or cord blood. Each has its own benefits and things to consider.
Getting stem cells from different sources is quite different. Bone marrow collection takes stem cells directly from the marrow, usually from the hips, under anesthesia. On the other hand, peripheral blood stem cells are collected after they’re moved from the bone marrow into the blood with special drugs and apheresis. Cord blood is collected after birth, by clamping the umbilical cord and taking blood from the placenta and cord.
Each method is different in how invasive it is, the risks involved, and how many stem cells you can get. For example, getting stem cells from bone marrow is more invasive and risky than getting them from peripheral blood.
Choosing where to get stem cells depends on many things. These include the patient’s health, who can donate, and what the transplant needs. Bone marrow has been used a lot in transplants because it’s full of stem cells. Peripheral blood stem cells are used more now because they’re easier to get and there’s more of them. Cord blood is limited but easy to get and has less risk of problems with the transplant.
The need for matching stem cells for transplants changes based on where they come from. Human Leukocyte Antigen (HLA) matching is key for transplants from others, with the need for matching varying by source. Cord blood is more flexible with HLA matches, making it a good choice when a perfect match isn’t available.
| Stem Cell Source | Collection Method | Advantages | Matching Requirements |
| Bone Marrow | Direct harvesting from the hip bones under anesthesia | Rich source of stem cells, historical use | High HLA matching required |
| Peripheral Blood | Mobilization and apheresis | Ease of collection, higher yield | High HLA matching required |
| Cord Blood | Collection after birth from the umbilical cord | Readily available, lower risk of GVHD | More forgiving of HLA mismatches |
Understanding the bone marrow transplant journey is key for patients. It involves several steps, from the first evaluation to aftercare.
The journey starts with a detailed pre-transplant evaluation. This step is vital to see if a patient can have a bone marrow transplant. It includes tests and talks with doctors to check the patient’s health and condition.
Preparation also means talking about the risks and benefits of the transplant. Patients learn about expected outcomes and possible complications.
Before the transplant, patients go through a conditioning regimen. There are two main types: myeloablative and reduced intensity.
Myeloablative conditioning uses strong chemotherapy and/or radiation to clear the bone marrow. It’s more intense and used for some cancers or diseases.
“The choice between myeloablative and reduced intensity conditioning depends on various factors, including the patient’s age, overall health, and the specific disease being treated.” – A renowned Hematologist
Reduced intensity conditioning uses lower doses of chemotherapy and/or radiation. It’s less intense and used for older patients or those with health issues.
The stem cell infusion day is a big moment. The infusion itself takes about 30 minutes to an hour. After, the stem cells go to the bone marrow to make new blood cells.
Engraftment is when the stem cells start working and making blood cells. It’s important to watch this process closely. Patients are checked for signs of engraftment and get support as needed.
The transplant journey is complex and unique for each patient. Knowing each step helps patients and families understand this challenging but potentially life-saving treatment.
Advances in bone marrow transplantation are making a big difference for patients with blood cancers and disorders. New research and techniques are improving treatment options and care for patients.
New technologies and strategies are emerging, promising better survival rates and quality of life for patients. The future of bone marrow transplantation looks bright, with breakthroughs in haploidentical transplantation and managing graft-versus-host disease.
We at our institution are dedicated to providing the latest and most effective treatments. By keeping up with the latest in bone marrow transplantation, we offer personalized care and better outcomes for our patients.
As the field keeps growing, we’re excited for the ongoing improvement in bone marrow transplantation. This will lead to better patient outcomes and a brighter future for those in need.
Autologous transplants use the patient’s own stem cells. Allogeneic transplants use donor stem cells. The choice depends on the disease, the patient’s health, and donor availability.
A MUD transplant is for patients without a matched relative. It uses a donor found through registries like Be The Match.
Syngeneic transplantation uses stem cells from an identical twin. This provides a perfect match, reducing graft rejection and disease risk.
Tandem transplants involve two transplants for conditions like multiple myeloma. It requires careful planning and stem cell collection.
Haploidentical transplantation uses partially matched family donors. It requires special techniques to avoid disease risk.
Stem cells come from bone marrow, blood, and cord blood. Each source has its own collection methods and matching needs.
The journey includes pre-transplant checks, conditioning, and stem cell infusion. Understanding these steps helps patients prepare.
GVHD is a risk of allogeneic transplants, where donor cells attack the recipient. Management strategies can reduce this risk.
The graft-versus-tumor effect is when donor cells fight cancer cells. It’s beneficial for treating some cancers.
Transplants treat various conditions, including leukemia, lymphoma, and multiple myeloma. They also help with non-malignant blood disorders and immune deficiencies.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!