Last Updated on December 2, 2025 by Bilal Hasdemir
Endoscopic procedures are key in modern medicine. They help with minimally invasive diagnoses and treatments. But, are you awake during these procedures? It all depends on the anesthesia used.
Different anesthetics are used for endoscopic surgeries. Conscious sedation is often chosen. It keeps patients relaxed and comfortable, yet they can breathe on their own.
Key Takeaways
- Endoscopic surgery can be performed under different types of anesthesia.
- Conscious sedation is a popular choice for many endoscopic procedures.
- Being “awake” during endoscopic surgery means being in a state of conscious sedation.
- The type of anesthesia used depends on the procedure and patient needs.
- Discussing anesthesia options with your doctor can help alleviate concerns.
Understanding Endoscopic Surgery
Endoscopic surgery is a big step forward in medical tech. It makes surgery less scary for patients. It’s changed how doctors diagnose and treat many health issues.
What Is Endoscopic Surgery?
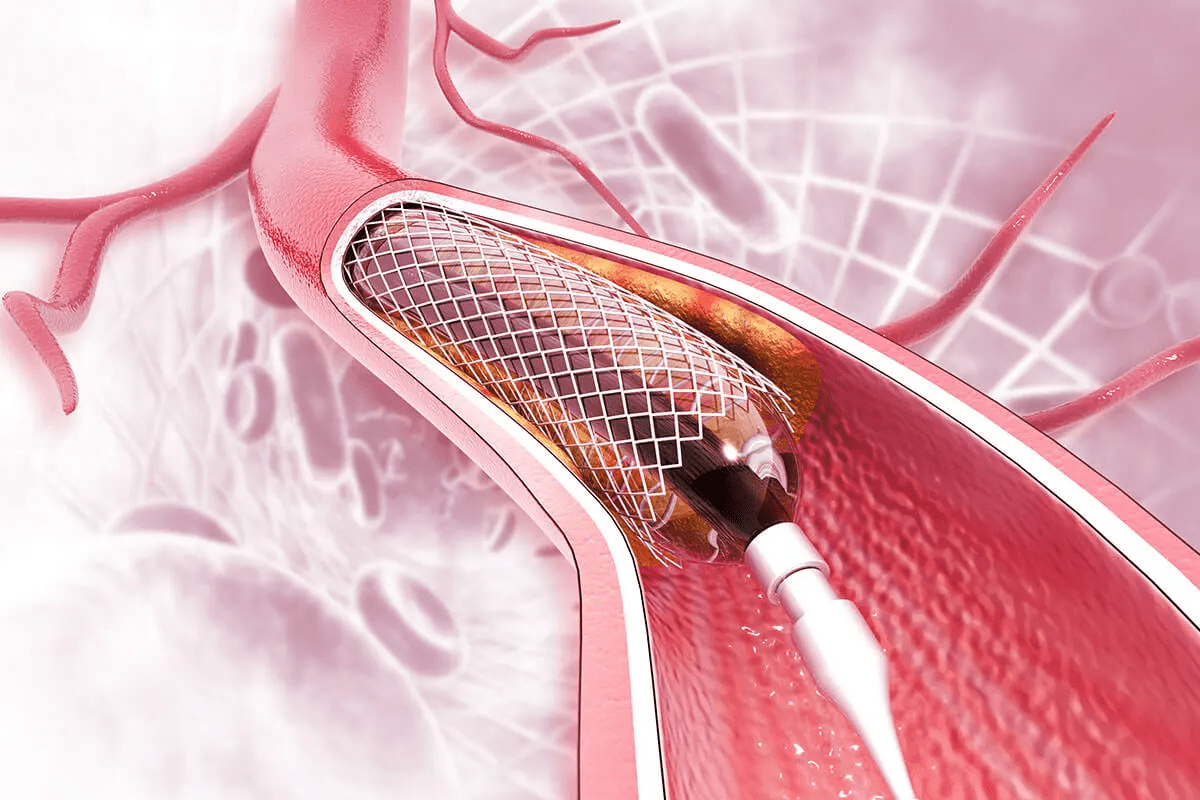
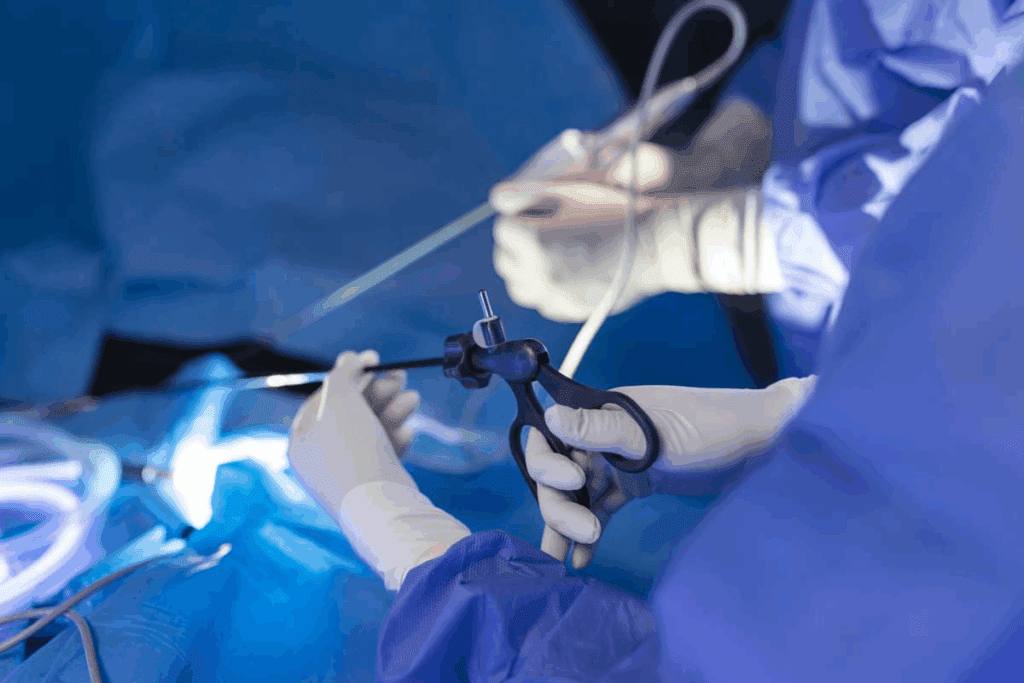
Endoscopic surgery uses a tube with a camera and light to see inside the body. Surgeons can do operations through tiny cuts. This means less damage to tissues and quicker healing.
The tube is linked to a monitor, showing what’s happening inside. This helps surgeons work with great accuracy, without harming too much of the surrounding tissue.
Common Types of Endoscopic Procedures
There are many endoscopic procedures done, like:
- Gastrointestinal endoscopy for the digestive tract
- Arthroscopy for joint issues
- Bronchoscopy for airway checks
- Laparoscopy for abdominal surgeries
Doctors pick the right procedure based on the patient’s needs.
Benefits of Minimally Invasive Approaches
Endoscopic surgery has many benefits, such as:
- Smaller cuts mean less scarring
- Less pain and discomfort after surgery
- Shorter hospital stays and recovery times
- Lower chance of complications and infections
These advantages lead to better health outcomes and happier patients.
Anesthesia Options for Endoscopic Procedures
Anesthesia for endoscopic procedures varies. There are several options to fit different needs. The right choice can greatly affect the patient’s experience and the procedure’s success.
General Anesthesia
General anesthesia makes the patient completely unconscious. It’s often used for complex procedures or when the patient’s health requires it. This ensures the patient is pain-free and remains motionless during the procedure. But, it comes with more risks and a longer recovery time.
Conscious Sedation
Conscious sedation relaxes the patient, allowing them to respond to commands but not remember the procedure. This method is common for many endoscopic procedures, balancing comfort and safety. Patients are closely monitored to ensure their safety and comfort.
Local Anesthesia
Local anesthesia numbs the area where the procedure is done, keeping the patient awake and alert. This is often used for simpler procedures. It has fewer side effects and quicker recovery times compared to other methods.
No Sedation Approaches
Some procedures can be done without sedation, relying on the patient’s ability to handle minimal discomfort. This is usually for patients at high risk for sedation complications or past adverse reactions. The decision to skip sedation depends on the patient’s health and the procedure’s nature.
Knowing the different anesthesia options for endoscopic procedures helps patients make better choices. By talking to their healthcare provider, patients can pick the best anesthesia for their needs.
Are You Awake During Endoscopic Surgery?
Many patients wonder if they’ll be awake during endoscopic surgery. It depends on the procedure type, patient health, and chosen anesthesia.
Defining “Awake” in Medical Contexts
In medical terms, “awake” means a patient is conscious and can respond. But, the level of awareness changes with anesthesia types.
We use various anesthetics for comfort during endoscopy. These include local, conscious sedation, and general anesthesia. Local numbs a specific area. Conscious sedation relaxes you. General anesthesia makes you completely unconscious.
Consciousness Spectrum During Procedures
Consciousness levels during procedures vary widely. Patients under general anesthesia are completely out. Those with local anesthesia or no sedation are fully awake, possibly feeling discomfort or anxiety.
Conscious sedation is in the middle. Patients are relaxed but can respond to commands or touch.
Procedure-Specific Consciousness Levels
Endoscopic procedures need different consciousness levels. For example, a simple gastroscopy might use conscious sedation. But, a complex procedure might need general anesthesia.
The anesthesia choice depends on the procedure’s complexity, patient health, and preference.
Memory Formation During Sedation
Patients often worry about remembering the procedure. Memory formation under sedation varies. Some might have fragmented memories or no recall at all.
We aim to make patients comfortable and positive about their experience. We discuss anesthesia options and what to expect.
Types of Endoscopic Procedures and Their Sedation Requirements
Endoscopic procedures come in many forms, each with its own sedation needs. We’ll look at these needs for each procedure. This ensures patients are ready for their specific procedure.
Upper GI Endoscopy
Upper GI endoscopy looks at the upper digestive system. Sedation helps patients relax during the exam. The sedation level can change, based on the patient’s anxiety and the procedure’s complexity.
Colonoscopy
Colonoscopy checks the colon and rectum’s lining. Conscious sedation is often used for comfort. The sedation choice depends on the patient’s health and past sedation experiences.
Bronchoscopy
Bronchoscopy examines airways with a camera tube. Sedation minimizes discomfort. The sedation type varies, based on the procedure and patient’s condition.
Arthroscopy
Arthroscopy lets doctors see inside joints with a camera. While often under general anesthesia, some procedures use local or regional anesthesia with sedation. The anesthesia choice depends on the joint and patient’s health.
In summary, sedation for endoscopic procedures varies by procedure, patient health, and anxiety level. Knowing these factors helps tailor sedation for a safe, comfortable experience.
Conscious Sedation: The Middle Ground
For those facing endoscopic surgery, conscious sedation is a good choice. It balances being awake and not fully asleep like general anesthesia. This method is popular because it makes patients comfortable, safe, and recovers faster.
How Conscious Sedation Works
Conscious sedation uses sedative drugs to relax patients during procedures. It doesn’t make them fully asleep like general anesthesia. Instead, it makes them relaxed and less anxious, so they can stay somewhat aware.
We mix different medications to get the right sedation level. The drugs we choose depend on the procedure, the patient’s health, and how they react to sedatives.
Medications Used
The drugs for conscious sedation are benzodiazepines and opioids. Benzodiazepines, like midazolam, reduce anxiety. Opioids, such as fentanyl, help with pain. We adjust the dose carefully to ensure patients can breathe and respond to commands.
Medication Class | Example Drugs | Purpose |
Benzodiazepines | Midazolam | Anxiety relief |
Opioids | Fentanyl | Pain relief |
What Patients Experience
Patients feel relaxed and comfortable during conscious sedation. They might be sleepy but can usually respond to commands or touch. Some might not remember the procedure because of the sedatives’ effects.
Key benefits include less anxiety, minimal discomfort, and a quicker recovery than general anesthesia.
Monitoring During Conscious Sedation
We watch vital signs like heart rate, blood pressure, and oxygen levels during the procedure. This lets us adjust sedation levels and quickly handle any problems.
Knowing how conscious sedation works and what to expect helps patients feel more comfortable during endoscopic procedures. Our team aims to make the experience safe and comfortable, tailoring it to each patient’s needs.
Benefits of Being Awake During Endoscopic Procedures
Being awake during endoscopic surgery has many benefits. It improves patient cooperation and reduces recovery times. This makes the whole experience better and more successful.
Patient Cooperation Advantages
Patients who are awake can follow instructions better. This is key for certain endoscopic exams that need patient help. It makes the procedure safer and more efficient.
Reduced Anesthesia Risks
Being awake lowers the risks of anesthesia. General anesthesia can cause breathing problems, allergic reactions, and longer recovery. Avoiding it reduces these risks.
Faster Recovery Times
Patients awake during procedures recover faster than those under general anesthesia. They skip the anesthesia’s effects, leading to quicker recovery and discharge.
Cost Considerations
The cost of endoscopic procedures can vary with anesthesia type. Procedures with the patient awake are often cheaper. This is because they need less anesthesia and have shorter recovery times. This can greatly reduce the total cost of care.
Benefits | Description | Impact |
Patient Cooperation | Improved ability to follow instructions during the procedure | More efficient and safer procedure |
Reduced Anesthesia Risks | Minimized risks associated with general anesthesia | Lower risk of complications |
Faster Recovery Times | Quicker recovery due to avoidance of general anesthesia | Sooner discharge and return to normal activities |
Cost Considerations | Lower costs due to reduced need for anesthesia and shorter recovery | More affordable care |
When General Anesthesia Is Necessary for Endoscopic Surgery
Choosing general anesthesia for endoscopic surgery depends on several factors. Some procedures can be done with conscious sedation or local anesthesia. But, for safety and comfort, some cases need full anesthesia.
Complex Surgical Endoscopy
For complex endoscopic surgeries, general anesthesia is often needed. This is because the patient must stay very calm and pain-free. For example, procedures like endoscopic submucosal dissection (ESD) for early gastric cancer require precise movements and a stable environment, making general anesthesia a preferred choice.
Patient-Specific Factors
Each patient’s needs play a big role in deciding on general anesthesia. Patients with severe anxiety or past traumatic medical experiences may need full anesthesia to avoid more stress. Also, those with medical conditions that make it hard to lie down or tolerate sedation might need general anesthesia.
Medical experts say, “The choice of anesthesia should be tailored to the individual patient’s needs and the specific requirements of the procedure.” (
This patient-centered approach ensures that the patient receives the most appropriate care.
Duration of Procedure
The length of the procedure is also important. Longer procedures can be uncomfortable and risky under conscious sedation. General anesthesia is often used for longer procedures to keep the patient comfortable and safe.
Risk Assessment
Before starting, a detailed risk assessment is done. This looks at the patient’s health, the procedure’s complexity, and the risk of complications. If the risk is high, general anesthesia is recommended to protect the patient’s safety.
The decision to use general anesthesia for endoscopic surgery is made for each patient individually. By carefully looking at these factors, healthcare providers can make sure patients get the best care for their situation.
Patient Experience During Awake Endoscopic Procedures
Awake endoscopic procedures need a deep understanding of the patient’s experience. This ensures comfort and safety. Being awake during a procedure can make many patients anxious.
Sensations and Awareness
Patients may feel sensations like mild discomfort or pressure during these procedures. These feelings are usually short-lived and can be managed. It’s important for patients to talk to the medical team about any discomfort.
Some patients might feel more aware or sensitive during the procedure. This could be because of the procedure itself or the sedation used. We make sure patients know what to expect to lower their anxiety.
Communication with Medical Team
Good communication between the patient and the medical team is key during awake procedures. Patients should share any discomfort or concerns. This helps the medical team adjust their approach to keep the patient comfortable.
We talk to patients about the procedure before it starts. We discuss the sedation or anesthesia and answer any questions or fears. This conversation is important for a smooth and comfortable experience.
Pain Management Strategies
We focus on effective pain management for awake endoscopic procedures. We use local anesthesia and conscious sedation to reduce pain. The choice of strategy depends on the procedure, the patient’s health, and their preferences.
Local anesthesia numbs the area where the procedure is done, reducing discomfort. Sometimes, conscious sedation is used to help the patient relax and not feel as much of the procedure.
Real Patient Testimonials
Many patients have a positive experience with awake endoscopic procedures. They praise the professionalism and care of the medical team. As one patient said,
“The team explained everything clearly, and I felt comfortable throughout the procedure. The follow-up care was also excellent.”
These testimonials show the value of the medical team’s skill and emotional support. We aim to provide this high level of care to all our patients.
Preparing for an Endoscopic Procedure
Endoscopic procedures are minimally invasive but need careful preparation for the best results. Knowing what to do before your procedure can make a big difference in your experience.
Pre-Procedure Consultations
You’ll have a consultation with your healthcare provider before the procedure. This is a key time to talk about your medical history and any medications you’re taking. It’s also when you can ask any questions and get answers.
Your healthcare team will explain the procedure in detail. They’ll tell you what to expect during and after it.
Discussing Anesthesia Options
Talking about anesthesia options is a big part of your consultation. You might choose between general anesthesia, conscious sedation, local anesthesia, or no sedation. Your healthcare provider will pick the best option for you based on your needs and the procedure.
Physical Preparation
Physical preparation might include dietary restrictions and changes to your medication. Your healthcare provider will give you specific instructions. For example, you might need to fast before the procedure or stop certain medications.
Mental Preparation
Mental preparation is just as important as physical. Knowing what to expect and understanding the recovery process can reduce anxiety. Techniques like deep breathing or meditation can help. Having a supportive friend or family member with you can also be beneficial.
By preparing well for your endoscopic procedure, you can make it a smooth and successful experience. Remember, your healthcare team is there to support you every step of the way.
Managing Anxiety About Being Awake During Procedures
Being awake during endoscopic procedures can be scary for many. The fear of the unknown can feel overwhelming. But, there are ways to handle this anxiety well.
Pre-Medication Options
Some patients might take pre-medication to lower their anxiety before the procedure. These drugs are usually given by mouth or through an IV.
Common pre-medication options include:
- Anti-anxiety medications
- Sedatives
Relaxation Techniques
Relaxation techniques can really help reduce anxiety. Deep breathing, progressive muscle relaxation, and visualization can calm your mind and body.
Here is a comparison of some relaxation techniques:
Technique | Description | Benefits |
Deep Breathing | Focuses on slow, deliberate breaths | Reduces heart rate, promotes relaxation |
Progressive Muscle Relaxation | Involves tensing and relaxing muscle groups | Reduces physical tension |
Visualization | Involves imagining a peaceful scene | Distracts from anxiety, promotes calm |
Communication Strategies
Talking openly with your healthcare team is key. Sharing your fears and worries helps them meet your needs better.
Key communication tips:
- Be open about your anxiety
- Ask questions about the procedure
- Discuss your preferences for sedation or other anxiety management options
Support Resources
A support system can make a big difference. This can include family, friends, or support groups.
Some patients also find guided relaxation apps or calming music helpful during the procedure.
By using these strategies, patients can manage their anxiety better. This makes their endoscopic procedure experience more comfortable.
Special Considerations for Different Patient Populations
When doing endoscopic surgery, we must think about different patient groups. This ensures safety and success. Each group has special needs that we must meet to get the best results.
Elderly Patients
Elderly patients often have health issues like heart disease or diabetes. These can make anesthesia and recovery harder. Careful preoperative assessment is key to manage these risks. We also watch for drug interactions and adjust doses as needed.
- Check kidney function to adjust drug doses.
- Watch heart health during the surgery.
- Plan for post-surgery care.
Patients with Chronic Conditions
Those with long-term health issues like high blood pressure or lung problems need custom care plans. We look at how severe their condition is and how it affects the surgery.
- Try to improve their health before surgery if we can.
- Change anesthesia plans based on their health.
- Make sure they’re closely watched during and after surgery.
Pregnant Women
Pregnant women face special challenges during endoscopic procedures. We must protect both the mother and the baby. We carefully choose the safest anesthesia options.
- Pick anesthesia that doesn’t harm the baby.
- Watch the baby’s heart rate when needed.
- Work with obstetricians for full care.
Patients with Anxiety Disorders
For those with anxiety, good communication and pre-surgery counseling are vital. We help these patients create a comfort plan. This might include relaxation methods or calming drugs.
By understanding and meeting the unique needs of various patient groups, we make endoscopic procedures safe and effective. This tailored approach improves patient results and happiness.
Recovery After Endoscopic Surgery
Recovering from endoscopic surgery involves many steps, influenced by the sedation level. We’ll help you understand what makes the healing process smooth and safe.
Recovery Based on Sedation Level
The sedation level during surgery affects recovery. Those with conscious sedation or local anesthesia tend to recover faster. We’ll watch your vital signs closely to make sure you’re comfortable.
Here are key aspects of recovery based on sedation level:
- Faster recovery for patients under conscious sedation or local anesthesia
- Close monitoring of vital signs post-procedure
- Adjusted care based on the level of sedation used
Post-Procedure Monitoring
After surgery, we’ll keep a close eye on you in a recovery area. We’ll track your vital signs like heart rate and blood pressure. This ensures your safety and comfort.
Key aspects of post-procedure monitoring include:
- Tracking vital signs
- Assessing pain and discomfort levels
- Managing any immediate post-procedure complications
Discharge Criteria
We’ll check your condition before you go home. You must have stable vital signs and manageable pain. You should also be able to resume normal activities or get the right care at home.
Follow-up Care
Follow-up care is vital after endoscopic surgery. We’ll give you clear instructions for home care. You’ll also have follow-up appointments to check on your healing.
Key aspects of follow-up care include:
- Detailed instructions for post-procedure care at home
- Follow-up appointments to monitor healing progress
- Support for managing any concerns or complications that may arise
Conclusion
Endoscopic surgery includes many procedures, each with its own specifics. This includes the type of anesthesia used. It’s important to know your anesthesia options, whether it’s for an upper GI endoscopy, a colonoscopy, or another procedure.
There are different types of anesthesia, like general, conscious sedation, and local. Each has its own benefits and is right for different procedures and patients. Your patient experience can change a lot based on the anesthesia and your procedure.
Knowing if you’ll be awake or not during surgery is key. We talked about conscious sedation, which lets you stay somewhat aware but relaxed. The choice depends on the procedure’s complexity, patient-specific factors, and what you prefer.
Recovery is also very important. The sedation level can affect how long and how you feel during recovery. Knowing what to expect can help reduce anxiety and make the process smoother.
Being informed about endoscopic surgery, anesthesia options, and what happens before and after can help you make better choices. We suggest talking to your healthcare provider about your options and concerns. This way, you can find the best approach for your needs.
FAQ
What is endoscopic surgery?
Endoscopic surgery is a minimally invasive method. It uses a thin tube with a camera and light to see inside the body. This allows doctors to diagnose and treat many conditions using smaller cuts, which means less pain and quicker healing.
Will I be awake during endoscopic surgery?
It depends on the type of procedure and anesthesia used. Some endoscopic surgeries may keep you awake or lightly sedated, while others require general anesthesia so you’re completely asleep.
What is conscious sedation?
Conscious sedation helps you relax and feel comfortable during procedures. It’s a middle ground between being fully awake and under general anesthesia. You stay responsive to commands and are carefully monitored by the medical team.
What are the benefits of being awake during endoscopic procedures?
Being awake during an endoscopic procedure can lead to faster recovery and fewer risks from anesthesia. It allows you to follow instructions during surgery, can make the process more efficient, and may lower overall costs.
How is pain managed during awake endoscopic procedures?
Pain management involves using local anesthesia, sedation, or both. Your medical team will discuss the best options to ensure you stay comfortable and pain-free during the procedure.
Can I choose to be awake or asleep during endoscopic surgery?
Your choice depends on the type of surgery, your overall health, and your anesthesiologist’s recommendation. It’s best to talk to your healthcare provider to determine what’s safest and most suitable for you.
What should I expect during recovery from endoscopic surgery?
Recovery varies depending on the procedure and anesthesia used. After surgery, you’ll be monitored for a short time before being discharged. Following your doctor’s post-operative instructions will help you recover quickly and safely.
Are there any special considerations for different patient populations undergoing endoscopic procedures?
Yes. Certain groups, like older adults, children, or pregnant women, may need special care and monitoring. The healthcare team will customize a plan to ensure maximum safety and comfort for each patient.
How can I manage anxiety about being awake during endoscopic procedures?
You can manage anxiety with pre-medication, relaxation techniques, and open communication with the medical team. Discuss your concerns beforehand so your provider can help you feel calm and prepared.
What are the risks associated with being awake during endoscopic surgery?
While generally safe, awake endoscopic surgery can cause mild discomfort or anxiety. Rarely, complications may occur. Your medical team will explain the risks and ensure you’re comfortable and well-informed.
Can I ask questions or communicate with the medical team during an awake endoscopic procedure?
Yes, communication is encouraged during awake procedures. You can ask questions or share concerns at any time to ensure your safety and comfort throughout the surgery.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/39678080/