Last Updated on December 2, 2025 by Bilal Hasdemir

Awake Surgery
Imagine being awake during a complex brain operation. For many, this thought is scary. Yet, for some brain conditions, being awake is safe and needed.Get the definitive answer: is it scary to be awake during brain surgery? Understand the patient experience during awake surgery clearly.
Medical News Today says awake brain surgery is a proven treatment for many neurological disorders. It lets surgeons watch brain function live, keeping important areas safe.
The idea of being awake during such a big procedure can be scary. But, new medical tech and surgery methods make brain surgery while awake a good choice for many.
Key Takeaways
- Awake brain surgery is a safe and effective treatment for certain neurological conditions.
- The procedure allows for real-time monitoring of brain function.
- Advancements in medical technology have improved the outcomes of awake craniotomy.
- Being awake during brain surgery enables surgeons to preserve critical brain areas.
- Patients undergoing awake brain surgery often have better post-operative outcomes.
What Happens During Awake Brain Surgery

Awake craniotomy is a special surgery for the brain. It’s done while the patient is awake. A skilled team plans and performs this complex operation.
Definition and Purpose of Awake Craniotomy
Awake brain surgery, or awake craniotomy, is a procedure where surgeons operate on the brain while the patient is conscious. The main goal is to map brain functions in real-time. This ensures that important areas are not damaged during the surgery.
The main goals of awake craniotomy include:
- Removing brain tumors or lesions located near critical brain areas
- Treating epilepsy by identifying and removing the seizure focus
- Preserving vital brain functions such as speech, motor control, and sensory processing
Historical Development of the Procedure
The idea of awake craniotomy has been around for over a century. It started in the early 20th century and has grown a lot since then. Today, it uses advanced neuroimaging and neuromonitoring tools for better results.
Some key milestones in the development of awake craniotomy include:
- The introduction of local anesthesia techniques in the early 1900s
- The development of intraoperative neurophysiological monitoring in the latter half of the 20th century
- The integration of advanced imaging technologies such as functional MRI and diffusion tensor imaging
Understanding the history and current methods of awake craniotomy shows its complexity and sophistication.
Why Patients Need to Be Awake During Brain Surgery
Surgeons need patients to be awake during brain surgery. This helps them map brain functions and keep critical areas safe. They use a method called cortical mapping to do this.
Preserving Critical Brain Functions
Keeping critical brain functions safe is another reason for awake brain surgery. By mapping brain areas, surgeons can avoid harming them. This reduces the chance of neurological problems after surgery.
| Benefits of Awake Brain Surgery | Description |
| Accurate Brain Mapping | Real-time feedback from the patient allows for precise mapping of brain functions. |
| Preservation of Critical Functions | Surgeons can identify and avoid damaging essential brain areas, reducing the risk of neurological deficits. |
| Improved Surgical Outcomes | The combination of accurate mapping and preservation of critical functions leads to better overall outcomes for patients. |
The importance of being awake during brain surgery is huge. It’s a key part that makes the surgery successful. It ensures patients get the best care possible.
Medical Conditions That Require Awake Surgery
Certain medical conditions, such as brain tumors and epilepsy, need awake surgery. This ensures precise treatment and keeps important brain functions safe. Awake brain surgery lets neurosurgeons work on the brain while the patient is awake. This way, they can spot and keep safe the most important brain areas.
Brain Tumors Near Functional Areas
Brain tumors near functional areas of the brain are a big challenge for neurosurgeons. These areas handle important tasks like speech, movement, and feeling. Awake surgery lets surgeons remove tumors safely while watching the patient’s brain functions closely.
The closeness of a brain tumor to these areas decides if awake surgery is right. By keeping the patient awake, surgeons can test brain areas during surgery. This helps in removing tumors more accurately and keeps the patient’s brain safe.
Epilepsy and Other Neurological Disorders
Epilepsy surgery often needs awake brain surgery too. For those with epilepsy who don’t get better with medicine, surgery might be needed. Awake surgery helps find the seizure focus area without harming nearby brain parts.
Other neurological disorders might also benefit from awake surgery. This method is getting better, thanks to new advances in neurological surgery. The choice to use awake surgery depends on the condition, its location, and the patient’s health.
The Patient Selection Process
Choosing the right patients for awake brain surgery is very detailed. It looks at both medical and psychological factors. This careful selection is key for the surgery’s success and the patient’s experience.
Medical Criteria for Candidacy
The medical criteria focus on the brain condition’s type and location. Patients with brain tumors or lesions near critical brain areas might be chosen for awake surgery. This helps protect these important areas.
We check the patient’s overall health, including any other health issues. This helps us decide if awake brain surgery is the best choice.
Psychological Preparation and Assessment
Psychological preparation is a big part of choosing patients. We check if they can handle the stress of being awake during surgery. We also look at their mental readiness.
Patients get psychological evaluations to see if they’re right for awake surgery. We check their anxiety levels, how well they understand the procedure, and if they can follow instructions during surgery.
We also get them ready by explaining everything in detail. We address their worries and reassure them. This lowers their anxiety and makes their experience better.
Before surgery, patients meet with healthcare professionals. They might get special medication to take before the operation, as Medical News Today reports. This meeting is very important for getting them ready for the surgery.
Preparing for Awake Brain Surgery
The journey to awake brain surgery starts with careful preparation. A dedicated surgical team guides you through this process. Knowing what to expect can help reduce anxiety and uncertainty.
Physical Preparation
Getting ready physically is key for awake brain surgery. You can usually keep up with your daily activities before surgery. It’s also important to take any prescribed medication unless told not to by your team. Always follow your team’s advice on medication and activity.
On surgery day, be ready for the physical aspects. Arrive at the hospital with enough time for preparation. Remove any jewelry or items that could get in the way. Wear comfortable clothes.
Mental and Emotional Preparation
Mental and emotional prep is just as important as physical prep. Knowing what to expect can greatly reduce anxiety. Don’t hesitate to ask questions or clarify any concerns.
Having a support system is also crucial. This could be family, friends, or a support group. Knowing you have people who care can offer emotional comfort.
Meeting with the Surgical Team
Meeting with the surgical team is a key part of prep. You’ll discuss your medical history, the surgery details, and any concerns. This is also when you learn about each team member’s role during surgery.
The team will give you detailed instructions on how to prepare. This includes any tests, dietary restrictions, and other preparations. They’ll also talk about post-operative care and what to expect during recovery.
By preparing physically, mentally, and emotionally, and working closely with your team, you can face awake brain surgery with more confidence and less anxiety.
The Awake Surgery Experience: Step by Step
The awake surgery experience is a detailed process. It starts with anesthesia and ends with the surgery’s completion. Knowing these steps helps patients understand what to expect.
Initial Anesthesia and Positioning
The journey begins with mild sedatives through an IV line. This helps the patient relax before surgery. The team then places the patient on the table, usually lying down or on their side.
Local anesthesia is used to numb the scalp. This is key to avoid pain during the surgery’s start. The anesthesiologist keeps a close eye on the patient’s vital signs.
The Awakening Process
After the initial steps, the patient starts to wake up. This is to ensure they can respond to the team during the surgery. The anesthesiologist manages this carefully to avoid discomfort.
The patient’s sedation is slowly reduced. They become fully awake, allowing the team to check their brain functions in real-time.
Intraoperative Testing and Monitoring
With the patient awake, the team starts testing brain functions. They do language, motor, and sensory tests. These ensure important brain areas are safe.
- Language tests to assess speech and comprehension
- Motor function tests to evaluate movement and strength
- Sensory evaluations to check for any numbness or tingling
These tests guide the surgeon. They help remove the targeted area while protecting others.
Completion of the Surgery
After the tests and surgery, the patient is sedated again. The incision is closed, and they go to the recovery room. Here, they receive post-operative care.
The surgery’s end is the start of recovery. The patient will be watched for any complications.
Comfort and safety are key during awake surgery. The team works together to make the process smooth and stress-free.
Pain Management During Awake Craniotomy
Pain management during awake craniotomy is a complex process. It uses different methods to keep patients comfortable and the surgery successful. Getting pain right is key to a good surgery outcome.
Local Anesthesia Techniques
Local anesthesia is crucial for pain control during awake craniotomy. Surgeons use local anesthesia to numb the scalp, so patients don’t feel pain. They use anesthetics like lidocaine or bupivacaine for this.
They inject the anesthetic into the scalp where they make the incision. This numbs the area, letting the team work without hurting the patient.
Conscious Sedation Options
Conscious sedation is also key for pain management in awake craniotomy. It helps patients relax and stay comfortable during the surgery.
They use sedatives like propofol, dexmedetomidine, and midazolam. The choice depends on the patient’s health, the anesthesiologist’s choice, and the surgery’s needs.
| Sedation Option | Benefits | Considerations |
| Propofol | Rapid onset, easy to titrate | Requires careful monitoring |
| Dexmedetomidine | Provides analgesia, less respiratory depression | Can cause bradycardia |
| Midazolam | Effective for anxiety, amnesia | Can cause respiratory depression |
By mixing local anesthesia with conscious sedation, the team can manage pain well. This makes the awake craniotomy procedure successful.
Is Brain Surgery Painful When Awake?
Many patients wonder if brain surgery hurts when they’re awake. The answer depends on the surgery details. Awake brain surgery, or awake craniotomy, is a complex operation. The patient stays awake during parts of the surgery.
What Patients Actually Feel
Patients usually don’t feel pain during awake brain surgery. This is because the brain tissue itself is not sensitive to pain. But, they might feel some sensations during the procedure.
Medical News Today explains, “People do not typically feel pain during awake brain surgery, as the brain tissue is not sensitive to pain. Additionally, surgeons anesthetize people before opening the skull to operate on the brain.”
“The brain is a unique organ in that it doesn’t feel pain, which is why surgeons can perform awake craniotomies with relative ease,” said a leading neurosurgeon.
Managing Discomfort During the Procedure
Even though the brain tissue is not sensitive to pain, other areas around the surgical site can be. To manage discomfort, surgeons use local anesthesia to numb the scalp before making an incision.
| Discomfort Source | Management Technique |
| Scalp Incision | Local Anesthesia |
| Brain Tissue Manipulation | Careful Surgical Technique |
| Positioning on the Operating Table | Adjustments for Comfort |
By understanding what to expect and how discomfort is managed, patients can better prepare themselves for the awake brain surgery experience.
The Psychological Experience of Being Conscious
Being awake during brain surgery can seem scary, but knowing what to expect can help. Patients who have awake brain surgery, or awake craniotomy, share many feelings. They often talk about the emotional ups and downs they face.
Common Emotional Responses
Being awake during surgery can bring out different feelings. Some feel anxious or scared, while others feel relieved and cooperative. Many patients are surprised to find the surgery isn’t as painful as they thought. They might feel some pressure or tugging instead.
Some common feelings include:
- Anxiety about being awake during the procedure
- Fear of pain or discomfort
- Relief that the surgery is progressing without major complications
- A sense of cooperation, as patients can respond to the surgical team’s requests
Coping Mechanisms During Surgery
Coping mechanisms are important for managing feelings during awake brain surgery. Pre-operative counseling and preparation help a lot. They help patients know what to expect and how to deal with it.
Some good ways to cope include:
- Deep breathing exercises to manage anxiety
- Positive self-talk and visualization techniques
- Support from family and friends during the recovery period
Using these coping strategies, patients can handle their psychological experience better. This makes the surgery less scary.
Success Stories
Many patients have seen great results from awake brain surgery. Their stories often talk about the surgery’s accuracy and the care they got after.
| Condition | Surgical Outcome | Patient Feedback |
| Brain Tumor | Successful removal | Positive |
| Epilepsy | Significant reduction in seizures | Very Satisfied |
Challenging Experiences
Not all patients have a smooth experience with awake brain surgery. These stories are important too. They show where we can do better and the need for more support.
Sharing both the good and the tough times helps us understand awake brain surgery better. This view is key for those thinking about this surgery.
Key Takeaways
- Patient experiences with awake brain surgery vary, with many reporting positive outcomes.
- The success of the surgery often depends on the precision of the surgical technique and post-operative care.
- Challenging experiences highlight the need for comprehensive patient support.
Risks and Complications of Awake Brain Surgery
It’s important for patients to know the risks of awake brain surgery. This surgery, like any other, has its own set of risks and complications. These need to be carefully looked at.
Medical Risks
One big medical risk is seizures during the surgery. Medical News Today says seizures are the main risk. Other risks include infection, bleeding, and reactions to anesthesia.
Common Medical Risks:
- Seizures during surgery
- Infection
- Bleeding or hematoma
- Reaction to local anesthesia
- Brain swelling
Psychological Impacts
The psychological effects of awake brain surgery are significant. Patients might feel anxious, scared, or uncomfortable. It’s key for the surgical team to offer emotional support.
Patients often feel anxious about being awake during surgery. But with the right support, many manage their anxiety well.
Knowing these risks helps patients and their families make better choices about treatment.
Recovery After Awake Craniotomy
Recovery after awake craniotomy is a multi-stage process. It requires careful monitoring and post-operative care. The journey starts right after surgery and goes on for weeks, aiming for full recovery.
Immediate Post-Operative Period
Right after surgery, vital signs are watched for two hours in a post-anesthesia care unit. Then, people usually stay in a high-dependency ward or ICU. Close monitoring is key to handle any immediate issues and manage pain well.
Patients are closely watched to make sure they’re recovering as they should. This includes checking for any neurological deficits or complications. The medical team also manages pain with various medications and other methods.
Short-term Recovery Timeline
The short-term recovery timeline varies based on health and surgery complexity. Patients usually spend several days in the hospital. They start physical therapy to regain strength and mobility.
After leaving the hospital, patients recover at home. They need to rest, take their meds, and keep up with doctor’s appointments. Having a support system is crucial for daily help during this time.
Long-term Healing Process
The long-term healing process takes weeks to months. Patients should avoid hard activities and live a healthy lifestyle. Regular check-ups with their healthcare team are vital to track progress and address concerns.
In this phase, patients might notice cognitive changes or emotional shifts, which are usually temporary. The healthcare team offers advice on managing these effects and supporting overall well-being. With the right care and following post-operative instructions, most patients can fully recover and get back to their normal lives.
Success Rates and Outcomes
The success of awake brain surgery shows how far neurosurgery has come. We’ve seen big improvements in patient care and surgery techniques. This has led to better results overall.
A 2021 study looked at 469 people who had awake craniotomy. Only 1.7% had permanent side effects after surgery. This shows the positive outcomes of this procedure.
Statistical Success Rates
Statistical success rates tell us how well awake brain surgery works. We look at things like how many surgeries are successful, complication rates, and how long patients take to recover. The data shows awake brain surgery is very effective, with many patients seeing their quality of life improve after surgery.
- High success rate in removing brain tumors near functional areas
- Low rate of permanent complications
- Improved patient outcomes due to real-time monitoring during surgery
Quality of Life After Surgery
The quality of life after awake brain surgery is very important. Many patients see a big improvement in their well-being after the surgery. Being awake during surgery helps doctors map brain functions more accurately. This means they can better preserve important brain areas.
Patients often get back to their normal activities faster after awake brain surgery. They also have a lower risk of long-term problems with thinking or moving. This is because the surgery focuses on removing the right brain area while keeping healthy tissue safe.
Alternatives to Awake Surgery
Awake brain surgery works for many, but it’s not for everyone. The choice depends on health, tumor location, and staying calm during surgery.
Doctors look at each case to pick the best surgery. Some prefer traditional surgery under general anesthesia. Others might like new, less invasive methods.
When Traditional Surgery is Preferred
General anesthesia is often chosen for hard-to-reach tumors or when awake surgery isn’t possible. It lets the team work without the patient’s feedback.
Traditional surgery is best for:
- Tumors deep in the brain
- Patients with severe anxiety or can’t stay still
- Cases where tumors are close to important brain parts
A neurosurgeon says, “Choosing between awake and traditional surgery depends on many factors. This includes the patient’s health and the tumor’s details.” This shows how important a tailored treatment plan is in neurosurgery.
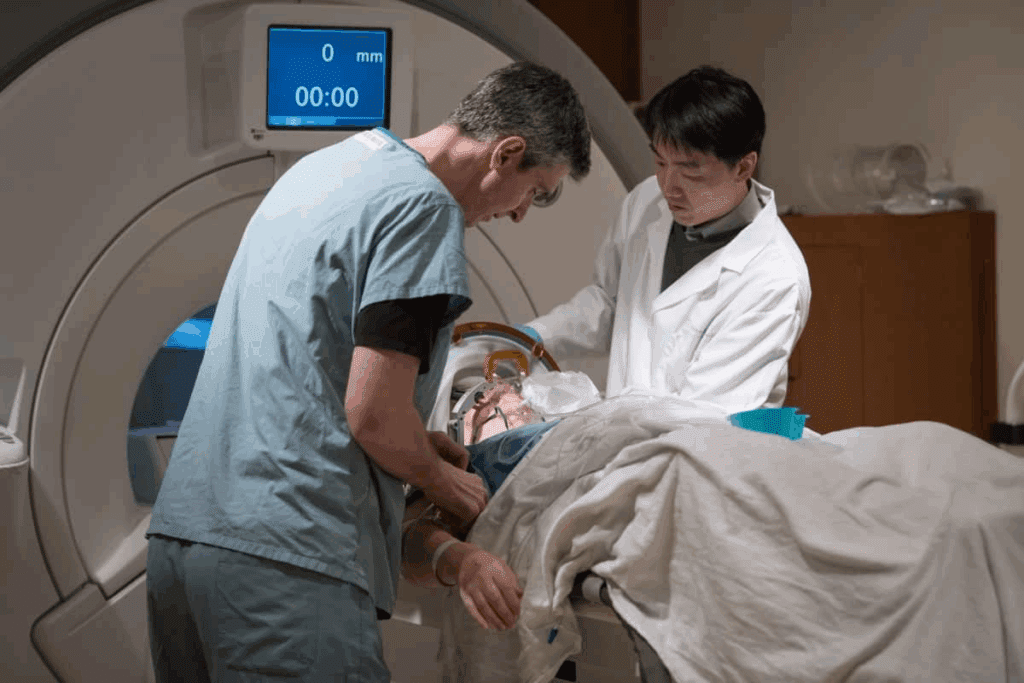
Emerging Minimally Invasive Techniques
New, less invasive brain surgery methods are changing the game. They include laser ablation, stereotactic radiosurgery, and endoscopic surgery. These methods aim to reduce recovery time and risks.
Laser ablation uses MRI to target and kill tumor cells with heat. It’s great for tumors hard to reach with traditional surgery.
The field of neurosurgery is always growing. New technologies and techniques are being researched. This could lead to even more safe and effective treatments in the future.
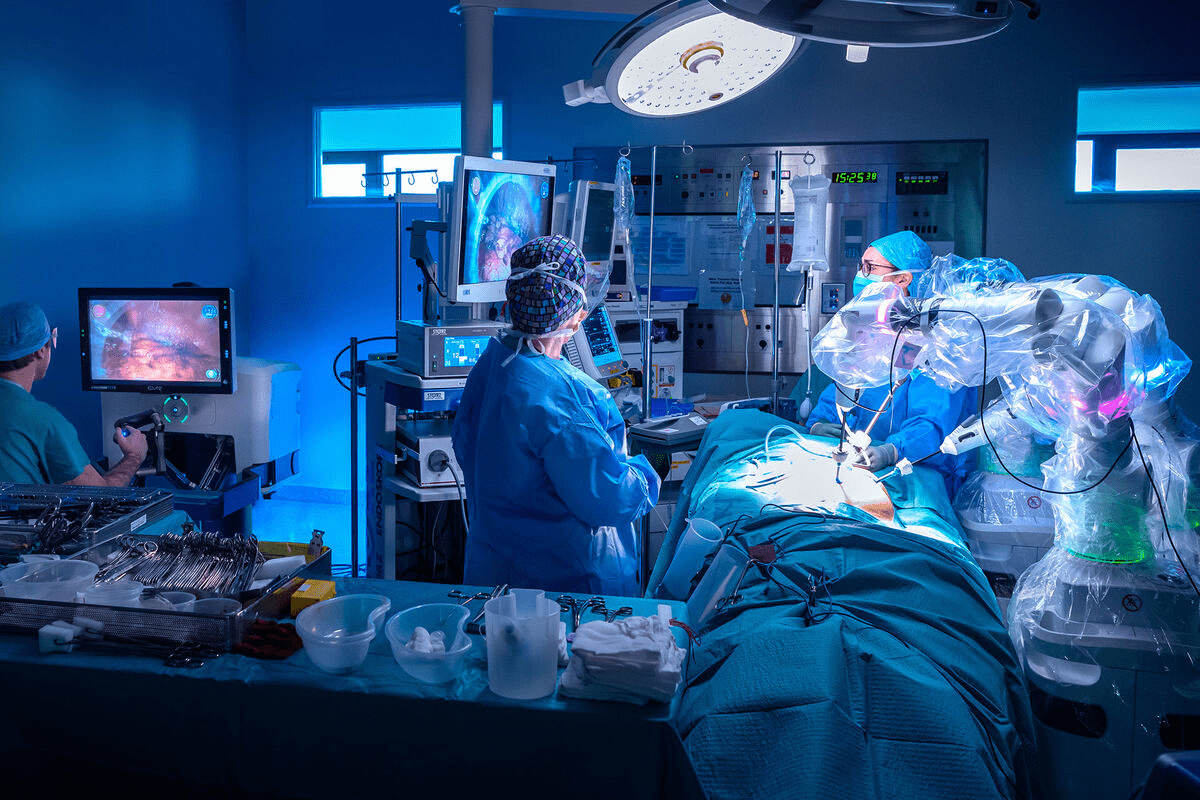
Advancements in Awake Brain Surgery Techniques
The field of neurosurgery has seen big changes in awake brain surgery. These changes have made surgeries better and more precise. Medical technology keeps getting better, changing how awake craniotomies are done.
Technological Innovations
Technology has been key in improving awake brain surgery. Intraoperative MRI and CT scans are big advancements. They let surgeons see the brain in real-time during surgery.
This technology helps in removing tumors more accurately. It also helps in keeping important brain functions safe.
Key technological advancements include:
- Intraoperative imaging techniques
- Advanced brain mapping technologies
- Robot-assisted surgery systems
These technologies have made awake brain surgeries more accurate and safe. For example, brain mapping helps find important brain areas. This lets surgeons work on complex neural structures more precisely.
“Awake craniotomies increase the margin of safety of resecting brain tumors,” allowing for more precise surgeries.
Improved Patient Comfort Measures
There’s also a big push to make patients more comfortable during awake brain surgery. New local anesthesia and conscious sedation options are being developed. These help reduce discomfort and anxiety for patients.
Some of the measures to enhance patient comfort include:
- Personalized anesthesia plans tailored to individual patient needs
- Advanced pain management strategies
- Psychological support and counseling before, during, and after surgery
By combining these comfort measures with advanced surgical techniques, we can make the patient experience better. This is crucial for awake brain surgery.
As we keep improving, our main goal is to give the best care. We aim for the best outcomes for patients having awake craniotomy procedures.
Conclusion: Balancing Fear with Medical Necessity
Awake brain surgery, or awake craniotomy, is a complex procedure that can make patients nervous. Yet, it’s a crucial treatment for many, allowing surgeons to work on the brain while keeping important functions intact.
We’ve looked into awake brain surgery, from what it is and its history to the medical needs it serves. Understanding how it works and who it helps shows its importance. This knowledge helps us see why awake brain surgery is sometimes necessary.
Fear is normal when thinking about brain surgery while awake. But the benefits of this surgery are huge. By weighing fear against medical need, patients can choose the best treatment for them. As medical tech gets better, so will the results of awake brain surgery.
Awake brain surgery shows how far medical science has come. It’s a key part of helping many people. By learning about it and its benefits, we can help reduce the fear it causes. This makes the experience better for those having awake craniotomy.
FAQ
What is awake brain surgery?
Awake brain surgery, also known as awake craniotomy, is a procedure where the patient stays awake. This lets the surgical team watch the brain’s function in real-time. It helps them avoid damaging important areas.
Why is it necessary to be awake during brain surgery?
Being awake is key for surgeries that affect brain areas controlling speech, movement, or sensation. It lets the team map brain functions and avoid damage.
Is brain surgery painful when you’re awake?
The brain itself doesn’t feel pain because it lacks pain receptors. But, the scalp and other tissues are numbed with local anesthesia. This makes the surgery less uncomfortable. Some patients might feel pressure or vibrations, but these are usually manageable.
How is pain managed during awake craniotomy?
Pain is managed with local anesthesia to numb the scalp and surgery areas. Conscious sedation may also be used to help the patient relax and reduce anxiety.
What are the risks and complications of awake brain surgery?
Risks include infection, bleeding, stroke, seizures, and reactions to anesthesia. There can also be psychological impacts like anxiety or stress from being awake during the surgery.
How long does awake brain surgery take?
The time needed for awake brain surgery varies. It depends on the procedure’s complexity, the condition being treated, and the patient’s needs. It can last from a few hours to several hours.
What is the recovery process like after awake brain surgery?
After surgery, the patient is closely watched for complications. The recovery time can vary, but most are discharged within a few days. Healing fully can take weeks to months.
Are there alternatives to awake brain surgery?
Yes, alternatives include traditional surgery under general anesthesia and newer, minimally invasive techniques. The choice depends on the patient’s condition and the brain lesion’s location and nature.
How successful is awake brain surgery?
Awake brain surgery has high success rates in removing lesions while preserving brain functions. Success rates vary based on the condition and the patient’s situation.
What advancements have been made in awake brain surgery techniques?
Advances include better imaging and mapping technologies and improved patient comfort measures. These have led to better outcomes and a more comfortable experience for patients.
How do patients prepare for awake brain surgery?
Preparation involves physical, mental, and emotional readiness. Patients undergo assessments and consultations with their team to ensure they’re ready.
What is the psychological experience like for patients during awake brain surgery?
Patients’ experiences vary. Some feel anxious or stressed, while others are more relaxed. Support from the team is key in managing the psychological aspects.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8072195/