Last Updated on December 2, 2025 by Bilal Hasdemir
Awake brain surgery, also known as awake craniotomy, is a complex procedure. Surgeons operate on the brain while the patient is awake. This method is key for treating conditions like brain tumors and epilepsy. It allows for precise mapping of brain functions.Learn how common awake brain surgery is. Understand the percentage of cases where an awake surgery approach is necessary clearly.
According to various sources, awake brain surgery is used to treat some brain conditions. It’s a significant treatment option in modern medicine. We are seeing a growing reliance on this technique. It’s effective in minimizing neurological damage.
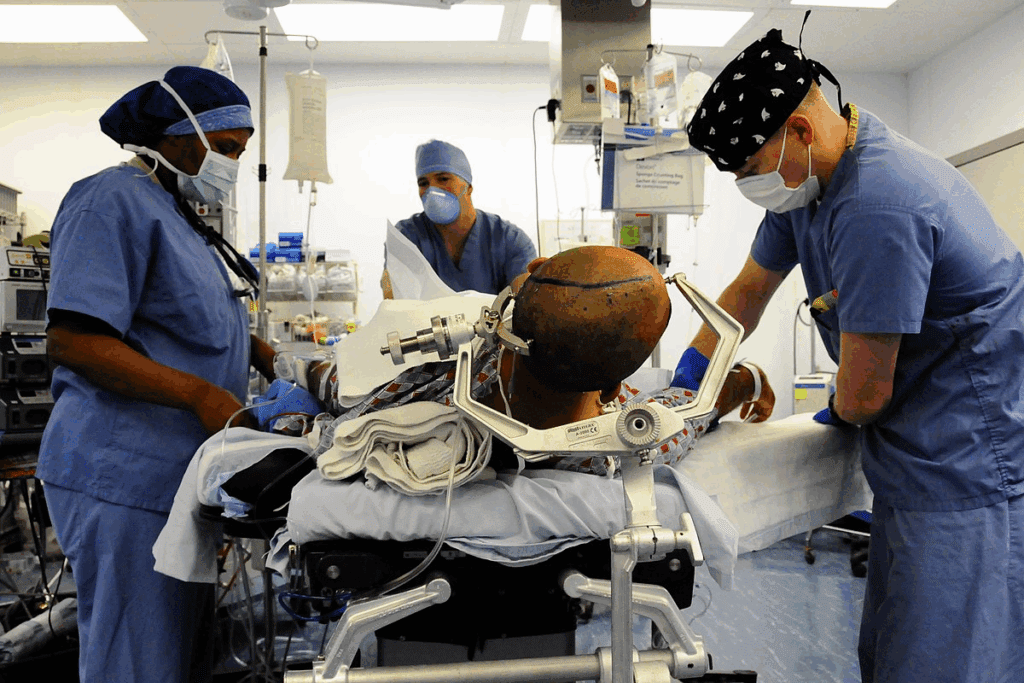
awake surgery
As medical technology advances, the use of brain operation on awake procedures is increasing. This offers new hope to patients with previously inoperable conditions.
Key Takeaways
- Awake brain surgery is a complex procedure used to treat brain conditions like tumors and epilepsy.
- This technique allows for precise mapping of brain functions, minimizing neurological damage.
- The prevalence of awake brain surgery is increasing due to advancements in medical technology.
- It offers new hope to patients with previously inoperable brain conditions.
- Awake craniotomy is a significant treatment option in modern medicine.
Understanding Awake Brain Surgery

Awake brain surgery is a cutting-edge neurosurgical method. It has changed how we treat brain diseases. The surgery involves taking out a part of the skull to reach the brain. The patient stays awake during this time.
Definition and Basic Concept
Awake brain surgery, or awake craniotomy, is a complex surgical procedure. The patient is awake and can talk during the surgery. This lets neurosurgeons map the brain. They make sure important brain functions are not harmed.
The main idea is to have the patient help during surgery. Being awake, patients can do tasks. These tasks help surgeons avoid areas of the brain that control important things like speech and movement.
Historical Development of the Procedure
The history of awake brain surgery goes back many years. At first, it was used only in a few cases. But, thanks to better anesthesia and surgery methods, it’s now used more often.
| Year | Milestone | Description |
| Early 20th Century | First recorded awake craniotomies | Initial attempts at performing brain surgery with patients awake. |
| 1960s | Advancements in anesthesia | Introduction of local anesthesia allowed for more complex procedures. |
| 1990s-Present | Modern techniques and technology | Integration of advanced imaging and brain mapping techniques. |
Today, awake brain surgery is a refined and sophisticated procedure. It gives hope to those with complex brain issues. The growth of this method shows how far neurosurgery has come. It also shows the dedication to bettering patient care.
Prevalence of Awake Surgery in Modern Medicine
Awake brain surgery is becoming more common worldwide. Medical technology and surgical techniques are improving. This has led to more awake craniotomies, changing how we do neurosurgery.
The trend towards awake brain surgeries is growing. It’s because we need more precise and safe procedures. New data shows awake craniotomies are beneficial.
Global Statistics on Awake Craniotomies
Statistics on awake craniotomies vary globally. This is due to differences in healthcare, surgery, and patients. Studies show awake craniotomies are being done more often worldwide.
- A 2021 study found 1.7% of awake craniotomy patients had permanent side effects. This shows a low complication rate.
- The frequency of awake brain surgery varies by region and country. It depends on skilled neurosurgeons and medical facilities.
Frequency in the United States
In the U.S., awake craniotomies are becoming more common. They are used to treat brain tumors and epilepsy. This is especially true in specialized neurosurgical centers.
- Research supports the safety and effectiveness of awake brain surgery in the U.S.
- Major neurosurgical centers are adopting awake craniotomy procedures. This is increasing their frequency.
As we learn more about awake brain surgery, its use will likely grow. This is thanks to better medical technology and surgical techniques.
Medical Conditions That May Require Awake Brain Surgery
Several neurological conditions may need awake brain surgery for the best results. This surgery is key when the affected area is close to important brain functions. It lets surgeons treat the condition while keeping these functions safe.
Brain Tumors and Awake Procedures
Brain tumors, whether they are benign or malignant, can be treated with awake brain surgery. This method is very useful when the tumor is near areas that control vital functions like speech, movement, or sensation. By keeping the patient awake, surgeons can watch the patient’s brain responses in real-time. This reduces the chance of damaging important brain areas.
Benefits of Awake Surgery for Brain Tumors:
- Preservation of critical brain functions
- Real-time neurological assessment
- Potential for more precise tumor removal
Epilepsy Treatment
Awake brain surgery is also used for certain types of epilepsy. For patients whose epilepsy doesn’t respond to medication, surgery might be needed to remove the seizure focus. Awake surgery lets the team map the brain’s function and find the seizure areas. This ensures that removing the seizure focus doesn’t harm other important brain functions.
Other Neurological Conditions
Other neurological conditions, like vascular malformations and certain movement disorders, may also need awake brain surgery. The choice to use awake brain surgery depends on the condition’s location, nature, and the patient’s health.
Here is a summary of the medical conditions that may require awake brain surgery:
| Condition | Description | Role of Awake Surgery |
| Brain Tumors | Benign or malignant growths in the brain | Precise removal while preserving critical brain functions |
| Epilepsy | Seizure disorder resistant to medication | Mapping and removal of seizure focus |
| Vascular Malformations | Abnormal formations of blood vessels in the brain | Precise treatment to avoid damage to surrounding brain tissue |
Understanding the medical conditions that may need awake brain surgery helps patients and their families. Awake brain surgery is a complex and advanced way to treat brain conditions. It offers the chance for better outcomes and a better quality of life.
Why Patients Need to Be Awake During Brain Surgery
Awake brain surgery is now a key procedure. It lets surgeons map brain functions accurately. This is vital for keeping important brain areas safe during surgery.
Functional Mapping of the Brain
Functional brain mapping finds brain areas for things like speech and movement. Keeping patients awake lets surgeons interact with them, mapping these areas precisely. This is key for knowing which areas to keep safe during surgery.
Patients do tasks like naming objects or moving limbs. The surgeon watches their brain activity. This feedback helps create a detailed brain map.
Real-time Neurological Assessment
Neurological checks during surgery let surgeons see how the brain is working. This is crucial for making quick changes if needed.
| Assessment Type | Description | Importance |
| Motor Function | Evaluating the patient’s ability to move limbs or perform specific motor tasks. | Ensures preservation of motor skills post-surgery. |
| Speech and Language | Assessing the patient’s ability to speak, understand language, and perform tasks like naming objects. | Critical for maintaining communication skills. |
| Sensory Function | Testing the patient’s sensory perception, such as feeling touch or temperature. | Important for preserving sensory capabilities. |
These checks in real-time help surgeons avoid problems after surgery. Being able to change the surgery plan based on feedback is a big plus of awake brain surgery.
The Awake Craniotomy Procedure Explained
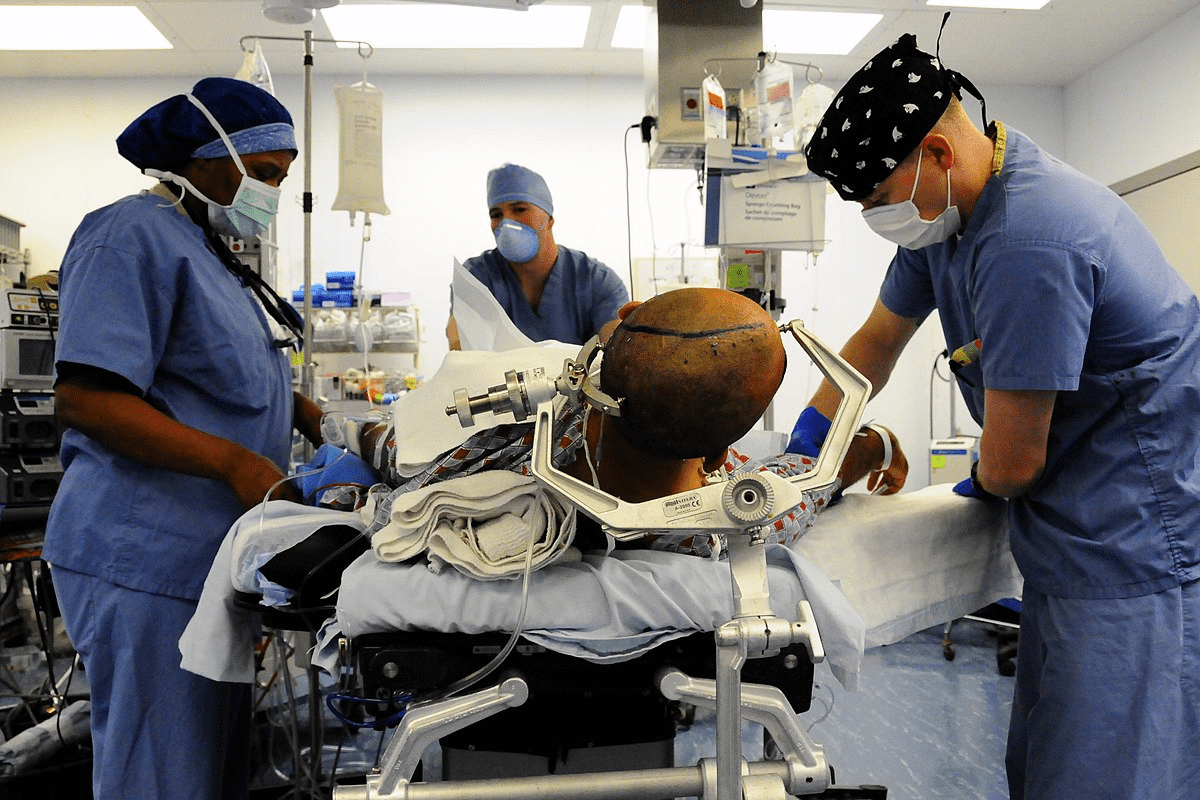
The awake craniotomy process is complex. It involves getting ready, using special anesthesia, and watching the patient closely during surgery. A team of experts, including neurosurgeons, anesthesiologists, and nurses, work together.
Pre-surgical Preparation
Getting ready for surgery is key. Patients get a full check-up, including their medical history and scans like MRI or CT. This helps the team plan the surgery.
On surgery day, patients follow special instructions. They learn about the surgery and how to stay calm. The team explains everything to make the patient feel at ease.
Anesthesia Techniques Used
Anesthesia is vital in awake craniotomy. The chosen method keeps patients comfortable but awake enough for checks. It’s a mix of local anesthesia and sedation.
Local anesthesia numbs the scalp and incision area. Sedation helps patients relax at first. The sedation level is adjusted to keep them calm and responsive.
Intraoperative Patient Monitoring
Keeping an eye on the patient’s brain is crucial. Techniques like EEG and direct stimulation check brain function live.
The team watches how the patient reacts to things. This feedback is key for protecting brain functions and getting good results.
Patient Selection Criteria for Awake Surgery
The success of awake brain surgery depends on picking the right patients. We carefully check each patient to see if they’re a good fit for this surgery.
Contraindications and Limitations
While awake brain surgery has many benefits, there are some things that make it not suitable. Patients with severe anxiety or those who are unable to cooperate during the procedure may not be good candidates. Also, people with serious medical problems or who are not stable enough for surgery are not good candidates.
The Patient Experience During Awake Surgery
Being awake during brain surgery is a unique experience. It involves careful monitoring and talking with the surgical team. Patients often wonder what they will feel and hear. Knowing this can help reduce their anxiety.
What Patients Can Feel and Hear
During awake brain surgery, patients are usually awake and can talk to the team. We make sure patients are comfortable and relaxed with the right anesthesia and monitoring. They might feel some discomfort, but they usually don’t feel pain.
Patients might hear the sounds of surgical tools and the voices of the team. Clear communication is kept up throughout to keep the patient informed and involved. This is key for the surgery’s success, as it lets the team check the patient’s brain functions in real-time.
Communication with the Surgical Team
Good communication between the patient and the team is vital in awake brain surgery. Patients are encouraged to share any discomfort or worries they have. This open communication helps the team make the right changes and keeps the patient safe and comfortable.
| Aspect of Surgery | Patient Experience | Surgical Team’s Role |
| Sensation | May feel some discomfort, generally no pain | Administer appropriate anesthesia |
| Communication | Respond to requests, report discomfort | Maintain clear and continuous communication |
| Monitoring | Undergo continuous neurological assessment | Monitor neurological functions, adjust as necessary |
Knowing what to expect during awake brain surgery helps patients prepare. Our team is committed to giving full care and support from start to finish.
Psychological Aspects and Preparation
Getting patients ready for awake brain surgery is key. It’s not just the surgical team. It’s also about taking care of their mental and emotional health.
Mental Preparation Before Surgery
It’s important for patients to prepare mentally for awake brain surgery. We start by teaching them about the surgery. This includes what they’ll go through during and after.
We make sure they know the risks, benefits, and other options. This helps them make informed decisions.
Patients are encouraged to talk about their fears and worries. This way, we can offer support and help ease their stress and anxiety.
Key aspects of mental preparation include:
- Understanding the surgical process
- Managing expectations and fears
- Establishing a support network
Psychological Support During and After Surgery
Psychological support doesn’t stop before surgery. It’s there during and after too. During surgery, patients might feel anxious or uncomfortable. Our team is ready to offer comfort and reassurance.
After surgery, patients might feel a mix of emotions. Our team is there to support them, addressing any concerns or worries they have.
“The psychological support provided to patients undergoing awake brain surgery is just as important as the surgical procedure itself. It’s about ensuring that patients are cared for holistically, addressing their emotional and psychological needs alongside their medical needs.”
To show the support we offer, let’s look at a table:
| Stage | Support Provided |
| Pre-Surgical | Education, anxiety management, establishing support networks |
| During Surgery | Reassurance, comfort measures, continuous monitoring |
| Post-Surgical | Ongoing emotional support, addressing recovery concerns, rehabilitation guidance |
By offering full psychological support, we can make sure patients do well. And we can make their surgery experience better.
Recovery and Rehabilitation After Awake Brain Surgery
The path to full recovery after awake brain surgery is complex. It includes both immediate care and long-term rehabilitation. We focus on providing full support and monitoring to help patients achieve the best results.
Immediate Post-Operative Period
Right after surgery, patients stay in a special care unit. Post-operative care is key to avoiding complications and making the recovery smoother.
Important parts of immediate care are:
- Watching the patient’s brain function closely
- Managing pain and discomfort
- Looking out for any complications
We also give patients clear guidance on what to expect and how to manage their recovery well.
Long-term Rehabilitation Process
The long-term rehabilitation process is customized for each patient. It aims to help them regain lost abilities and improve their quality of life. This might include physical, occupational, and speech therapy.
| Therapy Type | Focus | Goals |
| Physical Therapy | Motor function and mobility | Regaining strength and coordination |
| Occupational Therapy | Daily living activities | Independence in daily tasks |
| Speech Therapy | Communication skills | Improving speech clarity and comprehension |
In the rehabilitation journey, we team up with patients and their families. We set achievable goals and celebrate every step forward. This ensures our care is both thorough and caring.
Success Rates and Outcomes of Awake Brain Surgeries
Awake brain surgery is proving to be very effective. Many studies show its success rates. We look into how well this complex surgery works and its benefits for patients.
Statistical Analysis of Results
Research shows awake brain surgery leads to good results. A big number of patients see their brain function improve or stay the same. This makes the surgery safe and effective for treating brain issues.
For example, a study on awake craniotomies for brain tumors found over 90% of patients did well. They either got better or stayed the same after surgery. These numbers highlight the surgery’s success.
| Outcome | Percentage of Patients |
| Improved Neurological Function | 55% |
| Unchanged Neurological Function | 35% |
| Deteriorated Neurological Function | 10% |
Long-term Patient Outcomes
Studies on patients after awake brain surgery show good long-term results. Many patients keep improving, leading to a better life quality.
Being able to map brain functions during surgery makes it more precise. This is key for surgeries near important brain areas like speech and motor control.
The success of awake brain surgery comes from advanced techniques, careful patient choice, and good care after surgery. As we keep improving, we expect even better results for patients.
Risks and Complications of Awake Surgery
It’s important for patients to know the risks of awake brain surgery. This surgery has many benefits, like less chance of brain damage in some cases. But, it also has risks that need careful management.
Common Complications
Awake brain surgery can cause several complications. These are common in many surgeries. Here are some:
- Seizures: Seizures are a big risk during awake brain surgery. They can happen because of the surgery or the patient’s health.
- Infection: There’s a chance of infection with any surgery, including awake brain surgery. Doctors use antibiotics and follow strict cleanliness rules to lower this risk.
- Neurological Deficits: Patients might face neurological problems after surgery. These can be mild or severe and might last a short time or forever.
Management of Intraoperative Emergencies
Handling emergencies during surgery is key in awake brain surgery. Surgeons and anesthesiologists are trained to deal with sudden problems. They focus on:
- Rapid Response: The team must act fast in emergencies.
- Monitoring: Keeping a close eye on the patient’s health and brain function is vital.
- Communication: It’s important for the patient and the team to talk clearly, especially during awake surgeries.
| Complication | Description | Management |
| Seizures | Triggered by the surgical procedure or patient’s condition | Administering antiepileptic drugs, adjusting surgical technique |
| Infection | Risk associated with any surgical procedure | Use of antibiotics, sterile surgical techniques |
| Neurological Deficits | Range from mild to severe, can be temporary or permanent | Careful preoperative planning, intraoperative monitoring, postoperative rehabilitation |
Specialized Centers and Surgeons for Awake Brain Procedures
Choosing the right neurosurgical center and surgeon is key for awake brain surgery success. Specialized centers and experienced neurosurgeons are crucial for good outcomes.
Leading Neurosurgical Centers in the United States
The United States has many top neurosurgical centers for awake brain procedures. These places have the latest technology and expert teams. Some of the best include:
- Medical organization
- Johns Hopkins Hospital
- University of California, Los Angeles (UCLA) Medical Center
- NewYork-Presbyterian Hospital
- Medical organization
These centers are known for their excellent neurosurgery care. They offer full support for awake brain surgery patients.
Finding Experienced Neurosurgeons
Finding a skilled neurosurgeon is vital for awake brain surgery. Here are tips for patients:
- Check Credentials: Make sure the neurosurgeon is board-certified and has the right training for awake brain procedures.
- Review Patient Outcomes: Look at patient results and complication rates. This shows the surgeon’s skill.
- Seek Referrals: Ask your doctor or other healthcare workers for recommendations. They can suggest good neurosurgeons.
- Consult Multiple Surgeons: Talking to several neurosurgeons can help you compare their methods and advice.
By following these steps, patients can boost their chances of a successful awake brain surgery.
Conclusion
Awake brain surgery is a top-notch treatment for many brain issues. It’s precise and safe, thanks to skilled doctors. This surgery uses special techniques, advanced anesthesia, and checks on the brain in real-time.
This surgery is key for treating brain tumors and epilepsy. It helps keep important brain functions working. By looking at the main points of this surgery, we see its big role in today’s medicine.
Awake brain surgery is a big step forward in brain surgery. It gives patients with certain brain problems a safe and effective treatment. As we keep improving, the work of expert neurosurgeons and special centers will be more important than ever.
FAQ
What is awake brain surgery?
Awake brain surgery, also known as awake craniotomy, is a procedure where the patient stays awake. Surgeons operate on the brain while the patient is awake. This method is used for treating conditions like brain tumors and epilepsy. It allows for precise mapping of brain functions.
Is awake brain surgery painful?
No, awake brain surgery is not painful. The scalp is numbed with local anesthesia. Patients are usually comfortable during the procedure. Some may feel minor discomfort or pressure, but it’s manageable.
How common is awake brain surgery?
Awake brain surgery is not very common. But, it’s becoming more common as more surgeons learn the technique. The exact number of times it’s done varies globally. It’s more common in specialized neurosurgical centers.
What conditions are treated with awake brain surgery?
This surgery is used for various neurological conditions. These include brain tumors, epilepsy, and other disorders. It helps surgeons identify and preserve critical brain areas.
Why do patients need to be awake during brain surgery?
Patients are kept awake to map brain functions and assess them in real-time. This helps surgeons identify and avoid damaging critical areas. It ensures the best possible outcomes.
What is the success rate of awake brain surgery?
The success rate varies based on the condition and the patient. Generally, it has a high success rate in preserving brain function. It often achieves the desired surgical outcome.
What are the risks and complications of awake surgery?
Awake brain surgery carries risks like infection, bleeding, and neurological deficits. However, these risks are low. The procedure is safe when done by experienced surgeons.
How are patients selected for awake surgery?
Patients are chosen based on their condition, health, and ability to cooperate. Ideal candidates benefit from the precise mapping awake surgery provides.
What is the recovery process like after awake brain surgery?
Recovery involves close monitoring in the post-anesthesia care unit and a hospital stay. Patients need rest and may feel some discomfort. Most can return to normal activities in a few weeks.
How can I find an experienced neurosurgeon for awake brain surgery?
To find a skilled neurosurgeon, ask your doctor for referrals or research online. Contact leading neurosurgical centers directly. Make sure to ask about their experience and success rates.
What is the role of psychological support during awake surgery?
Psychological support is key during awake surgery. It helps patients deal with the stress and anxiety. Our team provides emotional support and guidance to ensure patients are comfortable and informed.
Are there any alternatives to awake brain surgery?
There may be alternatives like traditional surgery under general anesthesia or other treatments. The best option depends on the patient’s condition and needs.
References
JAMA Network. Evidence-Based Medical Insight. Retrieved from https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2814234





