Last Updated on November 25, 2025 by Ugurkan Demir

At Liv Hospital, we know how vital it is to spot early signs of heart attack or stroke. Pain in the back side of the heart is a warning sign that should not be ignored.
Feeling discomfort or pain in this area could mean a serious medical issue. We aim to offer top-notch healthcare. We also provide full support for international patients, ensuring they get the help they need quickly.
It’s key to know the early signs of heart attack or stroke to get treatment fast and avoid lasting harm. Our team is all about patient-focused care. We meet each person’s unique needs.
Key Takeaways
- Recognizing pain in the back side of the heart as a possible sign of heart attack or stroke.
- Understanding the importance of quick medical help.
- Liv Hospital’s dedication to international excellence and patient-centered care.
- The importance of early warning signs for heart attack and stroke.
- Comprehensive support for international patients.
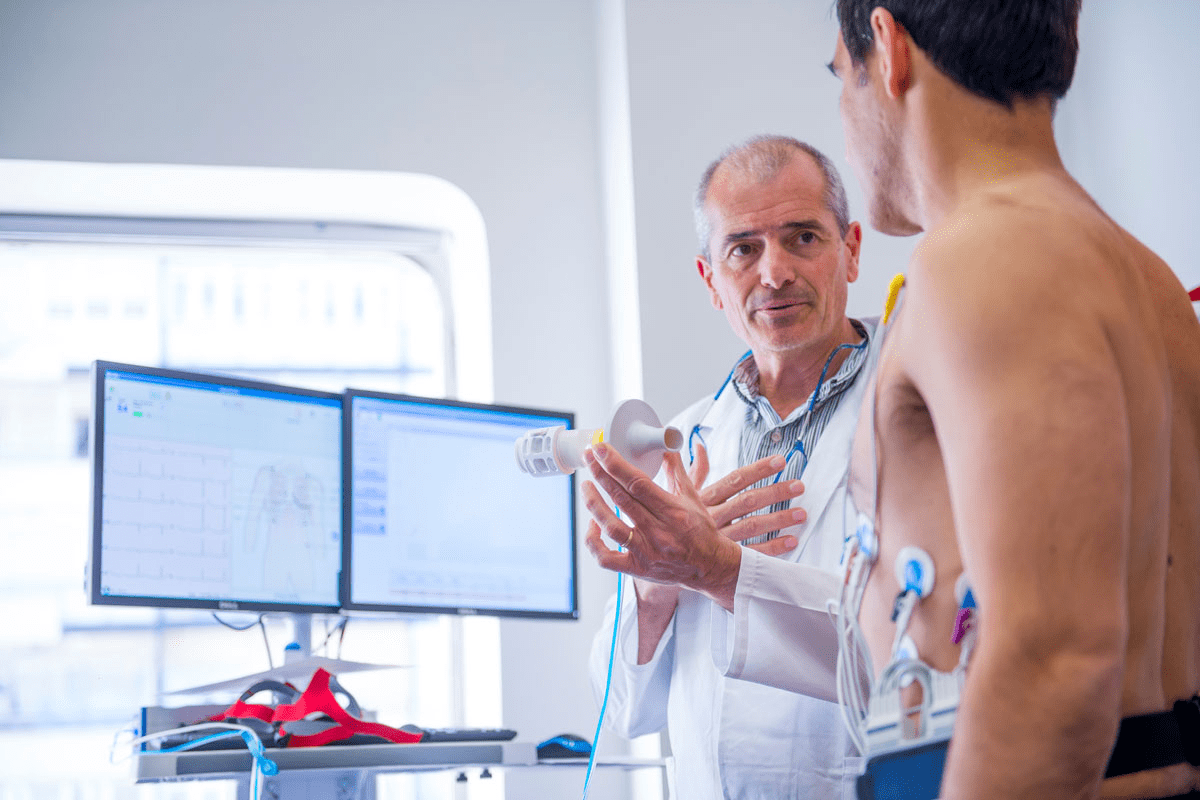
Understanding Cardiovascular Emergencies

It’s key to know the difference between heart attacks and strokes. Both are emergencies that need quick action. They affect different parts of the body and show different signs.
The Difference Between Heart Attacks and Strokes
A heart attack happens when blood flow to the heart stops. This causes damage to the heart muscle. It’s usually because of a blood clot on atherosclerosis in a coronary artery.
Symptoms include chest pain, feeling weak, and pain in the arms or shoulder.
A stroke occurs when blood flow to the brain is cut off. This prevents brain cells from getting oxygen and nutrients. Symptoms include sudden numbness, weakness, and trouble speaking.
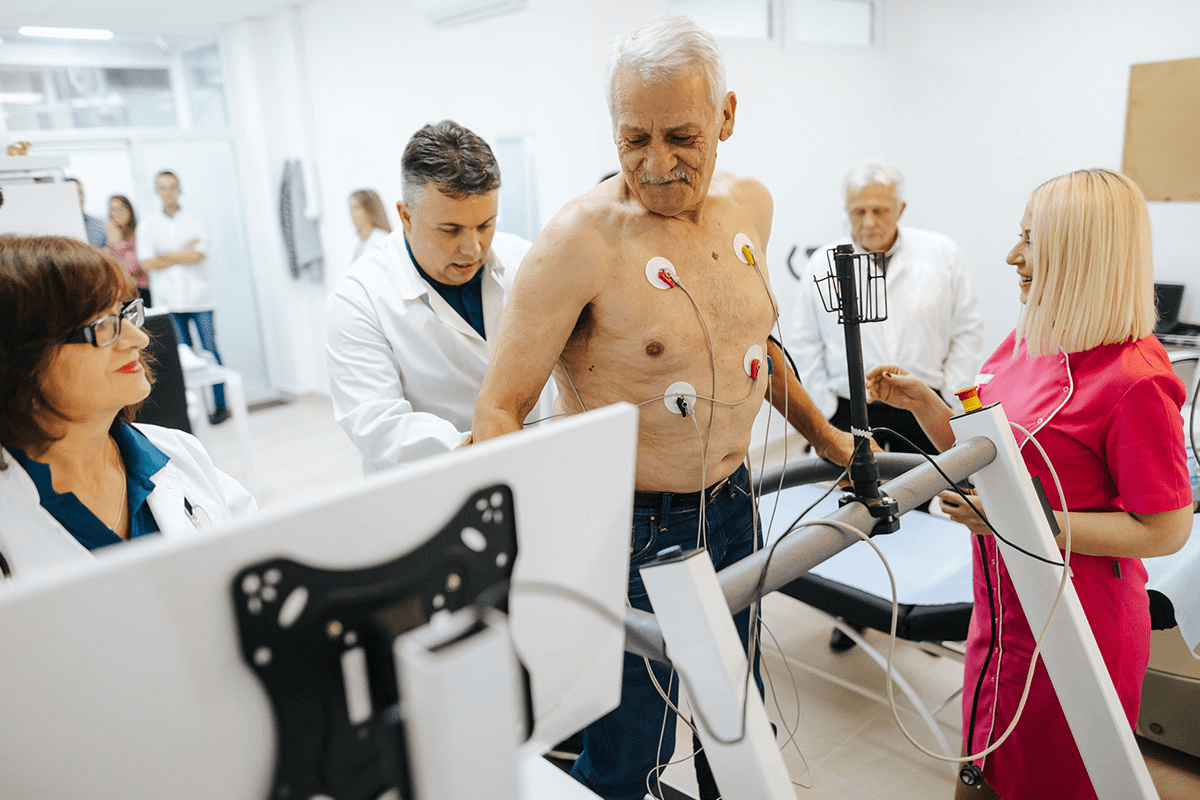
Why Minutes Matter in Treatment
Quick treatment for heart attacks and strokes is vital. The sooner treatment starts, the better the outcome. For heart attacks, it can lessen heart damage. For strokes, it can reduce brain damage and improve recovery.
| Condition | Cause | Symptoms | Importance of Timely Treatment |
| Heart Attack | Blockage of blood flow to the heart | Chest pain, weakness, pain in arms or shoulder | Reduces heart damage |
| Stroke (CVA) | Interruption or reduction of blood supply to the brain | Numbness, confusion, trouble speaking | Reduces brain damage, improves recovery |
Knowing the signs of these emergencies and acting fast can save lives. It’s vital to recognize symptoms and seek medical help immediately.
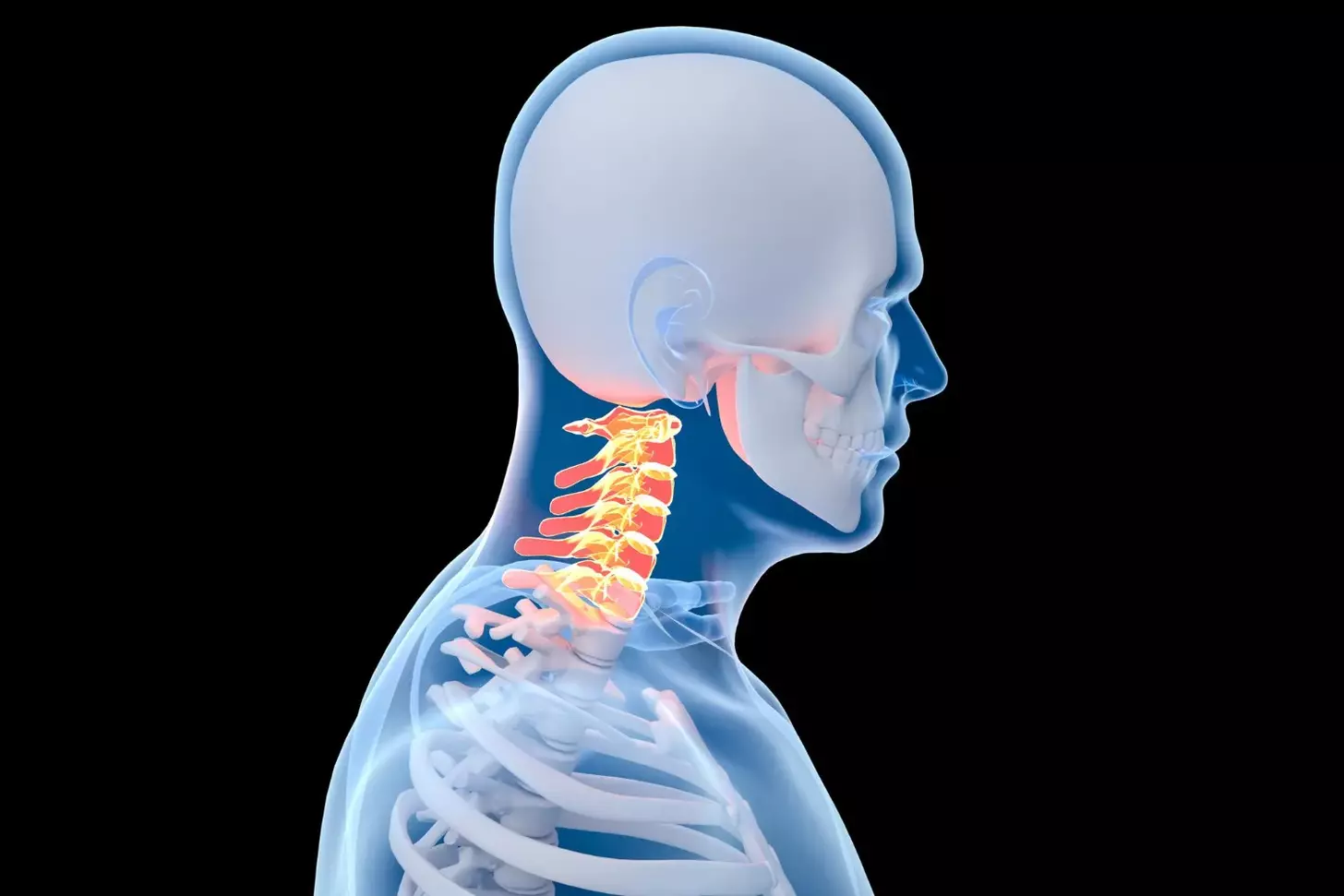
Pain in the Back Side of Heart: A Critical Warning Sign

Cardiac issues can show up as back pain. It’s key to tell the difference between heart pain and back pain. Pain in the back side of the heart might mean a heart problem that needs quick help.
How Cardiac Pain Radiates to the Back
Heart pain can feel like it’s in the back because of the way nerves work. When the heart doesn’t get enough blood or is stressed, it sends pain signals. These signals can make it feel like the pain is coming from the back.
The reasons for this include:
- The phrenic nerve, which connects the heart and diaphragm, can send pain to the back.
- Shared spinal segments also play a part in sending heart pain to the back.
Distinguishing Cardiac Back Pain from Musculoskeletal Issues
Telling cardiac back pain from musculoskeletal issues is important for the right treatment. Musculoskeletal pain usually comes from movement or posture. But cardiac back pain is steady and might come with other signs like shortness of breath or nausea.
Here are the main differences:
- Cardiac back pain feels like a deep, dull ache. Musculoskeletal pain is sharp and linked to certain movements.
- The duration of pain is also telling. Cardiac pain lasts longer, while musculoskeletal pain might go away with rest or a change in position.
Knowing these differences helps figure out if back pain is a sign of a serious heart problem. This can lead to getting medical help right away.
Chest Discomfort: Beyond the Classic Pressure
Heart health is complex, and chest discomfort can show up in many ways. It’s not just a crushing pressure in the chest. Chest sensations can be quite different.
The Spectrum of Chest Sensations
Chest discomfort during a heart attack isn’t just pressure. It can feel like:
- A sharp pain or stabbing sensation
- A dull ache that persists
- A feeling of tightness or squeezing
- Burning or indigestion-like sensations
These different feelings make it hard to know if chest discomfort is a heart problem. But, it’s very important to take any unusual or lasting chest sensations seriously.
Gender Differences in Chest Pain Presentation
Studies show men and women have different heart attack symptoms. Men often feel a classic pressure. Women, on the other hand, might have:
- Sharp or stabbing chest pain
- Pain that spreads to the back, neck, or jaw
- Shortness of breath without chest pain
Knowing these differences helps both patients and doctors spot heart attack symptoms right away.
Key Takeaways:
- Chest discomfort can show up in many ways, not just pressure.
- Men and women have different heart attack symptoms.
- Being aware of these differences can help treat heart issues sooner.
Shortness of Breath: When Breathing Becomes Labored
Labored breathing, or dyspnea, can come from many health problems. These include heart and lung issues. Feeling like you can’t breathe or breathing too fast are signs of this.
Cardiac vs. Respiratory Causes of Dyspnea
Dyspnea can be due to heart or lung problems. Heart issues might mean the heart isn’t pumping well. This can lead to fluid in the lungs, showing signs of heart failure or a heart attack.
Lung problems, like COPD, asthma, or pneumonia, can also cause it. These conditions narrow or block airways, making breathing hard.
Here are some main differences between heart and lung dyspnea:
- Cardiac Dyspnea: Often comes with leg swelling, tiredness, and coughing up pink, frothy mucus.
- Respiratory Dyspnea: Usually has wheezing, coughing, and trouble exhaling.
When Breathing Changes Warrant Emergency Care
Knowing when to get emergency help for shortness of breath is key. If you have any of these symptoms, go to the emergency room:
- Severe trouble breathing or feeling like you’re going to pass out.
- Chest pain or discomfort that gets worse with deep breathing.
- Confusion or trouble staying awake.
- Bluish color of the lips or fingers.
- Severe wheezing or coughing up blood.
Knowing why you’re having trouble breathing is important for the right treatment. If you’re not sure about your symptoms or their cause, it’s safer to get medical help.
Unusual Fatigue and Weakness: Your Body’s Distress Signal
Feeling unusually tired or weak can mean more than just being overworked. It might signal a heart attack or stroke coming. We often think of heart attacks and strokes with big symptoms. But sometimes, the signs are small and easy to miss.
Pre-Event Fatigue as an Early Warning
Pre-event fatigue is when you feel very tired or weak before a heart attack or stroke. It’s not just feeling tired after a long day. It’s a deep, unexplained tiredness that lasts for days or weeks.
It’s key to notice this fatigue because it can lead you to get medical help early. If you’re always tired and can’t shake it off, talk to your doctor.
Sudden Weakness as a Stroke Indicator
Sudden weakness, often on one side of the body, is a stroke warning sign. You might feel numbness, paralysis, or feel heavy on one side. This symptom needs quick action because fast medical help is vital.
Acting fast is very important. If you or someone else suddenly feels weak, call for emergency help right away. This is true if you also notice other stroke signs like facial drooping or trouble speaking.
Knowing about unusual fatigue and weakness can save lives. By spotting these signs and acting quickly, you can greatly improve your chances if a heart attack or stroke happens.
Cold Sweats and Clammy Skin: Autonomic Nervous System Response
The autonomic nervous system reacts to heart attacks or strokes with cold sweats and clammy skin. These are important warning signs. When the body faces a heart emergency, it goes into “fight or flight” mode. This natural stress response gets the body ready to face or flee danger.
This response is controlled by the autonomic nervous system. It handles actions like heart rate and sweating without us thinking about it. During a heart event, stress can make the heart beat faster, blood pressure rise, and breathing quicken, along with sweating.
Why Cardiovascular Events Trigger Sweating
Cardiovascular events make us sweat because of stress. When the heart struggles or doesn’t work right, it sends out stress hormones like adrenaline. These hormones get the body ready for action by speeding up the heart, raising blood pressure, and boosting energy, leading to sweat.
Dr. John Smith, a cardiologist, says, “Sweating is a common symptom during a heart attack, often with chest pain or shortness of breath.”
“Sweating is a physiological response to the stress that a cardiovascular event places on the body,”
he adds.
Differentiating Stress Sweats from Warning Signs
Telling stress sweats from heart event sweats can be hard. But, there are key differences. Stress sweats usually happen with other anxiety signs like a fast heartbeat, shaking, or feeling overwhelmed.
| Symptom | Stress Sweats | Cardiovascular Event |
| Sweating Pattern | Typically involves palms, soles, and underarms | Often cold sweats, clammy skin |
| Associated Symptoms | Anxiety, rapid heartbeat, trembling | Chest pain, shortness of breath, dizziness |
| Onset | Gradual, related to stressor | Sudden, without clear stressor |
If you’re sweating and have chest pain, shortness of breath, or dizziness, get medical help right away.
Knowing the difference between stress sweats and heart event sweats can save lives. Always be cautious with your health.
Nausea and Digestive Distress: Often Overlooked Symptoms
The heart and gut are closely connected. Sometimes, nausea and digestive issues can signal heart problems, not just stomach issues. These symptoms can warn of a heart attack, more so in women.
The Heart-Gut Connection During Cardiac Events
The heart and gut are linked through the autonomic nervous system. This system controls actions like heart rate and digestion. When the heart has a problem, this link can cause stomach symptoms. The body’s stress response can slow digestion, causing nausea, vomiting, or stomach pain.
Studies show heart attack patients often feel nauseous and vomit. Women are more likely to have these symptoms than men. Knowing about the heart-gut connection helps spot heart attack warning signs.
When Digestive Symptoms Should Raise Concern
Not all nausea or stomach discomfort is serious. But, some symptoms could mean a heart problem. If you have:
- Nausea or vomiting with chest pain or discomfort
- Severe abdominal pain
- Shortness of breath
- Cold sweats
- Lightheadedness or dizziness
Seeing these symptoms as heart attack warnings can save lives. Here’s a table to help tell the difference between stomach issues and heart-related symptoms:
| Symptom | Gastrointestinal Issue | Cardiac-Related |
| Nausea/Vomiting | Often follows eating, related to food poisoning or viral gastroenteritis | May occur without eating, accompanied by chest pain or shortness of breath |
| Abdominal Pain | Typically localized, related to meals or bowel movements | May be diffuse, accompanied by other cardiac symptoms |
Knowing about the heart-gut connection and when to worry about stomach symptoms can save lives. It’s about getting medical help fast.
Facial Drooping: The Hallmark Sign of CVA (Cerebrovascular Accident)
A cerebrovascular accident (CVA), or stroke, shows in many ways. Facial drooping is a key sign that means you need to see a doctor right away.
Facial drooping happens when the muscles on one side of the face get weak or paralyzed. This makes one side of the face look uneven or droopy. It’s because the brain’s blood flow stops, damaging the parts that control our facial expressions.
Understanding the FAST Protocol
The FAST protocol helps spot stroke signs. FAST means Face, Arm, Speech, and Time. It’s made to help people quickly see if someone is having a stroke and act fast.
- Face: Ask the person to smile. Does one side of their face droop?
- Arm: Ask the person to raise both arms. Does one arm drift downward?
- Speech: Ask the person to repeat a simple sentence. Is their speech slurred or hard to understand?
- Time: Time is very important. If the person shows any of these signs, act fast.
Subtle Facial Changes to Watch For
Facial drooping is clear, but there are subtle facial changes too. Look for slight unevenness when smiling or trouble closing one eye fully. Paying attention to these signs can help get medical help quickly.
Knowing these signs and the FAST protocol can really help. It can make a big difference for someone having a CVA.
Arm and Limb Weakness: Circulation Warning Signs
Arm or limb weakness can be a sign of a serious heart problem. We look into how these symptoms might point to circulation issues, like heart attacks and strokes.
One-Sided Weakness in Stroke
One-sided weakness, or hemiparesis, is a common stroke symptom. It happens when blood flow to the brain stops, affecting one side of the body. This can cause weakness or paralysis in the arm, leg, or face on one side.
Recognizing one-sided weakness is key. Quick medical help can greatly improve stroke outcomes. We should watch for sudden weakness on one side of the body as a stroke warning.
Bilateral Weakness in Heart Conditions
Bilateral weakness, or weakness on both sides, can be linked to heart issues. For example, heart failure can reduce blood flow to muscles, causing overall weakness.
The table below highlights the main differences between one-sided and bilateral weakness in heart emergencies:
| Characteristic | One-Sided Weakness | Bilateral Weakness |
| Common Cause | Stroke | Heart Conditions (e.g., Heart Failure) |
| Nature of Weakness | Typically affects one side of the body | Affects both sides of the body |
| Onset | Sudden onset | Can be gradual or sudden |
Knowing these differences helps identify the cause of weakness and get the right medical help. If sudden weakness happens, call emergency services right away.
Speech and Cognitive Changes: When to Be Alarmed
It’s important to notice speech and cognitive changes early. These signs can mean a stroke or other brain issues. They might seem small, but they show a big problem that needs quick doctor help.
Types of Communication Difficulties
When a heart problem happens, people might have trouble talking. Slurred speech, trouble finding words, and incoherent or nonsensical speech are warning signs. These changes can really hurt how well someone can talk.
Some might have trouble saying words or sentences. Others might not get what’s being said or follow talks. Seeing these signs should make you call for a doctor right away.
Confusion and Mental Status Changes
Confusion and changes in how someone thinks are also big warnings. Sudden confusion or feeling lost can mean a serious issue, like a stroke. We need to watch for signs of confusion, like not knowing where they are or not following directions.
Mental changes can be mild or very serious. They might include memory loss or trouble solving problems. Seeing these signs means it’s time to get medical help fast.
Knowing about speech and thinking changes helps us know when to get help. Spotting these signs early can really help in emergencies.
Dizziness and Vision Disturbances: Cerebral Blood Flow Warning Signs
Dizziness and vision problems can signal serious issues with blood flow to the brain. This might mean a stroke is happening. When the brain doesn’t get enough blood, it can’t work right.
Vertigo vs. Lightheadedness
Dizziness covers many feelings, like vertigo and lightheadedness. Vertigo makes you feel like you’re spinning, often from ear problems. Lightheadedness feels like you’re going to faint, usually because your brain isn’t getting enough blood.
It’s important to know the difference between vertigo and lightheadedness. Vertigo might be from ear issues, but it can also mean a serious brain problem. Lightheadedness, with vision changes, might show a blood flow issue in the brain.
| Symptom | Vertigo | Lightheadedness |
| Sensation | Spinning or rotational | Faintness or impending faint |
| Common Causes | Inner ear issues, neurological problems | Reduced blood flow to the brain, cardiac issues |
Visual Changes That Signal Emergency
Vision problems can be anything from blurry vision to losing sight in one eye. These signs might mean you’re having a TIA or stroke. Other vision issues include double vision, seeing flashes, or a blind spot.
If your vision suddenly changes, get help right away. These symptoms, with dizziness, can mean a serious problem with blood flow to the brain.
Quick action when you see these warning signs can greatly help if you’re having a stroke or other heart emergency.
Conclusion: When to Seek Emergency Care
It’s vital to know the signs of a heart attack and stroke to get help fast. We’ve talked about symptoms like pain in the back of the heart and chest discomfort. Also, shortness of breath, unusual fatigue, and cold sweats are important signs.
Nausea, facial drooping, arm and limb weakness, and speech changes are other warning signs. Dizziness is also a symptom to watch out for.
If you or someone you know is showing these signs, get emergency care right away. At Liv Hospital, we offer top-notch care for international patients. Our team is ready to help with world-class healthcare and support.
Quick medical help can make a big difference in heart and stroke emergencies. If you see these symptoms, don’t wait. Act fast to get the care you need.
FAQ
What are the early warning signs of a heart attack or stroke?
Early signs of a heart attack or stroke include pain in the back of the heart and chest discomfort. Shortness of breath and unusual fatigue are also signs. Cold sweats, nausea, and facial drooping are other symptoms.
Arm and limb weakness, speech changes, and dizziness are also warning signs. Vision disturbances can also indicate a problem.
How does cardiac pain radiate to the back?
Cardiac pain can spread to the back because of shared nerve paths. This makes it hard to tell if it’s heart or back pain.
What is the difference between a heart attack and a stroke?
A heart attack blocks blood to the heart. A stroke blocks blood to the brain. Both need quick medical help.
What are the symptoms of a heart attack in men and women?
Men and women both might feel chest pain during a heart attack. But women often have other symptoms too. These include shortness of breath, nausea, and feeling very tired.
How can I differentiate between cardiac and respiratory causes of shortness of breath?
Shortness of breath from the heart often comes with chest pain or feeling very tired. Respiratory issues like asthma or COPD might not have these extra symptoms.
What is the FAST protocol for identifying stroke symptoms?
The FAST protocol checks for Facial drooping, Arm weakness, Speech issues, and Time to call for help.
Can nausea and digestive distress be symptoms of a heart attack?
Yes, nausea and digestive issues can be signs of a heart attack, more so in women.
What are the signs of a stroke?
Stroke signs include facial drooping, arm weakness, speech changes, and dizziness. Vision problems are also signs.
When should I seek emergency care for symptoms of a heart attack or stroke?
If you have chest pain, shortness of breath, facial drooping, or arm weakness, get emergency help right away.
How can I distinguish between stress-induced sweating and warning signs of a heart attack?
Stress sweating usually comes with anxiety or a racing heart. Heart attack sweating often has chest pain too.
What are the causes of dizziness and vision disturbances during a cardiovascular event?
Dizziness and vision problems can mean a stroke or heart issue. They happen when blood flow to the brain is affected.
Can unusual fatigue and weakness be early warning signs of a cardiovascular event?
Yes, feeling very tired or weak can be a sign of a heart problem. Look for other symptoms like chest pain or shortness of breath too.
References
- Martinez-Lemus, L. A. (2012). The dynamic structure of arterioles. Basic & Clinical Pharmacology & Toxicology, 110(1), 5-11. https://pubmed.ncbi.nlm.nih.gov/21989114/