Last Updated on November 26, 2025 by Bilal Hasdemir
At Liv Hospital, we use balloon angioplasty to treat heart disease. This method is minimally invasive. It helps restore blood flow to the heart muscle.
We inflate a small balloon at the blockage site. This opens narrowed or blocked arteries. It’s a life-saving technique.
This method relieves angina symptoms and lowers heart attack risk. It greatly improves patients’ lives with little recovery time. Our team follows international standards and puts patients first, focusing on safety, innovation, and trust.
Key Takeaways
- Balloon angioplasty is a minimally invasive procedure used to treat coronary artery disease.
- The procedure involves inflating a small balloon to open blocked or narrowed arteries.
- It helps restore blood flow to the heart muscle, relieving angina symptoms.
- The treatment significantly reduces the risk of heart attack.
- Patients experience minimal recovery time, improving their quality of life.
What Is Balloon Angioplasty and How Does It Work
Balloon angioplasty, also known as percutaneous transluminal angioplasty (PTA), is a procedure to widen narrowed blood vessels. It’s a less invasive method compared to traditional surgery. This technique has greatly helped in treating coronary artery disease.
Definition and Medical Purpose
Balloon angioplasty uses a balloon catheter to open up blocked arteries. Its main goal is to improve blood flow to the heart. This helps reduce symptoms like chest pain and lowers the risk of heart attacks.
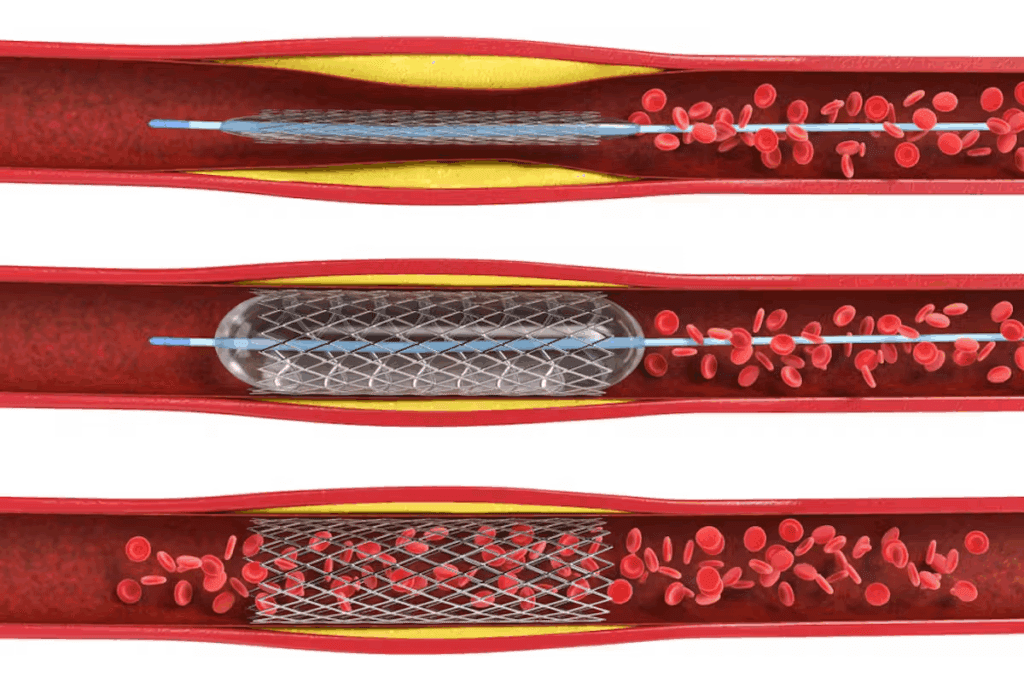
An angioplasty balloon catheter is used to reach the blockage in the coronary artery. Once there, the balloon is inflated. This pushes aside plaque and stretches the artery, improving blood flow.
History and Evolution of the Procedure
The idea of balloon angioplasty was started in the late 1970s by an expert. It was a big step forward in heart treatments. Over time, it has evolved with new stents and better catheters.
| Year | Milestone |
| 1977 | First balloon angioplasty was performed by an expert . |
| 1980s | Introduction of bare-metal stents |
| 1990s | Development of drug-eluting stents |
Mechanism of Action in Treating Coronary Artery Disease
The process of balloon catheter angioplasty starts with a guidewire. It guides the angioplasty balloon catheter to the blockage. When inflated, the balloon pushes plaque against the wall, widening the artery.
Often, a stent is placed to keep the artery open. The whole procedure is watched under fluoroscopy, allowing for real-time monitoring.
Understanding balloon angioplasty helps patients make better choices for treating coronary artery disease.
Medical Indications for Balloon Angioplasty

We use balloon angioplasty to treat heart conditions caused by atherosclerosis and vascular stenosis. This method helps restore blood flow to the heart muscle. It relieves symptoms and improves life quality.
Symptoms and Conditions Requiring Intervention
Balloon angioplasty is mainly for those with coronary artery disease symptoms. Symptoms include chest pain (angina), shortness of breath, and fatigue. It’s also for those with big blockages that could lead to a heart attack.
Conditions needing this procedure include stable angina, unstable angina, and heart attacks. The choice to do the procedure depends on the patient’s health and how severe their condition is.
Diagnostic Tests That Determine Candidacy
To see if a patient is right for balloon angioplasty, we use several tests. These include coronary angiography, stress tests, and cardiac imaging like echocardiography or cardiac MRI.
Coronary angiography is key. It shows the coronary arteries in detail. This helps doctors plan the angioplasty.
Emergency vs. Elective Procedure Considerations
Balloon angioplasty can be urgent or planned. In heart attacks, it’s often urgent to get blood flowing again.
For stable heart disease, it’s planned. The choice between urgent and planned depends on the situation and the patient’s risk.
Essential Equipment and Tools for the Procedure
To do balloon angioplasty well, doctors need many important tools. The right tools are key to a successful procedure.
Angioplasty Balloon Catheter Types and Selection Criteria
The angioplasty balloon catheter is a key part of the process. It’s a flexible tube with a balloon that can be inflated. There are different types of catheters, like:
- Over-the-wire catheters, which are pushed through with a guidewire.
- Rapid-exchange catheters, for quicker changes during the procedure.
- Cutting balloon catheters for tougher blockages.
Choosing the right catheter depends on its size, length, and material.
Guidewires, Introducers, and Support Devices
Guidewires help guide the catheter to the right spot. They come in different sizes and shapes. Introducers help get the catheter into the blood vessels. Support devices help keep the catheter steady and easy to move.
Imaging Systems and Contrast Media
Imaging systems, like fluoroscopy, are important for seeing what’s happening. Contrast media make blood vessels show up better on images. Choosing the right contrast media is important to avoid bad reactions.
Stent Types and Selection Factors
Stents are used with balloon angioplasty to keep arteries open. There are many types, like bare-metal and drug-eluting stents. Doctors choose based on how likely the artery is to narrow again, the blockage’s complexity, and the patient’s ability to take antiplatelet drugs.
Pre-Procedure Patient Preparation Protocol

The pre-procedure patient preparation is key in the balloon angioplasty process. It makes sure patients are ready for the treatment. We know that a heart catheter balloon procedure can be scary for many. Our goal is to make this process as easy and stress-free as we can.
Patient Assessment and Eligibility Evaluation
Before the balloon heart procedure, patients get a full check-up. This includes looking at their medical history, doing a physical exam, and talking about their symptoms and hopes.
We also check the patient’s overall health and any other health issues that might affect the procedure or recovery. This helps us make a treatment plan that fits the patient’s needs.
Laboratory Tests and Imaging Requirements
To find out where and how bad the blockage is, patients need to do some tests. These tests include blood work, an electrocardiogram (ECG), a chest X-ray, and coronary angiography.
| Test | Purpose |
| Blood Tests | Evaluate overall health and detect any issues |
| Electrocardiogram (ECG) | Check how the heart is working and if there are any irregular heartbeats |
| Chest X-ray | Look at the size of the heart and the lungs |
| Coronary Angiography | See the coronary arteries and find blockages |
Medication Management Before the Procedure
Managing medications is very important before the procedure. Patients need to tell us about all the medications they are taking, including blood thinners. They also need to follow specific instructions about taking medications before the balloon angioplasty procedure.
We might tell patients to stop taking certain medications before the procedure to lower the risk of bleeding.
Informed Consent Process and Patient Education
Before the procedure, patients talk to an interventional cardiologist. They review the test results, go over the procedure steps, and understand what to expect before, during, and after.
We also get informed consent from patients. This makes sure they know the possible risks and benefits of the heart catheter balloon procedure.
By following this detailed pre-procedure patient preparation, we can make sure patients are ready for their balloon angioplasty. This helps lower risks and improve outcomes.
Step-by-Step Balloon Angioplasty Procedure Guide
We’ll walk you through the steps of balloon angioplasty, a key heart treatment. It starts with a small incision in the skin to access a blood vessel. Then, a guidewire and balloon catheter are inserted.
Patient Positioning and Sterile Field Preparation
The first step is to get the patient ready on the table. We make sure they’re comfortable and won’t move during the procedure. The area for the catheter is cleaned and sterilized to avoid infection.
A sterile field is set up around the insertion site with drapes. This sterile environment helps prevent complications. Our team wears sterile gloves and gowns to keep everything clean.
Vascular Access Techniques (Femoral vs. Radial Approach)
There are two main ways to access blood vessels: the femoral and radial approaches. The femoral approach uses the groin artery, while the radial approach uses the wrist artery. The choice depends on the patient’s anatomy and the doctor’s preference.
We decide which approach is best based on the patient’s condition. A small incision is made, and a sheath is inserted into the artery.
Catheter Navigation to the Blockage Site
With vascular access, we guide a guidewire to the blockage. This is done under fluoroscopy, allowing us to see the guidewire’s path. Then, a balloon catheter is moved over the guidewire to the blockage site.
The balloon catheter is placed across the lesion, ready for inflation.
Lesion Assessment and Treatment Planning
Before inflating the balloon, we check the lesion’s size and the pressure needed. This ensures the balloon is the right size and won’t harm the artery.
We use angiography to look at the lesion and plan the treatment. This helps us choose the best balloon catheter and stent.
Post-Balloon Angioplasty Care Protocol
The care plan after balloon angioplasty is key to avoiding problems and helping patients feel better. Right after the procedure, patients go to the post-anesthesia care unit (PACU). There, they are watched until they are fully awake and stable.
Immediate Post-Procedure Monitoring Requirements
Right after the procedure, we keep a close eye on the patient’s vital signs. This includes heart rate, blood pressure, and oxygen levels. We also look out for any signs of complications, like bleeding or vascular problems.
Vital Sign Monitoring is very important in the first hours after the procedure. This includes:
- Continuous ECG monitoring
- Regular blood pressure checks
- Oxygen saturation monitoring
Vascular Access Site Management and Hemostasis
Managing the vascular access site well is key to avoid bleeding and help the site heal. We use different methods, like manual compression and closure devices, to do this.
| Method | Description | Advantages |
| Manual Compression | Applying manual pressure to the access site | Low cost, effective |
| Closure Devices | Using devices to seal the arterial puncture | Reduces bleeding risk, faster recovery |
Medication Administration and Antiplatelet Therapy
After balloon angioplasty, patients get medicines to stop clots and help the artery heal. Antiplatelet therapy is a big part of this.
Antiplatelet Therapy typically includes:
- Aspirin
- P2Y12 inhibitors (e.g., clopidogrel)
Early Complication Detection and Management
Spotting complications early is very important for quick action. We watch for signs of bleeding, vascular problems, and other issues.
By sticking to a detailed post-balloon angioplasty care plan, we can greatly improve patient results and lower the chance of problems.
Managing Complications During and After the Procedure
While balloon angioplasty is a minimally invasive procedure, it’s important to know about possible complications. Medical professionals must be ready for any issues to ensure the best results for patients.
Periprocedural Complications and Emergency Interventions
During the procedure, complications like coronary artery dissection, thrombosis, and cardiac arrhythmias can happen. Prompt recognition and management of these issues are key to avoiding bad outcomes. For example, coronary artery dissection might need immediate stenting to fix blood flow.
“The key to managing periprocedural complications lies in swift and effective intervention,” says a leading cardiologist. “Being prepared for emergencies is part of delivering high-quality care.”
Post-Procedure Complications (Short and Long-term)
After the procedure, patients might face short-term issues like bleeding at the access site, vascular complications, or acute kidney injury. Long-term problems can include restenosis, where the artery narrows again. Regular follow-up and monitoring are key to catch and manage these issues early.
- Restenosis
- Bleeding complications
- Vascular complications
- Acute kidney injury
Risk Factors for Complications
Some factors increase the risk of complications during and after balloon angioplasty. These include complex coronary lesions, diabetes, renal insufficiency, and a history of cardiovascular disease. Knowing these risk factors helps tailor the treatment plan to each patient’s needs.
| Risk Factor | Description |
| Complex Coronary Lesions | Lesions that are difficult to treat due to their location or characteristics |
| Diabetes | Patients with diabetes are at higher risk of complications and restenosis |
Prevention Strategies and Management Approaches
Preventing complications involves careful patient selection, precise procedural technique, and thorough post-procedure care. Antiplatelet therapy is key in managing patients after balloon angioplasty to prevent thrombotic complications. Lifestyle changes and sticking to medication are also important for long-term success.
By understanding complications and using effective prevention and management strategies, we can improve patient outcomes after balloon catheter angioplasty.
Patient Recovery and Long-Term Follow-Up
Recovering after an angioplasty involves several steps. These include getting discharge instructions, knowing what activities to avoid, and attending follow-up appointments. Each step is important for a smooth recovery.
Hospital Discharge Criteria and Instructions
Before leaving the hospital, patients must meet certain criteria. They need to have stable vital signs and a well-healing vascular access site. They also need to understand how to care for themselves at home.
We give detailed instructions on wound care and what to watch for. This helps prevent complications.
Activity Restrictions and Gradual Resumption
Patients are told to avoid heavy lifting and bending after the procedure. They should also avoid strenuous activities for a while. Slowly getting back to normal activities is key to healing.
Medication Compliance and Lifestyle Modifications
It’s important to take medications as directed after an angioplasty. Patients are given antiplatelet therapy to prevent clots. They must stick to their medication plan.
Changing your lifestyle is also important. Eating well, exercising regularly, and quitting smoking can help your heart health in the long run.
Follow-Up Appointments and Monitoring Schedule
Regular check-ups are vital to monitor recovery. These visits help adjust treatment plans and offer support. A typical schedule includes visits at one week, one month, and three months after the procedure.
| Follow-Up Visit | Typical Assessment |
| 1 Week | Check vascular access site, review medication adherence |
| 1 Month | Assess overall recovery, adjust medications as needed |
| 3 Months | Evaluate long-term outcomes, discuss lifestyle modifications |
Following the recommended care plan and schedule helps patients recover well after a heart balloon procedure.
Conclusion
Balloon angioplasty is a life-saving procedure that has changed how we treat heart disease. It helps restore blood flow to the heart. By understanding this process, patients can see the care and precision involved.
This procedure is a key treatment for heart disease. It offers quick recovery times and works well for many patients. Proper preparation, careful technique, and post-care all lead to good results.
Balloon angioplasty greatly improves life for those with heart disease. It boosts survival rates and quality of life. We highlight the importance of ongoing advancements in heart care and our dedication to top-notch healthcare.
FAQ
What is balloon angioplasty?
Balloon angioplasty is a procedure to open blocked arteries. It helps blood flow to the heart. This relieves symptoms like chest pain.
How does balloon angioplasty work?
A catheter with a balloon is guided to the blockage. The balloon is then inflated. This widens the artery and improves blood flow.
What is the purpose of using a stent during balloon angioplasty?
A stent keeps the artery open after the balloon widens it. This reduces the risk of the artery narrowing again.
What are the symptoms that may require balloon angioplasty?
Symptoms like chest pain, shortness of breath, or signs of coronary artery disease may need balloon angioplasty.
How is candidacy for balloon angioplasty determined?
Tests like angiography, stress tests, and echocardiograms are used. They check the severity of coronary artery disease.
What is the difference between emergency and elective balloon angioplasty?
Emergency angioplasty is for urgent situations like a heart attack. Elective angioplasty is planned for stable disease.
What are the risks associated with balloon angioplasty?
Risks include bleeding, vascular complications, heart attack, stroke, and artery narrowing again.
How long does recovery take after balloon angioplasty?
Recovery takes a few days to a week. Patients should avoid heavy lifting and follow medication instructions.
What lifestyle changes are recommended after balloon angioplasty?
Adopt a heart-healthy lifestyle. This includes a balanced diet, regular exercise, and managing conditions like hypertension and diabetes.
How often are follow-up appointments needed after balloon angioplasty?
Follow-up appointments are within a few weeks. They are then as needed, based on the patient’s condition.
Can balloon angioplasty cure coronary artery disease?
Balloon angioplasty treats blocked arteries and relieves symptoms. But it’s not a cure for coronary artery disease. Ongoing management and lifestyle changes are key.
What is cardiac balloon catheterization?
Cardiac balloon catheterization uses a catheter with a balloon. It diagnoses and treats coronary artery disease by widening blocked or narrowed arteries.
What is the role of antiplatelet therapy after balloon angioplasty?
Antiplatelet therapy is important after balloon angioplasty and with stent placement. It prevents blood clots and reduces heart attack risk.
Reference
- Levine, G. N., Bates, E. R., Blankenship, J. C., Bailey, S. R., Bittl, J. A., Cercek, B., … & Smith, P. K. (2011). 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention. Journal of the American College of Cardiology, 58(24), e44-e122.
https://www.jacc.org/doi/full/10.1016/j.jacc.2011.08.007





