Last Updated on November 25, 2025 by Ugurkan Demir

View benign prostatic hyperplasia images and learn 6 essential facts about BPH’s pathophysiology, etiology, and diagnostic procedures.
Benign Prostatic Hyperplasia (BPH) is a common issue for men as they get older. It makes the prostate gland grow bigger, causing problems with urination. Knowing about BPH means looking into its causes, symptoms, and how to treat it.
BPH is very common in older men, with more cases after 40. The exact reason for BPH isn’t known, but it’s thought to be linked to hormonal changes with age.
Signs of BPH include trouble starting to pee, a weak urine stream, needing to pee a lot, and waking up to pee at night. There are many ways to treat BPH, from simple changes in lifestyle to medicines and sometimes surgery.
What Is Benign Prostatic Hyperplasia?

Benign Prostatic Hyperplasia (BPH) is when the prostate gland gets bigger. This is common in older men. It can press on the urethra, leading to urinary problems.
As men get older, more of them face BPH. It’s important to know about its causes, symptoms, and treatments. This helps manage the condition better.
Prevalence and Demographics
BPH is a big concern for older men. Research shows it affects up to 50% of men by 60. By 80, it affects nearly 90%.
Clinical Significance
BPH causes urinary issues like weak flow and frequent need to urinate. These problems can really affect a man’s life. They can mess with sleep and daily activities.
Understanding BPH and its symptoms is key. Knowing the treatment options helps men live better lives. It also lowers the risk of serious problems.
Essential Fact #1: Anatomical Changes in BPH
Understanding BPH’s anatomical changes is key to diagnosing and treating it well. Benign Prostatic Hyperplasia changes the prostate’s structure. This can cause urinary blockage and other issues.
Normal Prostate Anatomy
The prostate gland is like a walnut, located below the bladder and around the urethra. In a healthy male, the prostate has different zones, including the transition zone. Normal prostate anatomy helps keep urine flowing freely.
Transition Zone Enlargement
In BPH, the transition zone grows too much, causing the prostate to enlarge. This growth presses on the urethra, leading to urinary problems. A medical expert notes, “The growth of the transition zone is a main cause of BPH symptoms.”
“The enlargement of the transition zone is a hallmark of BPH, resulting in significant urethral compression.”
Urethral Compression and Obstruction
The enlarged transition zone squeezes the urethra, causing urethral obstruction. This can lead to weak urine flow, straining, and not fully emptying the bladder. The severity of BPH symptoms often matches the degree of urethral compression.
BPH’s changes can greatly affect a man’s life. By understanding these changes, doctors can create better treatment plans. This helps improve symptoms and quality of life for patients.
Essential Fact #2: Pathophysiology of BPH
BPH is when the prostate gland gets bigger, causing urinary problems. Hormones, like testosterone, play a big part in this.
The growth of BPH is complex. Hormones, like DHT, help prostate cells grow. This makes the prostate bigger.
Essential Fact #3: Histological Features of BPH
Benign Prostatic Hyperplasia (BPH) makes the prostate gland grow bigger. This happens because more cells are added, forming nodules. The growth of both glandular and stromal elements is seen in BPH.
Nodular Hyperplasia
The main sign of BPH is nodular hyperplasia. This is when cells grow too much and form nodules. These nodules can block the urethra, causing trouble with urination.
Cellular Changes
The cells in the prostate change in BPH. The glandular parts grow too much. This makes the prostate gland bigger.
Knowing about BPH’s histological features is key for diagnosis and treatment. Doctors can plan better treatments by looking at these changes. This helps improve symptoms and outcomes for patients.
Benign Prostatic Hyperplasia Images: Visual Guide to Diagnosis
Benign Prostatic Hyperplasia (BPH) is common in older men. It makes the prostate gland grow bigger. This can cause urinary problems, affecting daily life.
Gross Pathological Specimens
Looking at BPH specimens, you see a big prostate gland. The size and weight differ from person to person.
Microscopic Features
Under a microscope, BPH shows more gland and tissue. It’s mainly the transitional zone of the prostate that grows too much.
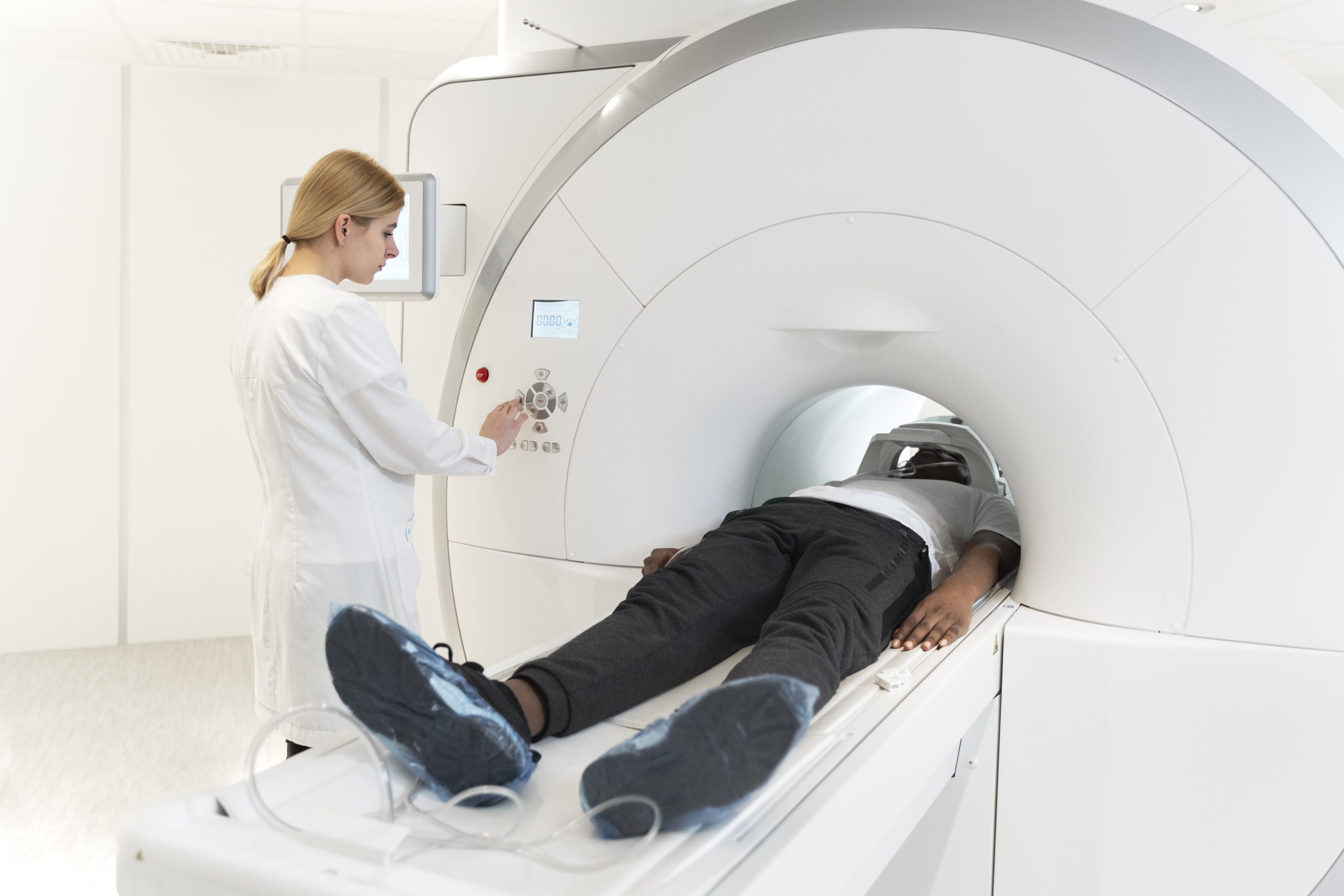
Radiological Imaging
Imaging tests like ultrasound and MRI are key in diagnosing BPH. They help see how big the prostate is and how much it’s grown.
Clinical Implications
Knowing about BPH is vital for treatment. Getting the right diagnosis and treatment helps ease symptoms. This improves the patient’s life quality.
Essential Fact #4: Etiology of Benign Prostatic Hyperplasia
The causes of BPH are complex and involve many factors. These include age-related changes, hormonal influences, and genetic predispositions. Knowing these factors helps in finding better ways to prevent and treat BPH.
Age-Related Factors
Age is a big risk factor for BPH. It’s rare in men under 40 but affects up to 80% of men by 80. As men get older, their prostate gland changes. This leads to BPH.
Androgen Dependence
Androgens, like dihydrotestosterone (DHT), are key in BPH. The conversion of testosterone to DHT is important. This shows how hormones play a big role in BPH.
Genetic Predisposition
Genetics also play a part in BPH. Men with a family history of BPH are more likely to get it. This suggests a genetic link to BPH.
Metabolic Syndrome and Inflammation
Metabolic syndrome and chronic inflammation are also important in BPH. Men with metabolic syndrome are at higher risk of BPH. Inflammation in the prostate gland may also contribute to BPH.
In summary, BPH has many causes. These include age, hormones, genetics, and metabolic syndrome and inflammation. Understanding these causes is key to managing BPH effectively.
Essential Fact #5: Clinical Diagnosis of BPH
To diagnose BPH, doctors look at many things. They consider symptoms, medical history, and test results. This helps make sure the right treatment is chosen.
Patient History and Symptom Assessment
Diagnosing BPH starts with a detailed patient history and symptom check. We use the International Prostate Symptom Score (IPSS) to measure symptoms. These include problems like not being able to hold urine, weak flow, and trouble starting to urinate.
- Assessing the impact of symptoms on quality of life
- Identifying possible other health issues that might affect symptoms
- Looking at medications that could change urine symptoms
Physical Examination
A physical exam is key to finding signs of BPH or other problems. We do a digital rectal exam (DRE) to check the prostate. This helps us see if it’s enlarged or has any unusual areas.
Key findings on DRE may include:
- Enlarged prostate
- Prostate nodules or irregularities
- Tenderness or pain upon palpation
Laboratory Testing
Labs help us rule out other reasons for urinary issues and check for BPH complications. We do urinalysis to look for blood or infection. We also check prostate-specific antigen (PSA) levels to see how the prostate is doing.
Differential Diagnosis
When diagnosing BPH, we also think about other conditions that might look like BPH. We check for things like urinary tract infections, prostate cancer, and how medications might affect symptoms.
Essential Fact #6: Management Approaches for BPH
Managing Benign Prostatic Hyperplasia (BPH) needs a mix of treatments. This helps ease symptoms and boosts quality of life. Each patient’s needs are unique, so a personalized plan is key.
Medical Therapies
Medical treatments are often the first step for BPH. Alpha-blockers, like tamsulosin, relax prostate muscles. This improves urine flow and lessens symptoms.
5-alpha-reductase inhibitors, such as finasteride, shrink the prostate over time. “Combining alpha-blockers and 5-alpha-reductase inhibitors is more effective than using one alone,” say experts.
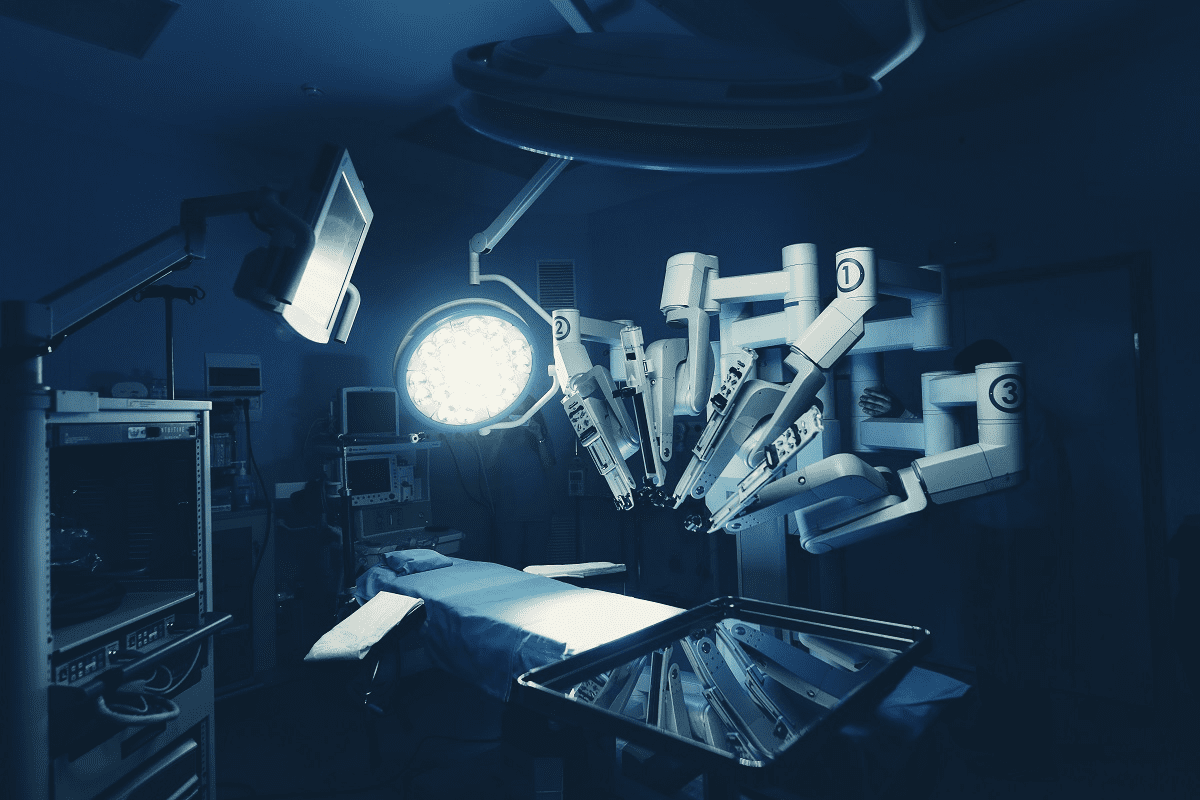
Surgical Interventions
For severe symptoms or when medical therapy fails, surgery is needed. Transurethral resection of the prostate (TURP) removes excess tissue. This improves urine flow.
Other surgeries, like open prostatectomy and laser surgery, are also options. They help those with larger prostates or complex cases.
Minimally Invasive Procedures
Minimally invasive methods are becoming more popular. They offer quick recovery and fewer side effects. Techniques like TUMT and TUNA use heat or radiofrequency to shrink the prostate.
“These methods are great for those at high risk for surgery or who prefer less invasive options,” studies show.
Lifestyle Modifications
Lifestyle changes are also important for BPH management. Drinking less before bed, avoiding caffeine and alcohol, and staying active are key. Pelvic floor exercises and bladder training also help.
By using these approaches together, healthcare providers can tailor care for BPH patients. This improves symptoms, quality of life, and overall well-being.
Conclusion: Advances in BPH Understanding and Management
Benign Prostatic Hyperplasia, or BPH, is a complex condition. It needs a detailed approach for diagnosis and treatment. Healthcare providers can offer effective care by understanding its causes, symptoms, and treatment options.
As research keeps moving forward, we’ll see better results. This means a higher quality of life for those dealing with BPH.
FAQ
Q: What is Benign Prostatic Hyperplasia (BPH)?
BPH is a non-cancerous enlargement of the prostate gland. It can cause urinary symptoms in men.
Q: What are the symptoms of BPH?
The symptoms of BPH include trouble starting to urinate and a weak urine flow. Men may also urinate more often and wake up at night to use the bathroom.
Q: How is BPH diagnosed?
BPH is diagnosed by looking at a man’s medical history and doing a physical exam. Tests like PSA testing, uroflowmetry, and PVR measurement are also used.
Q: What are the treatment options for BPH?
There are several ways to treat BPH. These include watching the condition, taking medications, or undergoing surgery like TURP.
Q: What are the possible complications of untreated BPH?
Untreated BPH can cause urinary retention and damage to the bladder and kidneys.
Q: Can BPH be prevented?
While there’s no sure way to prevent BPH, a healthy lifestyle can help. Eating well and exercising regularly may reduce the risk.
Q: How is BPH managed?
BPH is managed with lifestyle changes, medications, and sometimes surgery. Changes in diet and more exercise are recommended. Medications like alpha-blockers and 5-alpha-reductase inhibitors can help. In severe cases, surgery like TURP may be needed.
References
National Center for Biotechnology Information. (2025). Benign Prostatic Hyperplasia Images 6 Essential Facts on. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC1477609/