Last Updated on November 27, 2025 by Bilal Hasdemir
Hernia surgery is a common effective treatment for hernias, offering relief and preventing further complications. The choice of surgical technique is crucial for a successful outcome.
The best hernia treatment options include three primary repair techniques: open, laparoscopic, and robotic repair. Each method has its advantages and is suited to different patient needs.
Understanding the differences between these hernia repair techniques is essential for making an informed decision. This article will explore the various surgical approaches, including laparoscopic hernia surgery, to help you choose the best hernia treatment option.
Key Takeaways
- Understanding the different types of hernia repair techniques is crucial.
- Laparoscopic hernia surgery offers several benefits, including less recovery time.
- The choice of surgical technique depends on individual patient needs.
- Effective hernia treatment requires a skilled surgeon.
- Robotic repair is a modern approach with promising outcomes.
Understanding Hernias: Types and Causes
A hernia occurs when an organ or tissue bulges through a weakened area in the muscle or connective tissue. This condition can be painful and often requires surgical intervention. Understanding the different types of hernias and their causes is crucial for determining the best treatment approach.
Common Types of Hernias
There are several types of hernias, each with distinct characteristics. The most common types include:
- Inguinal Hernia: Occurs when tissue, such as part of the intestine, protrudes through a weak spot in the abdominal muscles in the groin area.
- Umbilical Hernia: Happens when part of the intestine bulges through an opening in the abdominal muscles near the navel.
- Incisional Hernia: Develops through a scar or incision in the abdominal wall, resulting from previous abdominal surgery.
- Hiatal Hernia: Occurs when the stomach bulges up into the chest through an opening in the diaphragm.
Risk Factors and Causes
Several factors can increase the risk of developing a hernia, including:
- Age: Hernias are more common in older adults due to the natural weakening of muscles with age.
- Family History: Having a family history of hernias can increase an individual’s risk.
- Chronic Coughing or Sneezing: Persistent coughing or sneezing can put strain on the abdominal muscles.
- Heavy Lifting: Lifting heavy objects can increase pressure on the abdominal wall.
- Obesity: Excess weight can put additional strain on the muscles.
When Surgery Becomes Necessary
Not all hernias require immediate surgery, but surgical repair is often necessary to prevent complications such as incarceration or strangulation of the hernia. The decision to undergo surgery depends on the type of hernia, its size, and the severity of symptoms. For instance, inguinal hernia surgery is a common procedure to repair groin hernias.
Understanding the types of hernias and their causes is essential for making informed decisions about treatment. By recognizing the risk factors and knowing when surgery is necessary, individuals can take proactive steps towards managing their condition and improving their quality of life.
Overview of Hernia Repair Techniques
Understanding the different hernia repair techniques is crucial for determining the best course of treatment. Hernia repair has evolved significantly over the years, with various methods now available to suit different patient needs.
Tension vs. Tension-Free Repairs
Hernia repair techniques can be broadly categorized into tension and tension-free repairs. Traditional hernia repair involved suturing the edges of the hernia defect, which often resulted in tension on the surrounding tissue. This tension could lead to post-operative pain and a higher risk of recurrence. In contrast, tension-free repairs utilize a mesh to bridge the hernia defect, reducing tension on the surrounding tissue and promoting a more natural healing process.
Tension-free repairs have become the preferred method due to their lower recurrence rates and reduced post-operative discomfort. The use of mesh in hernia repair has revolutionized the field, enabling surgeons to perform repairs with greater ease and efficacy.
Mesh vs. Non-Mesh Approaches
The debate between mesh and non-mesh approaches continues, with each having its own set of advantages and disadvantages. Mesh hernia repair involves the use of a synthetic or biological mesh to reinforce the weakened area. This approach has been shown to reduce recurrence rates significantly. However, concerns regarding mesh-related complications, such as adhesions and chronic pain, have led some surgeons to explore non-mesh techniques.
Non-mesh approaches, such as suturing or tissue repair, are typically reserved for specific cases, such as small hernias or in patients with certain comorbidities. While these methods avoid the potential complications associated with mesh, they may have higher recurrence rates.
Evolution of Hernia Surgery Methods
Hernia surgery has undergone significant evolution, driven by advances in technology and a deeper understanding of hernia pathology. From traditional open repairs to minimally invasive laparoscopic techniques, the field has seen a shift towards less invasive procedures that promote quicker recovery times.
The development of robotic-assisted surgery has further enhanced the precision and control available to surgeons, allowing for more complex repairs to be performed with greater ease. As technology continues to advance, it is likely that hernia repair techniques will continue to evolve, offering patients even more effective and personalized treatment options.
Open Hernia Surgery: Traditional Approach
As a long-standing treatment for hernias, open hernia surgery offers a reliable solution. This traditional approach has been refined over the years to address the complexities of hernia repair.
The Procedure Explained
Open hernia surgery involves making an incision in the abdomen to access the hernia directly. The surgeon then pushes the herniated tissue back into place and reinforces the weakened area, often using a mesh to provide additional support.
The steps involved in open hernia surgery include:
- Making an incision near the site of the hernia
- Identifying and isolating the hernia sac
- Reducing the hernia and excising the sac if necessary
- Repairing the defect with or without mesh
- Closing the incision
Advantages and Limitations
Open hernia surgery has several advantages, including its simplicity and the ability to perform it without specialized equipment. However, it also has limitations, such as a potentially longer recovery time compared to minimally invasive techniques.
“The open approach remains a valuable technique in the surgeon’s armamentarium, particularly for complex or recurrent hernias.” –
Surgical Expert
A comparison of the advantages and limitations is provided in the table below:
| Aspect | Advantages | Limitations |
| Recovery Time | Simple procedure | Longer recovery |
| Equipment Requirement | No specialized equipment needed | Limited applicability for complex cases |
| Surgeon Expertise | Wide applicability | Higher risk of complications |
Ideal Candidates for Open Repair
Open hernia surgery is particularly suitable for patients with larger hernias, those who are not good candidates for laparoscopic surgery due to health reasons, and individuals with previous abdominal surgery that may complicate laparoscopic access.
The decision to undergo open hernia surgery should be made after consulting with a healthcare provider, who can assess the individual’s condition and recommend the most appropriate treatment.
Laparoscopic Hernia Surgery: Minimally Invasive Option
The advent of laparoscopic techniques has revolutionized hernia repair, providing patients with quicker recovery times and less post-operative pain. Laparoscopic hernia surgery, a minimally invasive procedure, has become increasingly popular among both patients and surgeons due to its numerous benefits over traditional open surgery.
How Laparoscopic Repair Works
Laparoscopic hernia repair involves making several small incisions in the abdomen through which a laparoscope and surgical instruments are inserted. The laparoscope, equipped with a camera, transmits images to a monitor, allowing the surgeon to visualize the hernia and surrounding tissue. The hernia is then repaired by reinforcing the weakened area with mesh.
Key Steps in Laparoscopic Hernia Repair:
- Insertion of the laparoscope and instruments through small incisions
- Visualization of the hernia on a monitor
- Repair of the hernia using mesh to reinforce the weakened area
- Closure of the incisions
Benefits Over Traditional Surgery
Laparoscopic hernia surgery offers several advantages over traditional open repair, including less post-operative pain, reduced risk of infection, and quicker return to normal activities. The smaller incisions result in less tissue trauma, contributing to these benefits.
Comparative Benefits:
| Aspect | Laparoscopic Surgery | Open Surgery |
| Pain Level | Less | More |
| Recovery Time | Quicker | Longer |
| Risk of Infection | Lower | Higher |
Potential Drawbacks to Consider
While laparoscopic hernia surgery has numerous benefits, it also has potential drawbacks. These include the need for general anesthesia, a longer learning curve for surgeons, and the risk of certain complications such as bowel injury.
It’s crucial for patients to discuss these aspects with their surgeon to understand the risks and benefits in their individual case.
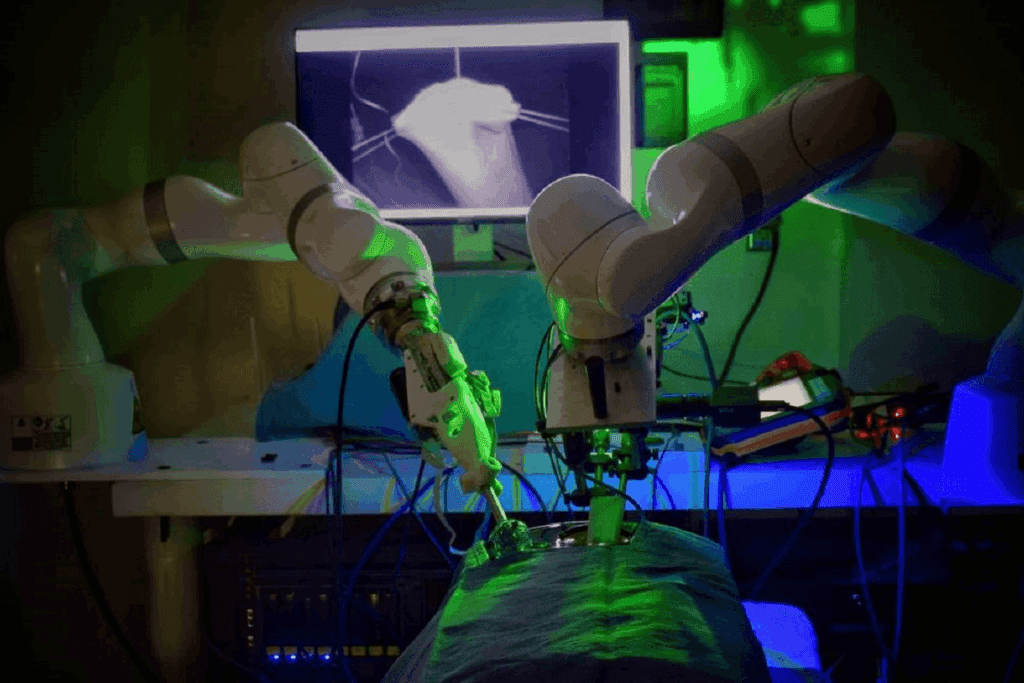
Robotic Hernia Repair: Advanced Surgical Technology
Robotic hernia repair represents a cutting-edge approach, offering enhanced precision and minimal invasiveness. This advanced surgical technology has been increasingly adopted in hernia repair surgeries due to its potential for improved outcomes.
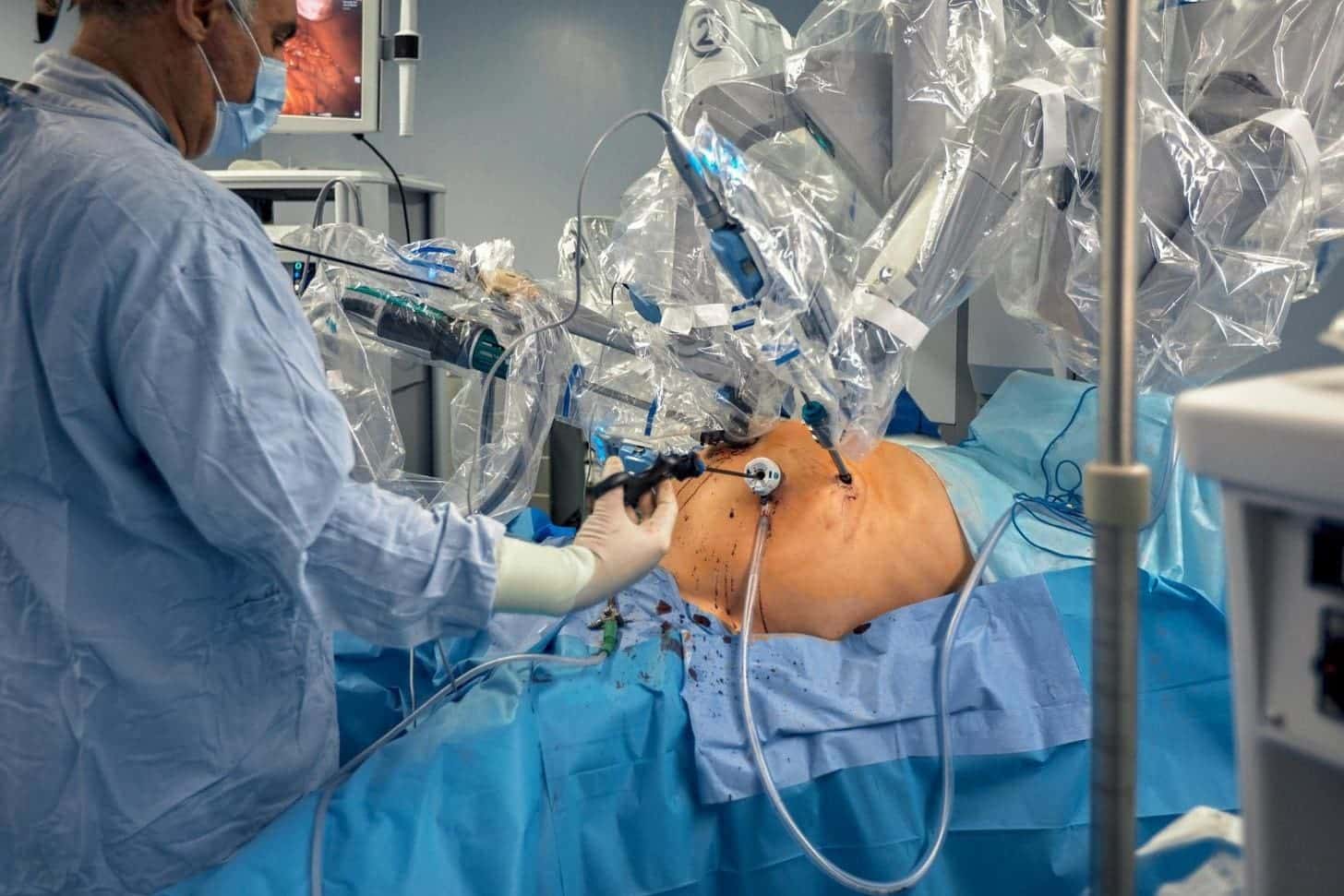
The Robotic Surgery Process
The robotic hernia repair process involves the use of a robotic system that allows surgeons to perform complex procedures with enhanced precision. The system includes a console where the surgeon sits and controls the robotic arms, a patient-side cart with the robotic arms, and a high-definition 3D vision system.
The procedure begins with the insertion of tiny incisions through which the robotic arms are guided. The surgeon then controls these arms from the console, manipulating tissues with great delicacy and precision, thereby facilitating a meticulous repair of the hernia.
Precision and Control Advantages
One of the significant advantages of robotic hernia repair is its ability to offer superior precision and control. The robotic system allows for a three-dimensional view of the operating area, enabling surgeons to identify and preserve vital structures more effectively.
The enhanced dexterity provided by the robotic arms allows for complex maneuvers in tight spaces, reducing the risk of damage to surrounding tissues. This precision contributes to a potentially lower rate of complications and a more effective repair.
Cost and Accessibility Factors
While robotic hernia repair offers several benefits, it also raises considerations regarding cost and accessibility. The robotic systems are expensive, and the cost is reflected in the overall expense of the surgery.
Additionally, not all hospitals or surgical centers have access to robotic technology, which can limit accessibility for some patients. However, as the technology becomes more widespread, these factors are likely to evolve.
Lichtenstein Technique: Gold Standard for Inguinal Hernias
The Lichtenstein technique, with its tension-free mesh repair, has revolutionized the treatment of inguinal hernias, setting a new standard in hernia surgery. This method has been widely adopted due to its simplicity, efficacy, and low recurrence rates.
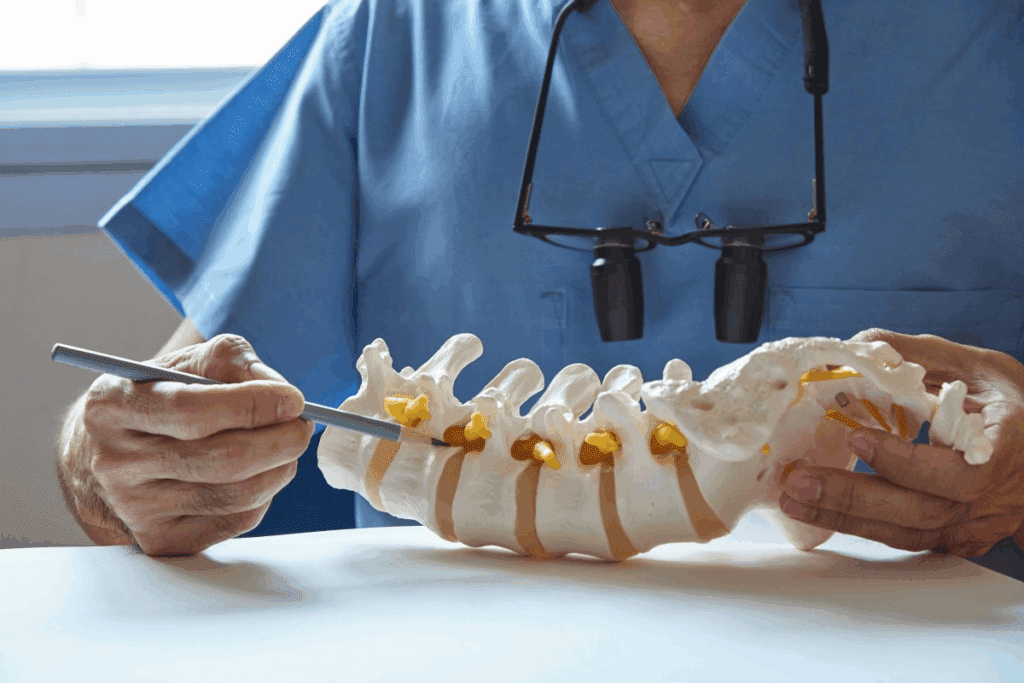
Procedure Details and Approach
The Lichtenstein technique involves an open repair approach where a synthetic mesh is placed over the hernial defect, reinforcing the posterior wall of the inguinal canal. This tension-free repair is key to its success, as it minimizes the risk of recurrence and reduces postoperative pain.
The procedure is typically performed under local anesthesia, allowing for a quicker recovery compared to more invasive surgeries. The mesh used is usually made of a lightweight, monofilament material that promotes tissue ingrowth, further securing the repair.
Success Rates and Outcomes
Studies have consistently shown that the Lichtenstein technique has high success rates, with low recurrence rates reported in long-term follow-ups. The technique’s tension-free design is a significant factor in its success, as it reduces the strain on the repair site.
Patient outcomes are generally favorable, with most experiencing minimal postoperative complications and a rapid return to normal activities. The Lichtenstein technique’s reliability has made it a preferred choice among surgeons for inguinal hernia repair.
Comparing to Other Techniques
When compared to other hernia repair techniques, the Lichtenstein technique stands out for its balance of simplicity and effectiveness. Laparoscopic techniques, while offering smaller incisions and potentially quicker recovery, may have higher recurrence rates if not performed by experienced surgeons.
The Lichtenstein technique’s use of mesh provides a durable repair that is less likely to recur, making it a gold standard against which other techniques are often compared. However, the choice of technique ultimately depends on the patient’s specific condition, the surgeon’s expertise, and other individual factors.
TEP and TAPP: Laparoscopic Approaches Compared
When it comes to laparoscopic hernia surgery, two approaches stand out: TEP and TAPP, each with its unique methodology and benefits. Laparoscopic hernia repair has become a preferred method due to its minimally invasive nature, leading to quicker recovery times and less postoperative pain.
Total Extraperitoneal Repair (TEP)
Total Extraperitoneal Repair (TEP) is a laparoscopic technique that involves accessing the hernia site without entering the abdominal cavity. This approach is known for reducing the risk of intra-abdominal complications.
- Key Benefits: Lower risk of bowel injury, less postoperative pain, and quicker recovery.
- Considerations: Requires advanced laparoscopic skills, and there’s a potential for difficulty in accessing the hernia site in some cases.
Transabdominal Preperitoneal Repair (TAPP)
Transabdominal Preperitoneal Repair (TAPP) is another laparoscopic technique that involves entering the abdominal cavity to access the preperitoneal space. This method allows for a more familiar anatomical approach for surgeons.
- Key Benefits: Easier access to the hernia site, ability to inspect the abdominal cavity, and potentially fewer complications related to mesh placement.
- Considerations: Higher risk of bowel injury compared to TEP, potential for adhesions, and the need for careful closure of the peritoneal incision.
Choosing Between TEP and TAPP
The choice between TEP and TAPP depends on several factors, including the surgeon’s expertise, the patient’s anatomy, and the specific characteristics of the hernia.
- Surgeon’s Expertise: The choice may be influenced by the surgeon’s familiarity and experience with either technique.
- Patient’s Anatomy: Anatomical considerations, such as previous surgeries or specific hernia characteristics, can influence the decision.
- Hernia Characteristics: The size, location, and complexity of the hernia can also play a role in choosing between TEP and TAPP.
Ultimately, both TEP and TAPP offer effective solutions for hernia repair, with the best approach determined on a case-by-case basis.
Best Hernia Treatment Options by Hernia Type
Different types of hernias require distinct treatment approaches to ensure the best outcomes. The type of hernia, its size, and the patient’s overall health are critical factors in determining the most appropriate surgical technique.
Inguinal Hernia Surgery Options
Inguinal hernias are the most common type of hernia and occur when tissue, such as part of the intestine, protrudes through a weak spot in the abdominal muscles. The Lichtenstein technique, a tension-free repair using mesh, is widely considered the gold standard for inguinal hernia repair due to its low recurrence rates and relatively straightforward procedure.
According to a study published in the Journal of the American College of Surgeons, the Lichtenstein technique has a recurrence rate of less than 1% in some cases.
“The Lichtenstein technique has become the preferred method for inguinal hernia repair due to its reliability and low complication rate,” states .
| Surgical Technique | Recurrence Rate | Recovery Time |
| Lichtenstein Technique | <1% | 1-2 weeks |
| Laparoscopic Repair | 1-2% | 1 week |
Ventral and Incisional Hernia Approaches
Ventral hernias occur in the abdominal wall, often at the site of a previous surgical incision, making them also known as incisional hernias. The treatment for ventral and incisional hernias often involves a more complex surgical approach, potentially including the use of mesh to reinforce the weakened area.
Laparoscopic ventral hernia repair is a minimally invasive technique that offers the advantage of smaller incisions and potentially quicker recovery times compared to open surgery. However, the choice between laparoscopic and open repair depends on the size and location of the hernia, as well as the patient’s health status.
Umbilical Hernia Repair Techniques
Umbilical hernias occur around the belly button and are more common in infants and adults with increased abdominal pressure. Surgical repair is often recommended for adults due to the low likelihood of spontaneous closure.
The surgical technique for umbilical hernia repair can vary, with options including open repair with or without mesh, and laparoscopic approaches. The choice of technique depends on the size of the hernia and the patient’s overall health.
Hiatal Hernia Surgical Management
Hiatal hernias occur when part of the stomach protrudes through the diaphragm into the chest cavity. Surgical management is typically reserved for patients with severe symptoms or complications. Laparoscopic Nissen fundoplication is a common surgical technique used to treat hiatal hernias, aiming to alleviate symptoms such as gastroesophageal reflux.
The decision to undergo surgery for a hiatal hernia should be made after careful consideration and consultation with a healthcare provider, as it involves wrapping the upper portion of the stomach around the lower portion of the esophagus to prevent reflux.
Mesh Types and Materials in Hernia Repair
The use of mesh in hernia repair has revolutionized the field, offering various types and materials to suit different patient needs. Mesh reinforcement is a critical component of hernia surgery, aimed at reducing the risk of recurrence and promoting healing.
Synthetic vs. Biological Mesh
Mesh materials can be broadly categorized into synthetic and biological types. Synthetic mesh, made from materials like polypropylene or polyester, is widely used due to its durability and effectiveness. On the other hand, biological mesh, derived from animal tissues, is often chosen for its biocompatibility and potential to promote tissue regeneration.
“The choice between synthetic and biological mesh depends on various factors, including the patient’s overall health, the type of hernia, and the surgeon’s preference,” notes a leading expert in hernia repair.
Permanent vs. Absorbable Options
Another important consideration is whether to use permanent or absorbable mesh. Permanent mesh remains in the body, providing ongoing support to the weakened area. In contrast, absorbable mesh is designed to degrade over time, potentially reducing the risk of long-term complications.
- Permanent mesh offers long-term reinforcement.
- Absorbable mesh may reduce the risk of chronic pain.
Mesh-Related Complications and Controversies
While mesh has significantly improved hernia repair outcomes, it is not without controversy. Complications such as mesh erosion, infection, and adhesion formation have been reported. The choice of mesh must be carefully considered to minimize these risks.
| Mesh Type | Advantages | Potential Complications |
| Synthetic | Durable, effective | Infection, adhesion |
| Biological | Biocompatible, promotes tissue regeneration | Higher cost, variable durability |
As the field of hernia repair continues to evolve, ongoing research and advancements in mesh technology are expected to address current limitations and improve patient outcomes.
Patient-Specific Factors in Surgical Selection
Patient-specific factors play a crucial role in determining the best surgical approach for hernia treatment. The decision-making process involves a comprehensive evaluation of individual characteristics to tailor the surgical technique to the patient’s unique needs.
Age and Health Considerations
The patient’s age and overall health status are significant factors in choosing the appropriate hernia surgery. Older patients or those with underlying health conditions may require a more conservative approach, while younger, healthier individuals might be candidates for more advanced techniques. For instance, laparoscopic surgery might be recommended for patients who are fit for general anesthesia and have a relatively simple hernia.
Health considerations also include the presence of comorbidities such as diabetes or heart disease, which can impact surgical outcomes and recovery. Careful preoperative evaluation is essential to minimize risks and ensure the best possible results.
Body Type and Anatomy
A patient’s body type and anatomy are critical in determining the most suitable surgical approach. For example, patients with a higher body mass index (BMI) might benefit from laparoscopic surgery due to reduced recovery time and less tissue trauma. Conversely, those with a slender build might be suitable for open repair with a mesh.
The anatomy of the hernia itself, including its size and location, also influences the choice of surgery. Surgeons must consider these factors to select the most appropriate technique, ensuring effective repair and minimizing the risk of complications.
Previous Surgeries and Comorbidities
Patients who have undergone previous surgeries, especially in the abdominal area, present unique challenges. Adhesions or scar tissue from prior operations can complicate both open and laparoscopic procedures. Surgeons must carefully plan the approach, potentially using imaging studies to assess the anatomy and identify potential difficulties.
The presence of comorbidities, such as chronic obstructive pulmonary disease (COPD) or cardiovascular disease, can also impact surgical decisions. These conditions may affect the patient’s ability to tolerate certain types of anesthesia or surgery, necessitating adjustments to the treatment plan.
Lifestyle and Occupational Factors
A patient’s lifestyle and occupational demands are also important considerations. Individuals with physically demanding jobs or those who engage in strenuous activities may benefit from a more durable repair method to prevent recurrence. Conversely, less invasive techniques might be suitable for patients with less physically demanding lifestyles.
Lifestyle factors, including smoking and nutritional status, can influence healing and recovery. Surgeons often counsel patients on optimizing these factors preoperatively to improve outcomes.
Comparing Recovery Times and Post-Operative Care
Post-operative care and recovery times vary considerably among the various hernia surgery techniques available. The choice of surgical method significantly impacts the patient’s recovery process, influencing factors such as hospital stay, return to normal activities, pain management, and long-term follow-up requirements.
Hospital Stay Duration
The length of hospital stay following hernia surgery depends on the type of surgical technique used. Laparoscopic and robotic surgeries typically result in shorter hospital stays, often allowing patients to be discharged on the same day or within 24 hours. In contrast, open hernia repair may require a longer hospital stay, sometimes extending to several days.
Return to Normal Activities
Recovery times also vary in terms of returning to normal activities. Patients who undergo minimally invasive surgeries generally resume their normal activities within a few days to a couple of weeks. Conversely, those who have open repair surgery may need several weeks to fully recover.
Pain Management Differences
Pain management is another critical aspect of post-operative care. Laparoscopic procedures are often associated with less post-operative pain compared to open repair. The use of mesh and the technique of mesh placement can also influence pain levels. Effective pain management strategies are tailored to the individual’s needs and the specifics of their surgery.
Long-term Follow-up Requirements
Long-term follow-up is essential for monitoring the success of the hernia repair and detecting any potential complications early. The frequency and nature of follow-up appointments can vary based on the surgical technique used and the patient’s overall health. A typical follow-up schedule might include check-ups at 1, 6, and 12 months post-surgery.
| Surgery Type | Hospital Stay | Return to Normal Activities | Pain Level |
| Laparoscopic | 0-1 day | 1-2 weeks | Low-Moderate |
| Open Repair | 1-3 days | 3-6 weeks | Moderate-High |
| Robotic | 0-1 day | 1-2 weeks | Low |
Emerging Innovations in Hernia Surgery
Emerging innovations are transforming the landscape of hernia surgery, offering improved recovery times and outcomes. The field is witnessing significant advancements in various techniques and technologies.
Robotic-Assisted Single-Incision Techniques
Robotic-assisted single-incision techniques represent a significant leap forward in hernia repair. These methods utilize advanced robotic systems to perform surgery through a single incision, minimizing visible scarring and potentially reducing recovery time. The precision offered by robotic systems allows for more complex repairs to be performed with greater ease.
Advanced Mesh Technologies
Advanced mesh technologies are being developed to reduce complications associated with traditional mesh materials. New meshes are designed to be more biocompatible, reducing the risk of adverse reactions and improving integration with the body’s tissues. Biological meshes, derived from natural tissues, are one such innovation, offering the potential for better healing and reduced risk of long-term complications.
Tissue Engineering Approaches
Tissue engineering represents a promising frontier in hernia repair. This approach involves using the patient’s own cells to generate tissue that can be used to repair hernias, potentially eliminating the need for synthetic materials. Tissue-engineered solutions could significantly reduce the risk of recurrence and complications associated with traditional repair methods.
Minimally Invasive Advancements
Minimally invasive surgery continues to evolve, with advancements in laparoscopic techniques and instrumentation. New instruments and methods are being developed to make these procedures even less invasive, further reducing recovery times and improving patient outcomes.
| Innovation | Description | Potential Benefits |
| Robotic-Assisted Surgery | Utilizes robotic systems for precise hernia repair | Reduced recovery time, less scarring |
| Advanced Mesh Technologies | New mesh materials for better biocompatibility | Reduced risk of complications, improved healing |
| Tissue Engineering | Uses patient’s cells to generate repair tissue | Potential elimination of synthetic materials, reduced recurrence |
Evaluating Hernia Surgery Success Rates
Understanding the factors that influence hernia surgery success rates can help patients make informed decisions about their treatment options.
The success of hernia surgery is multifaceted, involving various factors such as recurrence rates, quality of life outcomes, and cost-effectiveness. Evaluating these aspects is crucial for determining the best surgical approach for different types of hernias.
Recurrence Rate Comparisons
One of the primary measures of hernia surgery success is the recurrence rate. Different surgical techniques have varying recurrence rates.
- Laparoscopic repair tends to have lower recurrence rates compared to open repair.
- The use of mesh significantly reduces recurrence rates.
- Robotic hernia repair is also showing promising results with low recurrence rates.
Quality of Life Outcomes
Quality of life after hernia surgery is another critical factor in evaluating success. This includes:
- Pain levels post-surgery.
- Return to normal activities.
- Patient satisfaction.
Laparoscopic and robotic surgeries generally offer quicker recovery times and less post-operative pain, enhancing patient satisfaction and quality of life.
Complication Profiles by Technique
Different surgical techniques have unique complication profiles. For instance:
- Open repair may have a higher risk of wound infections.
- Laparoscopic repair can have complications related to the insertion of trocars.
- Robotic repair, while precise, can be associated with higher costs and longer operating times.
Cost-Effectiveness Analysis
Evaluating the cost-effectiveness of hernia surgery involves considering both the direct costs (such as surgical fees and hospital stays) and indirect costs (such as lost productivity due to recovery time).
While laparoscopic and robotic surgeries may have higher upfront costs, their quicker recovery times can make them more cost-effective in the long run.
Conclusion: Making an Informed Decision About Hernia Surgery
Making an informed decision about hernia surgery requires a thorough understanding of the various hernia surgery options available and their implications. By considering individual factors and the characteristics of different surgical techniques, patients can choose the best hernia treatment approach for their specific needs.
Throughout this article, we have explored the different types of hernias, the various surgical techniques, and the factors that influence the choice of surgery. Understanding these elements is crucial for patients to make an informed decision that aligns with their health goals and lifestyle.
Ultimately, the key to successful hernia surgery lies in selecting the most appropriate technique based on the type of hernia, the patient’s overall health, and other individual factors. By doing so, patients can minimize the risk of complications and ensure a smooth recovery.
FAQ
What are the most common types of hernias that require surgery?
The most common types of hernias that require surgery are inguinal hernias, umbilical hernias, and ventral hernias. Inguinal hernias occur when tissue protrudes through a weak spot in the abdominal muscles in the groin area. Umbilical hernias occur around the belly button, while ventral hernias occur in the abdominal wall.
What is the difference between open and laparoscopic hernia surgery?
Open hernia surgery involves making a single incision in the abdomen to repair the hernia, whereas laparoscopic hernia surgery involves making several small incisions and using a camera and instruments to repair the hernia. Laparoscopic surgery is considered minimally invasive and often results in less pain and quicker recovery.
What is robotic hernia repair, and how does it differ from traditional laparoscopic surgery?
Robotic hernia repair is a type of laparoscopic surgery that uses a robotic system to enhance the surgeon’s capabilities. It provides high-definition 3D visualization, precise dissection, and suturing. The robotic system allows for more precise and delicate movements, which can be beneficial for complex hernia repairs.
What is the Lichtenstein technique, and is it still considered a gold standard for inguinal hernia repair?
The Lichtenstein technique is a type of open hernia repair that involves placing a mesh patch over the weakened area to reinforce it. It is still considered a gold standard for inguinal hernia repair due to its high success rates and low recurrence rates.
What are the differences between TEP and TAPP laparoscopic hernia repair techniques?
TEP (Total Extraperitoneal Repair) and TAPP (Transabdominal Preperitoneal Repair) are both laparoscopic techniques used to repair inguinal hernias. TEP involves approaching the hernia from behind the abdominal wall without entering the abdominal cavity, while TAPP involves entering the abdominal cavity to access the hernia. The choice between TEP and TAPP depends on the surgeon’s preference and the patient’s specific condition.
What types of mesh are used in hernia repair, and what are their advantages and disadvantages?
There are several types of mesh used in hernia repair, including synthetic mesh, biological mesh, permanent mesh, and absorbable mesh. Synthetic mesh is durable and long-lasting, but may cause complications such as adhesions or chronic pain. Biological mesh is derived from animal tissue and is often used for complex or contaminated hernias. Permanent mesh remains in the body forever, while absorbable mesh is designed to be absorbed by the body over time.
How do patient-specific factors influence the selection of hernia surgery?
Patient-specific factors such as age, health status, body type, previous surgeries, and lifestyle or occupational factors can influence the selection of hernia surgery. For example, older patients or those with underlying health conditions may require a more conservative approach, while younger patients may be candidates for more minimally invasive techniques.
What are the recovery times and post-operative care requirements for different hernia surgery techniques?
Recovery times and post-operative care requirements vary depending on the type of hernia surgery. Laparoscopic and robotic surgeries often result in quicker recovery times and less post-operative pain compared to open surgery. However, the specific recovery plan will depend on the individual patient’s condition and the surgeon’s instructions.
What are some emerging innovations in hernia surgery?
Emerging innovations in hernia surgery include robotic-assisted single-incision techniques, advanced mesh technologies, tissue engineering approaches, and advancements in minimally invasive surgery. These innovations aim to improve outcomes, reduce recovery times, and minimize complications.
How is the success of hernia surgery evaluated, and what are the key metrics used to compare different techniques?
The success of hernia surgery is evaluated based on recurrence rates, quality of life outcomes, complication profiles, and cost-effectiveness analysis. These metrics help compare different techniques and determine the most effective approach for individual patients.
Reference:
PMC Article: Comparison and Standardisation of Various Open Preperitoneal Techniques. https://pmc.ncbi.nlm.nih.gov/articles/PMC11961359/