Endometriosis affects millions of women worldwide, causing chronic pelvic pain. This pain can greatly impact daily life. Managing this condition requires a complete approach, with pain relief being a key part of treatment. Review of the best pain reliever for endometriosis symptoms and long-term management.
Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen are often suggested first. They help with mild to moderate endometriosis pain. But, finding the best pain reliever for you means knowing your options and talking to a trusted healthcare provider.
At Liv Hospital, we know how hard it is to live with endometriosis. We’re dedicated to giving patient-centered care. This care combines proven methods with caring support.
Key Takeaways
- Endometriosis is a chronic condition that needs a full management plan.
- NSAIDs are often suggested for mild to moderate endometriosis pain.
- Knowing your treatment options is key for effective pain relief.
- Working with a trusted healthcare provider helps find the best pain reliever for you.
- Liv Hospital offers patient-centered care for endometriosis management.
Understanding Endometriosis and Its Pain Symptoms

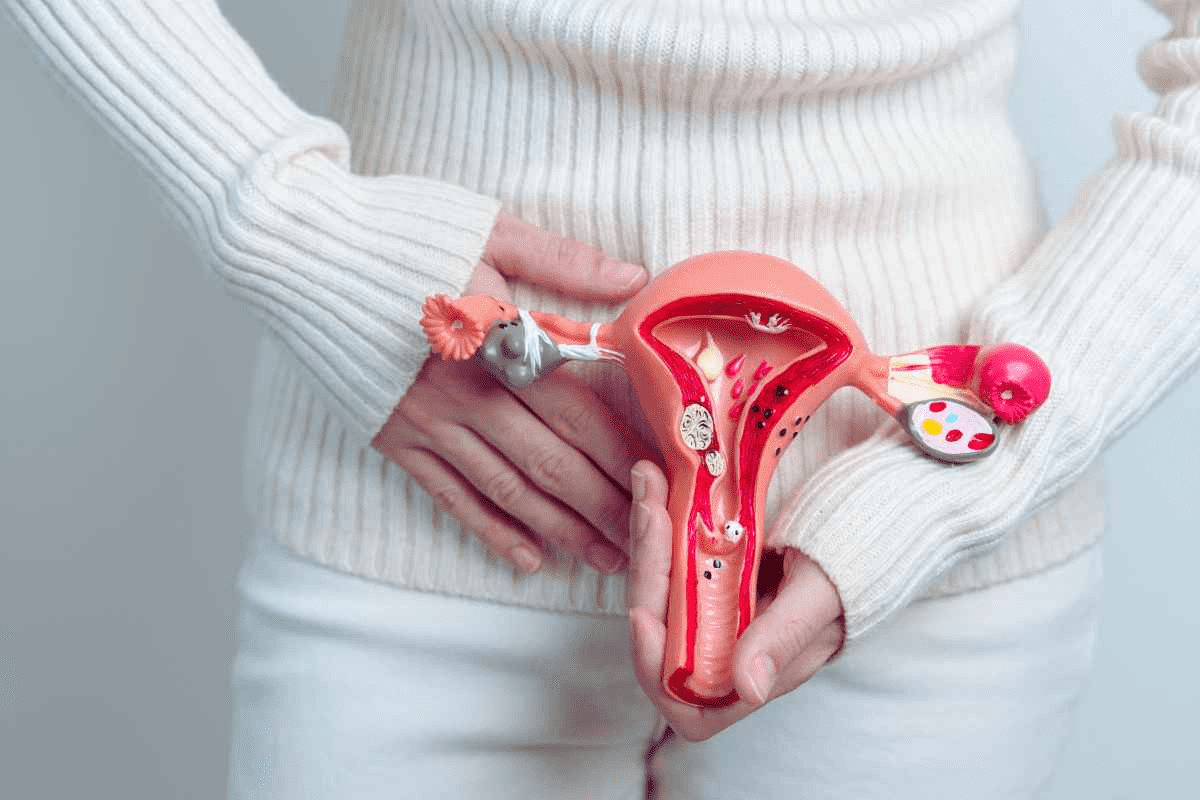
It’s important to know about endometriosis pain to manage it better. This condition happens when tissue like the uterine lining grows outside the uterus. It causes chronic pelvic pain, mostly during menstruation.
To tackle endometriosis pain, understanding its causes and how it affects people is key. Your doctor will ask about your symptoms and health history. Keeping a pain journal can help diagnose and understand your condition.
What Causes Endometriosis Pain
Endometriosis pain comes from tissue growing outside the uterus. This tissue bleeds and thickens with each cycle, causing inflammation and scarring. The pain’s severity varies based on the tissue’s location, size, and depth.
Common Pain Symptoms and Patterns
Common symptoms of endometriosis include:
- Chronic Pelvic Pain: Persistent pain in the pelvic area, from mild to severe.
- Dysmenorrhea: Painful menstruation, often felt as cramping.
- Dyspareunia: Pain during sexual intercourse.
- Dysuria: Painful urination, worse during menstruation.
- Lower Back Pain: Some people experience lower back pain, mainly during their period.
The Role of Prostaglandins in Endometriosis Pain
Prostaglandins are key in endometriosis pain. They make the uterus contract, causing cramps and pain. People with endometriosis often have more prostaglandins, making their pain worse. Knowing this helps find treatments like NSAIDs, which reduce prostaglandin production.
Over-the-Counter NSAIDs: The First Line of Defense
[Add image here]
Many women start with over-the-counter NSAIDs to ease endometriosis symptoms. These drugs are often the first choice for mild to moderate pain.
How NSAIDs Work Against Endometriosis Pain
NSAIDs cut down on prostaglandins, which cause the uterus to contract and lead to pain. They block the cyclooxygenase (COX) enzyme. This reduces prostaglandin levels, easing pain and swelling.
Ibuprofen (Advil, Motrin) for Endometriosis
Ibuprofen is a top pick for endometriosis pain. It comes in different strengths and types, like extended-release. For endometriosis, take 400 to 800 mg every 8 hours as needed.
Naproxen Sodium (Aleve) for Endometriosis
Naproxen sodium is also good for endometriosis pain. It lasts longer than ibuprofen, giving longer relief. Take 250 to 500 mg twice a day.
Proper Dosing and Timing for Maximum Effect
To get the most from NSAIDs, stick to the recommended doses. Take them when pain starts or before expected cramps. Taking them regularly helps manage pain better.
Key Considerations:
- Always follow the recommended dosage on the label or as directed by your healthcare provider.
- Be aware of possible side effects, like stomach issues, and talk to your doctor about them.
- If your pain doesn’t get better or gets worse, see your healthcare provider for advice.
Best Pain Reliever for Endometriosis: Prescription Options
When over-the-counter options aren’t enough, prescription medications can provide significant relief for endometriosis pain. For women with more severe symptoms, these stronger pain relievers can be a key part of their pain management plan.
Prescription-Strength NSAIDs
Prescription-strength NSAIDs offer a more potent version of the over-the-counter medications many are familiar with. These include higher doses of ibuprofen or naproxen, which can be more effective for managing severe endometriosis pain. It’s essential to follow the prescribed dosage carefully to minimize side effects.
COX-2 Inhibitors
COX-2 inhibitors are a specific class of NSAIDs that target the COX-2 enzyme, reducing inflammation and pain. They are useful for women who experience gastrointestinal side effects from traditional NSAIDs. Celecoxib (Celebrex) is a commonly prescribed COX-2 inhibitor for endometriosis pain.
Comparing Effectiveness of Different Pain Medications
When comparing the effectiveness of different pain medications for endometriosis, several factors come into play. The table below summarizes some key points to consider:
| Medication Type | Effectiveness for Endometriosis | Common Side Effects |
|---|---|---|
| Prescription-Strength NSAIDs | Highly effective for inflammation and pain | Gastrointestinal issues, increased risk of bleeding |
| COX-2 Inhibitors | Effective for pain relief with fewer GI side effects | Increased risk of cardiovascular events, potentially kidney issues |
Potential Side Effects and Management
While prescription pain relievers can be highly effective, they also come with side effects. Managing these side effects is key for maintaining quality of life. For instance, taking medication with food can help reduce gastrointestinal issues. Regular check-ups with your healthcare provider can help monitor for any adverse effects.
Key Considerations:
- Always follow the prescribed dosage.
- Report any side effects to your healthcare provider.
- Consider combining medication with other pain management strategies.
For more severe pain not controlled by NSAIDs and hormonal birth control, GnRH analogues have shown effectiveness. Studies show over 80 percent pain reduction in women using this treatment. Your healthcare provider can help determine if this is a suitable option for you.
Hormonal Birth Control for Endometriosis Pain Management
Hormonal birth control is a common treatment for endometriosis pain. It helps by controlling or stopping menstrual cycles. This can lessen or stop the pain caused by endometriosis.
Combined Hormonal Contraceptives (Estrogen and Progestin)
Combined hormonal contraceptives, which have both estrogen and progestin, help reduce endometriosis pain. They prevent ovulation and slow down the growth of endometrial tissue.
Doctors say, “The use of combined hormonal contraceptives can significantly reduce the symptoms of endometriosis. This improves the quality of life for many women.”
“Hormonal treatments are often the first-line therapy recommended for endometriosis. They offer a viable solution for pain management.”
Continuous vs. Cyclic Dosing Strategies
Hormonal birth control can be taken continuously or cyclically. Continuous dosing means taking the contraceptive without a break. This might make it more effective in managing endometriosis pain.
A study showed that continuous dosing can help some women manage their pain better. Here’s a comparison of the two methods:
| Dosing Strategy | Description | Potential Benefits |
|---|---|---|
| Cyclic Dosing | Traditional dosing with a placebo week | Mimics natural menstrual cycle |
| Continuous Dosing | Dosing without a placebo week | Potential for improved pain management |
Expected Timeline for Pain Relief
Patients usually start feeling pain relief in a few months after starting hormonal birth control. But, the exact time can vary. It depends on the individual and the treatment.
It’s essential for patients to work closely with their healthcare provider to find the best approach. They should also adjust the treatment plan as needed.
Managing Side Effects of Hormonal Treatments
Hormonal birth control can be effective but has side effects. Common ones include nausea, breast tenderness, and mood changes. To manage these, the type or dose of the contraceptive might need to be adjusted.
- Monitoring side effects and adjusting treatment
- Considering alternative hormonal contraceptives
- Lifestyle changes to mitigate side effects
Progestin-Only Treatments for Endometriosis
Progestin-only contraceptives are now seen as effective for easing endometriosis pain. They are a good choice for women who want to avoid estrogen.
The Mini-Pill for Daily Management
The mini-pill is a daily pill that helps manage endometriosis symptoms. It makes the uterus lining thinner, cuts down on bleeding, and eases pain. It’s important to take it every day for it to work well.
Depo-Provera Injections
Depo-Provera is a shot given every three months. It helps with pain by stopping menstruation in many women. But, it can cause weight gain and lower bone density.
Progestin-Releasing IUDs (Mirena, Skyla)
Progestin-releasing IUDs like Mirena and Skyla deliver progestin directly to the uterus. They last 5-7 years and reduce bleeding and pain.
Comparing Effectiveness for Different Symptoms
Each progestin-only treatment works better for different symptoms. The table below shows the benefits and side effects of each option.
| Treatment | Administration | Effectiveness for Pain Relief | Common Side Effects |
|---|---|---|---|
| Mini-Pill | Daily oral | High | Irregular bleeding, mood changes |
| Depo-Provera | Every 3 months injection | High | Weight gain, bone density loss |
| Mirena IUD | Intrauterine device (up to 7 years) | High | Spotting, cramping during insertion |
| Skyla IUD | Intrauterine device (up to 3 years) | High | Spotting, cramping during insertion |
Choosing a progestin-only treatment depends on many factors. These include symptom severity, future fertility plans, and side effect tolerance. Talking to a healthcare provider is key to finding the right option.
GnRH Analogues for Severe Endometriosis Pain
GnRH analogues can help women with severe endometriosis pain when other treatments don’t work. These medications are effective in managing symptoms, even when other treatments fail.
How GnRH Treatments Work
GnRH analogues first increase estrogen levels. But, they then lower estrogen production. This decrease makes the endometriosis tissue shrink, reducing pain. Over 80% of women using GnRH analogues see a pain reduction.
Injectable and Nasal Spray Options
GnRH analogues come in injectable and nasal spray forms. Injectables like leuprolide acetate are given every 1-3 months. Nasal sprays, such as nafarelin, are used twice daily. The choice depends on what the patient prefers and what insurance covers.
Managing Side Effects of GnRH Therapy
GnRH analogues can cause side effects like hot flashes and vaginal dryness. Healthcare providers suggest lifestyle changes and other treatments to help manage these.
Add-Back Therapy to Reduce Side Effects
Add-back therapy uses estrogen and/or progesterone with GnRH analogues. This helps lessen side effects without reducing treatment effectiveness. It improves quality of life for women on GnRH therapy.
Understanding GnRH analogues and their side effects helps women with severe endometriosis pain. Working with a healthcare provider is key to finding the right treatment and managing side effects.
When to Consider Surgical Options for Pain Relief
If endometriosis pain doesn’t go away with other treatments, surgery might be next. For women who haven’t found relief, surgery can greatly reduce pain and improve life quality.
Laparoscopic Excision Surgery
Laparoscopic excision surgery is a minimally invasive method. It removes endometrial lesions with great precision. This approach is chosen for its effectiveness in removing bad tissue while keeping healthy tissue intact.
The surgery is done under general anesthesia. A laparoscope is used to see inside the pelvic area. The aim is to remove as much of the endometrial growths as possible, which can greatly lessen pain.
Ablation Procedures
Ablation procedures destroy endometrial tissue instead of removing it. Methods like laser ablation or electrosurgical ablation are used to vaporize or destroy the implants.
Though effective, ablation is less precise than excision surgery. It doesn’t allow for tissue removal for examination. Yet, it can offer significant pain relief for many women.
Post-Surgical Pain Management
Managing pain after surgery is key for recovery. Post-surgical pain management may include NSAIDs and hormonal treatments. These help control pain and prevent adhesions or recurrence.
Following your healthcare provider’s post-operative care instructions is vital. This includes rest, activity level, and follow-up appointments.
Combining Surgery with Medical Treatments
For the best results, surgery is often paired with medical treatments. Hormonal therapies or other medications may be started or continued after surgery. This helps manage any remaining symptoms and prevent recurrence.
Using both surgical and medical approaches creates a more complete treatment plan. It addresses immediate pain relief and long-term endometriosis management.
Non-Pharmaceutical Pain Relief Strategies
There are many ways to ease endometriosis pain without medicine. These methods can work alongside traditional treatments to manage pain better.
Heat Therapy and Cold Packs
Heat or cold on the lower abdomen can lessen endometriosis pain. Heat, like a heating pad or warm bath, relaxes muscles and boosts blood flow. This can help reduce pain. Cold packs, on the other hand, can cut down inflammation and dull pain.
Benefits of Heat Therapy:
- Relaxes uterine muscles
- Increases blood flow
- Reduces cramping
Benefits of Cold Therapy:
- Reduces inflammation
- Numbs the pain
- Decreases muscle spasms
TENS Units for Endometriosis Pain
TENS units are small devices that send electrical impulses to nerves. This interrupts pain signals to the brain. They are great for managing menstrual cramps and other endometriosis pain.
Pelvic Floor Physical Therapy
Pelvic floor physical therapy strengthens and relaxes pelvic muscles. It can lessen pain and boost pelvic health.
| Therapy Type | Benefits |
|---|---|
| Pelvic Floor Physical Therapy | Reduces pain, improves pelvic health |
| Heat Therapy | Relaxes muscles, increases blood flow |
| Cold Therapy | Reduces inflammation, numbs pain |
| TENS Therapy | Interrupts pain signals to the brain |
Complementary Pain Management Approaches
Many complementary therapies can help with endometriosis pain. These include acupuncture, yoga, and mindfulness meditation. They aim to reduce stress and enhance well-being.
Complementary Therapies:
- Acupuncture
- Yoga
- Mindfulness Meditation
Adding these non-medical pain relief strategies to your treatment plan can offer more relief. It can also improve your life quality.
Dietary Changes and Supplements for Pain Management
Managing endometriosis pain can be helped by changing what you eat and taking supplements. These steps can lessen your symptoms and boost your health.
Anti-Inflammatory Diet Principles
Eating foods that fight inflammation can help with endometriosis. More fiber in your diet can cut estrogen levels by 10% to 25%. This can make your symptoms better. Good sources of fiber are whole grains, legumes, and colorful veggies.
“Eating whole, nutrient-rich foods is a strong way to manage endometriosis pain,” says a top expert in treating endometriosis.
Omega-3 Fatty Acids and Fish Oil
Omega-3 fatty acids, found in fish oil, may lower endometriosis risk. These fats fight inflammation and pain. You can get them from fatty fish like salmon or from high-quality fish oil supplements.
Turmeric and Other Natural Anti-Inflammatories
Turmeric has curcumin, a strong anti-inflammatory. Research shows it can lessen inflammation and pain from endometriosis. Ginger, cinnamon, and boswellia are also good for fighting inflammation.
- Turmeric/Curcumin
- Ginger
- Cinnamon
- Boswellia
Vitamin and Mineral Supplements
Some vitamins and minerals can help with endometriosis symptoms. Vitamin D fights inflammation, and magnesium relaxes muscles and eases pain. Always talk to a doctor before starting new supplements to make sure they’re right for you.
By changing your diet and using the right supplements, people with endometriosis can feel less pain and live better lives.
Creating a Pain Management Plan
Creating a personalized pain management plan can greatly improve life for those with endometriosis. It should fit the individual’s needs, considering the disease’s extent, pain severity, and pregnancy plans.
Tracking Pain Patterns and Triggers
To make an effective pain management plan, tracking pain patterns and triggers is key. Your healthcare team might ask you to keep a journal of your pain and symptoms. This helps describe how pain affects your daily life.
By monitoring symptoms, you can spot patterns and triggers. This allows for more focused treatments.
Combining Multiple Approaches
A good pain management plan uses many methods. This might include medicines, lifestyle changes, and alternative therapies. A multi-faceted approach can help manage endometriosis symptoms best.
For example, you might use over-the-counter pain relievers with hormonal treatments and dietary changes.
Working with Your Healthcare Team
It’s vital to work closely with your healthcare team for a successful pain management plan. They can guide you through treatment options, track your progress, and adjust plans as needed. Regular talks with your healthcare team keep your plan effective and tailored to your changing needs.
When to Seek Emergency Medical Help
Knowing when to seek emergency medical help is important when managing endometriosis pain. Severe symptoms like heavy bleeding, intense pain, or signs of infection need immediate care. Being aware of these signs ensures your safety and well-being.
Conclusion: Finding Your Endometriosis Pain Relief Solution
Finding relief from endometriosis pain needs a plan made just for you. This plan should include medical treatments, lifestyle changes, and other therapies. We’ve looked at many options, like over-the-counter NSAIDs and prescription drugs.
Hormonal birth control and surgery are also choices. Everyone reacts differently to these treatments. Some people find relief with non-hormonal methods too.
Working with your healthcare team is key. Together, you can create a pain management plan that fits you. This plan will help you manage your pain better.
Managing endometriosis pain is a process of trying different things. Keep track of when and why you feel pain. Be open to trying different methods to find what works best for you. With the right approach, you can live a better life and find relief from endometriosis pain.
FAQ
What are the best pain relievers for endometriosis?
For endometriosis, over-the-counter NSAIDs like ibuprofen and naproxen are good. Prescription meds and hormonal treatments also help. The best one depends on your symptoms and health history.
How do NSAIDs work to relieve endometriosis pain?
NSAIDs cut down on prostaglandins. These substances make the uterus contract and cause pain. So, NSAIDs help ease endometriosis pain.
What is the role of prostaglandins in endometriosis pain?
Prostaglandins make the uterus contract, causing pain. Cutting down on them with NSAIDs or other treatments can help reduce this pain.
Can hormonal birth control help manage endometriosis pain?
Yes, hormonal birth control can help. It includes combined and progestin-only treatments. These regulate hormones and reduce prostaglandins, easing pain.
What are the benefits of progestin-releasing IUDs for endometriosis pain management?
Progestin-releasing IUDs, like Mirena and Skyla, offer long-term pain relief. They release progestin, which cuts down prostaglandins and eases symptoms.
How do GnRH analogues work to relieve endometriosis pain?
GnRH analogues lower estrogen, causing endometriosis tissue to shrink and pain to decrease. But, they can have side effects. Add-back therapy may be needed to lessen these.
What are some non-pharmacological pain relief strategies for endometriosis?
Non-medical strategies include heat therapy, cold packs, and TENS units. Pelvic floor physical therapy and acupuncture also help. Mindfulness techniques are another option.
Can dietary changes help manage endometriosis pain?
Yes, changing your diet can help. Eating anti-inflammatory foods like fruits, veggies, and whole grains can reduce symptoms. Omega-3 fatty acids and natural anti-inflammatories also help.
How can I create a pain management plan for endometriosis?
To manage pain, track your symptoms and triggers. Use a mix of meds, lifestyle changes, and alternative therapies. Work with your healthcare team to find what works best for you.
When should I seek emergency medical help for endometriosis pain?
Seek emergency help for severe pain, heavy bleeding, or other concerning symptoms. Your healthcare team can help decide the best action for your situation.
References
National Center for Biotechnology Information. Endometriosis Pain Relief: A Comprehensive Management Approach. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC11724681/