Beta thalassemia major is a genetic disorder that leads to chronic anemia. This causes the bone marrow to work too hard. As a result, it creates distinct facial features.
One of these features is chipmunk facies. It includes prominent cheekbones, a depressed nasal bridge, and a protruding upper jaw.
These facial changes happen because the bone marrow expands. This is an attempt to make up for the lack of red blood cells. Getting blood transfusions early is key to preventing or lessening these bone deformities.
Key Takeaways
- Beta thalassemia major causes distinct facial abnormalities due to bone marrow overactivity.
- Characteristic features include prominent cheekbones, depressed nasal bridge, and protruding upper jaw.
- Early blood transfusions are key in preventing or reducing bone deformities.
- Liv Hospital’s patient-centered approach transforms outcomes for those living with these conditions.
- Understanding the effects of beta thalassemia major on facial structure is essential for effective management.
Understanding Beta Thalassemia Major

Beta thalassemia major comes from mutations in the HBB gene. This gene is responsible for the beta-globin subunit of hemoglobin. The condition leads to less or no beta-globin chains, causing severe anemia and other issues.
Genetic Basis of Beta Thalassemia
Beta thalassemia major is caused by HBB gene mutations on chromosome 11. These mutations can reduce or eliminate beta-globin chains. The condition’s severity depends on the mutation type and whether an individual has two copies of the mutation.
Pathophysiology and Chronic Anemia
The condition’s pathophysiology involves ineffective erythropoiesis and chronic anemia. Without beta-globin chains, alpha-globin chains build up and harm red blood cells. This causes their early destruction, leading to severe anemia.
Chronic anemia requires regular blood transfusions. It also causes bone deformities and growth issues.
Global Prevalence and Demographics
Beta thalassemia major is common in areas where malaria was once prevalent, like the Mediterranean, Middle East, and South Asia. Migration has spread it to North America and Europe. It has a significant global presence, with high carrier rates in some populations.
| Region | Prevalence | Carrier Frequency |
| Mediterranean | High | 1 in 7 to 1 in 30 |
| Middle East | High | 1 in 5 to 1 in 20 |
| South Asia | High | 1 in 10 to 1 in 30 |
| North America | Low to Moderate | 1 in 20 to 1 in 50 |
| Europe | Low to Moderate | 1 in 30 to 1 in 60 |
The Beta Thalassemia Major Face: Clinical Overview

The beta thalassemia major face shows specific changes due to the disease’s pathophysiology.
Beta thalassemia major, or Cooley’s anemia, is a severe form of thalassemia. It greatly affects the quality of life of those who have it. The disease causes chronic anemia, which means patients need regular blood transfusions.
Definition and Medical Significance
The term “beta thalassemia major face” describes the unique facial features of patients with untreated or poorly treated beta thalassemia major. These features come from bone marrow expansion due to ineffective erythropoiesis.
Chipmunk facies is what these patients’ faces are called. It’s marked by big cheekbones, a sunken nasal bridge, and a sticking-out upper jaw.
When Facial Changes Typically Develop
Facial changes in beta thalassemia major start to show in early childhood. This usually happens between 2 and 6 years old as the disease gets worse and anemia increases.
A clinical expert said, “Early diagnosis and treatment can greatly change the disease’s course. It can also lessen the severity of facial changes.”
“The facial deformities linked to beta thalassemia major are a big worry for patients and their families. They affect not just physical health but also mental well-being.”
Relationship to Disease Severity
The severity of facial changes depends on the disease’s severity and treatment. Patients who get regular blood transfusions and iron chelation therapy are less likely to have severe facial deformities.
A study in a well-known medical journal showed that “effective management of beta thalassemia major can stop or lessen the appearance of typical facial features.”
This shows how important early diagnosis and proper management of beta thalassemia major are.
Pathophysiology Behind Chipmunk Facies
The chipmunk facies comes from a mix of bone marrow activity and poor red blood cell making. In beta thalassemia major, the body can’t make enough hemoglobin. This leads to long-term anemia and the body tries to fix it in many ways.
Bone Marrow Hyperactivity Mechanism
Bone marrow gets busier to make up for the anemia in beta thalassemia major. It tries to make more red blood cells. This makes the bone marrow grow, causing bony changes like chipmunk facies.
The body makes more erythropoietin to help make red blood cells. But in beta thalassemia major, this doesn’t work well because of a genetic problem with hemoglobin.
Ineffective Erythropoiesis
In beta thalassemia major, the bone marrow makes bad or short-lived red blood cells. This makes the body keep making more erythropoietin and the bone marrow gets bigger.
- More erythropoietin makes the bone marrow work harder.
- The bone marrow gets bigger, causing bone changes.
- Bad red blood cells keep the anemia going.
Skeletal Response to Chronic Anemia
The bones try to help by making more red blood cells. This leads to bone deformities. The bone marrow growing in the face bones causes the chipmunk facies.
The face changes include prominent cheekbones and a depressed nasal bridge. These changes happen because the body is trying to fix the blood problem.
In summary, chipmunk facies in beta thalassemia major comes from bone marrow activity, bad red blood cell making, and bone changes due to anemia. Knowing how these work together helps in managing the condition and its effects on the face.
7 Characteristic Features of Thalassemia Chipmunk Facies
The term ‘thalassemia chipmunk facies’ refers to facial changes seen in beta-thalassemia major. These changes come from bone marrow activity and ineffective blood cell production. They lead to noticeable facial structure changes.
Prominent Cheekbones (Malar Prominence)
One key feature is the prominent cheekbones, or malar prominence. This happens because the bone marrow in the face grows, making the cheekbones bigger and stick out more.
Depressed Nasal Bridge
A depressed nasal bridge is another sign. It’s caused by bone marrow growth in the face, pushing the nasal bridge down.
Protruding Upper Jaw (Maxillary Hypertrophy)
Maxillary hypertrophy, or the upper jaw sticking out, is a big feature. It’s due to the maxillary bone growing too much because of bone marrow activity.
Frontal Bossing
Frontal bossing, or a big forehead, is common too. It’s caused by the frontal bone marrow expanding, making the forehead stick out more.
These features show how beta-thalassemia major affects the face. Knowing about them is key for managing and treating this condition.
Additional Bone Deformities in Beta Thalassemia
Beta thalassemia major can cause more than just the chipmunk facies. It affects bone marrow and leads to other bone deformities. This is because the body tries to make up for chronic anemia.
Spinal and Rib Abnormalities
Spinal and rib issues are common in beta thalassemia major. Bone marrow expands to help with anemia, causing:
- Vertebral body collapse
- Rib deformities
- Kyphosis or scoliosis
| Spinal Abnormality | Description | Potential Complications |
| Vertebral Body Collapse | Collapse of the vertebral bodies due to bone marrow expansion | Back pain, spinal instability |
| Rib Deformities | Deformation of the ribs due to marrow expansion | Respiratory issues, pain |
Limb Deformities
Limb issues in beta thalassemia major come from bone marrow growth and thin bones. This can cause:
- Pathological fractures
- Cortical thinning
- Deformities in the long bones
Growth Retardation and Delayed Development
Beta thalassemia major can slow down growth and development in kids. Chronic anemia and bone marrow growth can lead to:
- Delayed puberty
- Short stature
- Growth retardation
Regular treatment and management are key to reduce these effects. They help improve the life quality of those affected.
Functional Impacts of Thalassemia Facial Features
Thalassemia facial features can greatly affect the lives of those with beta thalassemia major. These facial changes can cause many challenges in daily life. They can also impact a person’s overall well-being.
Effects on Chewing and Eating
The facial changes from beta thalassemia major, like a bigger upper jaw, can change how we eat. These changes can make chewing and eating hard. This is because the teeth and jaw might not work right.
Patients might feel pain or discomfort when eating. This could affect how much and what they eat.
Speech Complications
The facial changes, like a sticking-out upper jaw, can also mess with speech. It can be hard to make some sounds because of the changes in the mouth and teeth. Speech therapy might be needed to help patients speak better.
Dental Health Challenges
Dental health is also a big problem with thalassemia facial features. The sticking-out upper jaw and other changes make it hard to keep teeth clean. This raises the risk of tooth decay and gum disease.
It’s important for these patients to see the dentist often and brush their teeth well.
Respiratory Considerations
In some cases, the facial and skeletal changes can also affect breathing. The bone marrow growth can cause rib and spine problems. This might make it harder to breathe.
It’s key to watch and manage breathing health in these patients. This is part of their overall care.
Psychological and Social Aspects of Facial Deformities
Facial deformities from Beta Thalassemia Major deeply affect a person’s mental health and social life. The changes in face shape bring emotional and social hurdles.
Impact on Body Image and Self-Esteem
Changes in face shape from thalassemia can hurt a person’s body image and self-esteem. They might feel insecure, unworthy, and anxious about how they look.
Effects on Social Interactions and Stigma
Facial deformities from thalassemia can also change how people interact socially. They might face stigma, be left out, or get too much attention. This can make them feel isolated and lower their self-esteem even more.
| Aspect | Potential Impact |
| Body Image | Negative self-perception, insecurity |
| Self-Esteem | Low self-worth, anxiety |
| Social Interactions | Social stigma, exclusion |
Coping Strategies and Support
People with thalassemia-related facial deformities need good ways to cope and support. This includes talking to a psychologist, joining support groups, and learning more about their condition. These steps help manage the emotional and social challenges they face.
Diagnosis and Assessment of Facial Changes
Diagnosing facial changes in Beta Thalassemia Major requires a detailed approach. It uses various clinical and diagnostic methods. These help accurately measure the extent of facial deformities.
Clinical Evaluation Methods
Clinical evaluation is the first step in diagnosing facial changes in Beta Thalassemia Major. A thorough physical exam is done. It looks for signs like prominent cheekbones, depressed nasal bridge, and protruding upper jaw.
Healthcare professionals then assess how severe these features are. They consider how these features affect the patient’s health and quality of life.
Radiological Assessment Techniques
Radiological assessment techniques are key in evaluating bone deformities in Beta Thalassemia Major. X-rays, CT scans, and MRIs are used. They help spot skeletal issues like bone marrow expansion and cortical thinning.
These issues lead to the characteristic facial changes seen in the condition.
Genetic Testing and Confirmation
Genetic testing is vital for confirming Beta Thalassemia Major diagnosis. It helps understand the genetic cause of the condition. Molecular analysis looks for mutations in the HBB gene.
This gene codes for the beta-globin subunit of hemoglobin. Knowing this is important for genetic counseling and family planning.
Differential Diagnosis Considerations
When diagnosing facial changes in Beta Thalassemia Major, it’s important to think about other conditions. Conditions like sickle cell disease and other hemoglobinopathies can look similar. This makes differential diagnosis key for accurate diagnosis and treatment.
Treatment Approaches for Preventing and Managing Facial Deformities
Several key strategies help prevent and manage facial deformities in Beta Thalassemia Major. These treatments can greatly improve life quality for those affected.
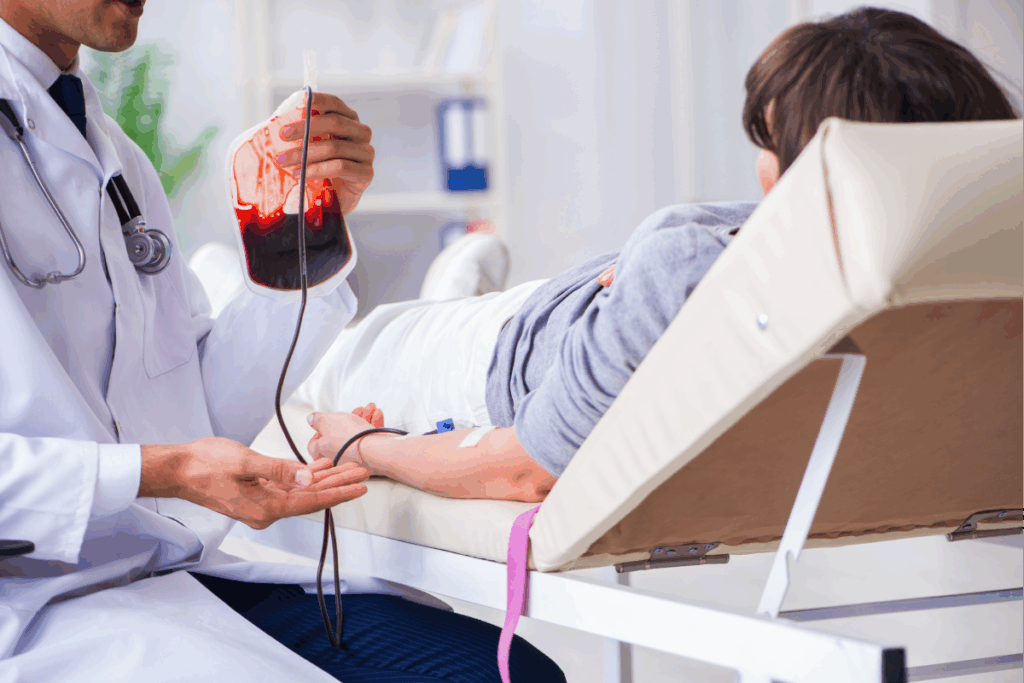
Regular Blood Transfusion Therapy
Regular blood transfusions are key in managing Beta Thalassemia Major. They keep hemoglobin levels up. This reduces bone marrow expansion and facial deformities.
- Reduces anemia and related complications
- Decreases bone marrow expansion
- Improves overall health and well-being
Iron Chelation Management
Iron chelation therapy is vital for managing iron overload from blood transfusions. Excess iron can harm organs. Chelation therapy removes this excess iron.
Benefits of Iron Chelation:
- Reduces iron overload
- Prevents organ damage
- Enhances patient survival and quality of life
Bone Marrow Transplantation
Bone marrow transplantation can cure Beta Thalassemia Major. It replaces the patient’s marrow with healthy marrow from a donor. This addresses the disease’s root cause.
Considerations for Bone Marrow Transplantation:
- Availability of a compatible donor
- Risk of graft-versus-host disease
- Pre-transplant conditioning regimen
Orthodontic and Maxillofacial Interventions
Orthodontic and maxillofacial treatments are needed to fix facial deformities and improve oral function. These include orthodontic treatments and surgical jaw corrections.
Treatment for Beta Thalassemia Major involves medical and surgical steps to prevent and fix facial deformities. Regular check-ups and a team of specialists are key for the best results.
Conclusion
Beta thalassemia major is a genetic disorder that can cause facial deformities. These are known as chipmunk facies or thalassemia chipmunk facies. It’s important to understand the reasons behind these changes to manage them well.
The face of someone with beta thalassemia major often shows signs like big cheekbones and a sunken nose. The upper jaw also sticks out more. These changes can make everyday tasks like eating and speaking harder.
There are many ways to treat and prevent these facial changes. Blood transfusions, iron chelation, and bone marrow transplants are some of them. These treatments help manage the condition.
Healthcare providers can make treatment plans better by knowing the causes of thalassemia chipmunk facies. Early and complete care can greatly improve life for those with beta thalassemia major.
FAQ
What is beta thalassemia major?
Beta thalassemia major, also known as Cooley’s anemia, is a severe form of thalassemia. It affects the production of the beta-globin chains of hemoglobin. This leads to severe anemia and other complications.
What are the characteristic facial features of beta thalassemia major?
The facial features of beta thalassemia major include prominent cheekbones and a depressed nasal bridge. There’s also a protruding upper jaw and frontal bossing. Together, they are known as chipmunk facies.
How do bone marrow hyperactivity and ineffective erythropoiesis contribute to facial changes in beta thalassemia major?
Bone marrow hyperactivity and ineffective erythropoiesis cause bone deformities. This includes facial changes. It happens because the bone marrow expands to compensate for the lack of effective red blood cell production.
What is the role of regular blood transfusions in managing beta thalassemia major?
Regular blood transfusions reduce the severity of anemia. They decrease the need for bone marrow expansion. This helps prevent or reduce bone deformities, including facial changes.
How do thalassemia facial features affect chewing and eating?
Thalassemia facial features, like maxillary hypertrophy and dental malocclusion, make chewing and eating hard. This can affect nutritional intake.
What are the psychological impacts of facial deformities in thalassemia patients?
Facial deformities can harm body image and self-esteem. They can lead to social stigma and make social interactions hard. This shows the need for coping strategies and support.
How are facial changes in thalassemia diagnosed and assessed?
Facial changes in thalassemia are diagnosed and assessed through clinical evaluation and radiological techniques. Genetic testing is also used. Differential diagnoses are considered.
What treatment approaches are available for managing facial deformities in thalassemia?
Treatment approaches include regular blood transfusions and iron chelation management. Bone marrow transplantation and orthodontic and maxillofacial interventions are also used. These help prevent or manage facial deformities.
Can bone marrow transplantation cure beta thalassemia major?
Bone marrow transplantation is the only curative treatment for beta thalassemia major. It offers the chance to eliminate the need for lifelong blood transfusions and other supportive care.
What is the significance of iron chelation therapy in beta thalassemia major management?
Iron chelation therapy is key in managing iron overload from frequent blood transfusions. It helps prevent organ damage and other complications from iron accumulation.
Reference
- National Center for Biotechnology Information (NCBI): Guidelines for the Clinical Management of Thalassaemia
https://www.ncbi.nlm.nih.gov/books/NBK173968/

Beta thalassemia major is a genetic disorder that leads to chronic anemia. This causes the bone marrow to work too hard. As a result, it creates distinct facial features.
One of these features is chipmunk facies. It includes prominent cheekbones, a depressed nasal bridge, and a protruding upper jaw.
These facial changes happen because the bone marrow expands. This is an attempt to make up for the lack of red blood cells. Getting blood transfusions early is key to preventing or lessening these bone deformities.
Key Takeaways
- Beta thalassemia major causes distinct facial abnormalities due to bone marrow overactivity.
- Characteristic features include prominent cheekbones, depressed nasal bridge, and protruding upper jaw.
- Early blood transfusions are key in preventing or reducing bone deformities.
- Liv Hospital’s patient-centered approach transforms outcomes for those living with these conditions.
- Understanding the effects of beta thalassemia major on facial structure is essential for effective management.
Understanding Beta Thalassemia Major

Beta thalassemia major comes from mutations in the HBB gene. This gene is responsible for the beta-globin subunit of hemoglobin. The condition leads to less or no beta-globin chains, causing severe anemia and other issues.
Genetic Basis of Beta Thalassemia
Beta thalassemia major is caused by HBB gene mutations on chromosome 11. These mutations can reduce or eliminate beta-globin chains. The condition’s severity depends on the mutation type and whether an individual has two copies of the mutation.
Pathophysiology and Chronic Anemia
The condition’s pathophysiology involves ineffective erythropoiesis and chronic anemia. Without beta-globin chains, alpha-globin chains build up and harm red blood cells. This causes their early destruction, leading to severe anemia.
Chronic anemia requires regular blood transfusions. It also causes bone deformities and growth issues.
Global Prevalence and Demographics
Beta thalassemia major is common in areas where malaria was once prevalent, like the Mediterranean, Middle East, and South Asia. Migration has spread it to North America and Europe. It has a significant global presence, with high carrier rates in some populations.
| Region | Prevalence | Carrier Frequency |
| Mediterranean | High | 1 in 7 to 1 in 30 |
| Middle East | High | 1 in 5 to 1 in 20 |
| South Asia | High | 1 in 10 to 1 in 30 |
| North America | Low to Moderate | 1 in 20 to 1 in 50 |
| Europe | Low to Moderate | 1 in 30 to 1 in 60 |
The Beta Thalassemia Major Face: Clinical Overview

The beta thalassemia major face shows specific changes due to the disease’s pathophysiology.
Beta thalassemia major, or Cooley’s anemia, is a severe form of thalassemia. It greatly affects the quality of life of those who have it. The disease causes chronic anemia, which means patients need regular blood transfusions.
Definition and Medical Significance
The term “beta thalassemia major face” describes the unique facial features of patients with untreated or poorly treated beta thalassemia major. These features come from bone marrow expansion due to ineffective erythropoiesis.
Chipmunk facies is what these patients’ faces are called. It’s marked by big cheekbones, a sunken nasal bridge, and a sticking-out upper jaw.
When Facial Changes Typically Develop
Facial changes in beta thalassemia major start to show in early childhood. This usually happens between 2 and 6 years old as the disease gets worse and anemia increases.
A clinical expert said, “Early diagnosis and treatment can greatly change the disease’s course. It can also lessen the severity of facial changes.”
“The facial deformities linked to beta thalassemia major are a big worry for patients and their families. They affect not just physical health but also mental well-being.”
Relationship to Disease Severity
The severity of facial changes depends on the disease’s severity and treatment. Patients who get regular blood transfusions and iron chelation therapy are less likely to have severe facial deformities.
A study in a well-known medical journal showed that “effective management of beta thalassemia major can stop or lessen the appearance of typical facial features.”
This shows how important early diagnosis and proper management of beta thalassemia major are.
Pathophysiology Behind Chipmunk Facies
The chipmunk facies comes from a mix of bone marrow activity and poor red blood cell making. In beta thalassemia major, the body can’t make enough hemoglobin. This leads to long-term anemia and the body tries to fix it in many ways.
Bone Marrow Hyperactivity Mechanism
Bone marrow gets busier to make up for the anemia in beta thalassemia major. It tries to make more red blood cells. This makes the bone marrow grow, causing bony changes like chipmunk facies.
The body makes more erythropoietin to help make red blood cells. But in beta thalassemia major, this doesn’t work well because of a genetic problem with hemoglobin.
Ineffective Erythropoiesis
In beta thalassemia major, the bone marrow makes bad or short-lived red blood cells. This makes the body keep making more erythropoietin and the bone marrow gets bigger.
- More erythropoietin makes the bone marrow work harder.
- The bone marrow gets bigger, causing bone changes.
- Bad red blood cells keep the anemia going.
Skeletal Response to Chronic Anemia
The bones try to help by making more red blood cells. This leads to bone deformities. The bone marrow growing in the face bones causes the chipmunk facies.
The face changes include prominent cheekbones and a depressed nasal bridge. These changes happen because the body is trying to fix the blood problem.
In summary, chipmunk facies in beta thalassemia major comes from bone marrow activity, bad red blood cell making, and bone changes due to anemia. Knowing how these work together helps in managing the condition and its effects on the face.
7 Characteristic Features of Thalassemia Chipmunk Facies
The term ‘thalassemia chipmunk facies’ refers to facial changes seen in beta-thalassemia major. These changes come from bone marrow activity and ineffective blood cell production. They lead to noticeable facial structure changes.
Prominent Cheekbones (Malar Prominence)
One key feature is the prominent cheekbones, or malar prominence. This happens because the bone marrow in the face grows, making the cheekbones bigger and stick out more.
Depressed Nasal Bridge
A depressed nasal bridge is another sign. It’s caused by bone marrow growth in the face, pushing the nasal bridge down.
Protruding Upper Jaw (Maxillary Hypertrophy)
Maxillary hypertrophy, or the upper jaw sticking out, is a big feature. It’s due to the maxillary bone growing too much because of bone marrow activity.
Frontal Bossing
Frontal bossing, or a big forehead, is common too. It’s caused by the frontal bone marrow expanding, making the forehead stick out more.
These features show how beta-thalassemia major affects the face. Knowing about them is key for managing and treating this condition.
Additional Bone Deformities in Beta Thalassemia
Beta thalassemia major can cause more than just the chipmunk facies. It affects bone marrow and leads to other bone deformities. This is because the body tries to make up for chronic anemia.
Spinal and Rib Abnormalities
Spinal and rib issues are common in beta thalassemia major. Bone marrow expands to help with anemia, causing:
- Vertebral body collapse
- Rib deformities
- Kyphosis or scoliosis
| Spinal Abnormality | Description | Potential Complications |
| Vertebral Body Collapse | Collapse of the vertebral bodies due to bone marrow expansion | Back pain, spinal instability |
| Rib Deformities | Deformation of the ribs due to marrow expansion | Respiratory issues, pain |
Limb Deformities
Limb issues in beta thalassemia major come from bone marrow growth and thin bones. This can cause:
- Pathological fractures
- Cortical thinning
- Deformities in the long bones
Growth Retardation and Delayed Development
Beta thalassemia major can slow down growth and development in kids. Chronic anemia and bone marrow growth can lead to:
- Delayed puberty
- Short stature
- Growth retardation
Regular treatment and management are key to reduce these effects. They help improve the life quality of those affected.
Functional Impacts of Thalassemia Facial Features
Thalassemia facial features can greatly affect the lives of those with beta thalassemia major. These facial changes can cause many challenges in daily life. They can also impact a person’s overall well-being.
Effects on Chewing and Eating
The facial changes from beta thalassemia major, like a bigger upper jaw, can change how we eat. These changes can make chewing and eating hard. This is because the teeth and jaw might not work right.
Patients might feel pain or discomfort when eating. This could affect how much and what they eat.
Speech Complications
The facial changes, like a sticking-out upper jaw, can also mess with speech. It can be hard to make some sounds because of the changes in the mouth and teeth. Speech therapy might be needed to help patients speak better.
Dental Health Challenges
Dental health is also a big problem with thalassemia facial features. The sticking-out upper jaw and other changes make it hard to keep teeth clean. This raises the risk of tooth decay and gum disease.
It’s important for these patients to see the dentist often and brush their teeth well.
Respiratory Considerations
In some cases, the facial and skeletal changes can also affect breathing. The bone marrow growth can cause rib and spine problems. This might make it harder to breathe.
It’s key to watch and manage breathing health in these patients. This is part of their overall care.
Psychological and Social Aspects of Facial Deformities
Facial deformities from Beta Thalassemia Major deeply affect a person’s mental health and social life. The changes in face shape bring emotional and social hurdles.
Impact on Body Image and Self-Esteem
Changes in face shape from thalassemia can hurt a person’s body image and self-esteem. They might feel insecure, unworthy, and anxious about how they look.
Effects on Social Interactions and Stigma
Facial deformities from thalassemia can also change how people interact socially. They might face stigma, be left out, or get too much attention. This can make them feel isolated and lower their self-esteem even more.
| Aspect | Potential Impact |
| Body Image | Negative self-perception, insecurity |
| Self-Esteem | Low self-worth, anxiety |
| Social Interactions | Social stigma, exclusion |
Coping Strategies and Support
People with thalassemia-related facial deformities need good ways to cope and support. This includes talking to a psychologist, joining support groups, and learning more about their condition. These steps help manage the emotional and social challenges they face.
Diagnosis and Assessment of Facial Changes
Diagnosing facial changes in Beta Thalassemia Major requires a detailed approach. It uses various clinical and diagnostic methods. These help accurately measure the extent of facial deformities.
Clinical Evaluation Methods
Clinical evaluation is the first step in diagnosing facial changes in Beta Thalassemia Major. A thorough physical exam is done. It looks for signs like prominent cheekbones, depressed nasal bridge, and protruding upper jaw.
Healthcare professionals then assess how severe these features are. They consider how these features affect the patient’s health and quality of life.
Radiological Assessment Techniques
Radiological assessment techniques are key in evaluating bone deformities in Beta Thalassemia Major. X-rays, CT scans, and MRIs are used. They help spot skeletal issues like bone marrow expansion and cortical thinning.
These issues lead to the characteristic facial changes seen in the condition.
Genetic Testing and Confirmation
Genetic testing is vital for confirming Beta Thalassemia Major diagnosis. It helps understand the genetic cause of the condition. Molecular analysis looks for mutations in the HBB gene.
This gene codes for the beta-globin subunit of hemoglobin. Knowing this is important for genetic counseling and family planning.
Differential Diagnosis Considerations
When diagnosing facial changes in Beta Thalassemia Major, it’s important to think about other conditions. Conditions like sickle cell disease and other hemoglobinopathies can look similar. This makes differential diagnosis key for accurate diagnosis and treatment.
Treatment Approaches for Preventing and Managing Facial Deformities
Several key strategies help prevent and manage facial deformities in Beta Thalassemia Major. These treatments can greatly improve life quality for those affected.
Regular Blood Transfusion Therapy
Regular blood transfusions are key in managing Beta Thalassemia Major. They keep hemoglobin levels up. This reduces bone marrow expansion and facial deformities.
- Reduces anemia and related complications
- Decreases bone marrow expansion
- Improves overall health and well-being
Iron Chelation Management
Iron chelation therapy is vital for managing iron overload from blood transfusions. Excess iron can harm organs. Chelation therapy removes this excess iron.
Benefits of Iron Chelation:
- Reduces iron overload
- Prevents organ damage
- Enhances patient survival and quality of life
Bone Marrow Transplantation
Bone marrow transplantation can cure Beta Thalassemia Major. It replaces the patient’s marrow with healthy marrow from a donor. This addresses the disease’s root cause.
Considerations for Bone Marrow Transplantation:
- Availability of a compatible donor
- Risk of graft-versus-host disease
- Pre-transplant conditioning regimen
Orthodontic and Maxillofacial Interventions
Orthodontic and maxillofacial treatments are needed to fix facial deformities and improve oral function. These include orthodontic treatments and surgical jaw corrections.
Treatment for Beta Thalassemia Major involves medical and surgical steps to prevent and fix facial deformities. Regular check-ups and a team of specialists are key for the best results.
Conclusion
Beta thalassemia major is a genetic disorder that can cause facial deformities. These are known as chipmunk facies or thalassemia chipmunk facies. It’s important to understand the reasons behind these changes to manage them well.
The face of someone with beta thalassemia major often shows signs like big cheekbones and a sunken nose. The upper jaw also sticks out more. These changes can make everyday tasks like eating and speaking harder.
There are many ways to treat and prevent these facial changes. Blood transfusions, iron chelation, and bone marrow transplants are some of them. These treatments help manage the condition.
Healthcare providers can make treatment plans better by knowing the causes of thalassemia chipmunk facies. Early and complete care can greatly improve life for those with beta thalassemia major.
FAQ
What is beta thalassemia major?
Beta thalassemia major, also known as Cooley’s anemia, is a severe form of thalassemia. It affects the production of the beta-globin chains of hemoglobin. This leads to severe anemia and other complications.
What are the characteristic facial features of beta thalassemia major?
The facial features of beta thalassemia major include prominent cheekbones and a depressed nasal bridge. There’s also a protruding upper jaw and frontal bossing. Together, they are known as chipmunk facies.
How do bone marrow hyperactivity and ineffective erythropoiesis contribute to facial changes in beta thalassemia major?
Bone marrow hyperactivity and ineffective erythropoiesis cause bone deformities. This includes facial changes. It happens because the bone marrow expands to compensate for the lack of effective red blood cell production.
What is the role of regular blood transfusions in managing beta thalassemia major?
Regular blood transfusions reduce the severity of anemia. They decrease the need for bone marrow expansion. This helps prevent or reduce bone deformities, including facial changes.
How do thalassemia facial features affect chewing and eating?
Thalassemia facial features, like maxillary hypertrophy and dental malocclusion, make chewing and eating hard. This can affect nutritional intake.
What are the psychological impacts of facial deformities in thalassemia patients?
Facial deformities can harm body image and self-esteem. They can lead to social stigma and make social interactions hard. This shows the need for coping strategies and support.
How are facial changes in thalassemia diagnosed and assessed?
Facial changes in thalassemia are diagnosed and assessed through clinical evaluation and radiological techniques. Genetic testing is also used. Differential diagnoses are considered.
What treatment approaches are available for managing facial deformities in thalassemia?
Treatment approaches include regular blood transfusions and iron chelation management. Bone marrow transplantation and orthodontic and maxillofacial interventions are also used. These help prevent or manage facial deformities.
Can bone marrow transplantation cure beta thalassemia major?
Bone marrow transplantation is the only curative treatment for beta thalassemia major. It offers the chance to eliminate the need for lifelong blood transfusions and other supportive care.
What is the significance of iron chelation therapy in beta thalassemia major management?
Iron chelation therapy is key in managing iron overload from frequent blood transfusions. It helps prevent organ damage and other complications from iron accumulation.
Reference
- National Center for Biotechnology Information (NCBI): Guidelines for the Clinical Management of Thalassaemia
https://www.ncbi.nlm.nih.gov/books/NBK173968/








