Embryonic stem cells are a key part of regenerative medicine. They could change how we treat many diseases.
These cells come from the early stages of a developing embryo. They can turn into many different cell types. This makes them very useful for medical research.
Studies on embryonic stem cells are showing great promise. They could help in creating new tissues and treatments.
ES cells have changed the world of stem cell biology. They can keep growing and change into different types of cells. This makes them key in studying how we grow and develop. They also hold great promise for helping people with diseases.
Embryonic stem cells are pluripotent cells from the inner cell mass of a blastocyst, an early embryo. They can turn into any cell in the body. This makes them very useful for research and could help in treating diseases.
Here are the main traits of ES cells:
The discovery of ES cells started in the 1980s with mouse embryos. Then, in 1998, scientists got human ES cells. This was a big step forward in stem cell research.
The discovery of ES cells is linked to big steps in genetic engineering and cell differentiation. These steps helped scientists understand how ES cells work.
ES cells are very important in science. They help us understand how we grow and develop. They also help in studying diseases and finding new treatments.
Here are some key areas where ES cells help a lot:
Embryonic stem cells are mainly divided into three types: totipotent, pluripotent, and multipotent. Each type has its own special abilities and uses. Knowing about these differences is key for improving regenerative medicine and finding new treatments.
Totipotent embryonic stem cells can turn into every cell type in the body. This includes cells in the embryo, the placenta, and other tissues. Their ability to do this is very important in the early stages of growth.
Pluripotent embryonic stem cells can become most cell types in the body. They can’t turn into cells of the placenta or other supporting tissues. Their wide range of uses makes them very valuable for studying how to repair and grow tissues.
Multipotent embryonic stem cells can only turn into cells within a specific lineage. For example, they can become blood cells or nerve cells. Even though they have a narrower range of abilities, they are also promising for medical treatments.
The differences between these three types of embryonic stem cells are not just for learning. They are also important for stem cell research and medical uses. By understanding what each type can do, scientists can find new ways to use them in medicine and engineering tissues.
Totipotent embryonic stem cells are at the start of cell development. They are key to understanding how an organism begins. These cells form early in embryonic development and can grow into a complete organism.
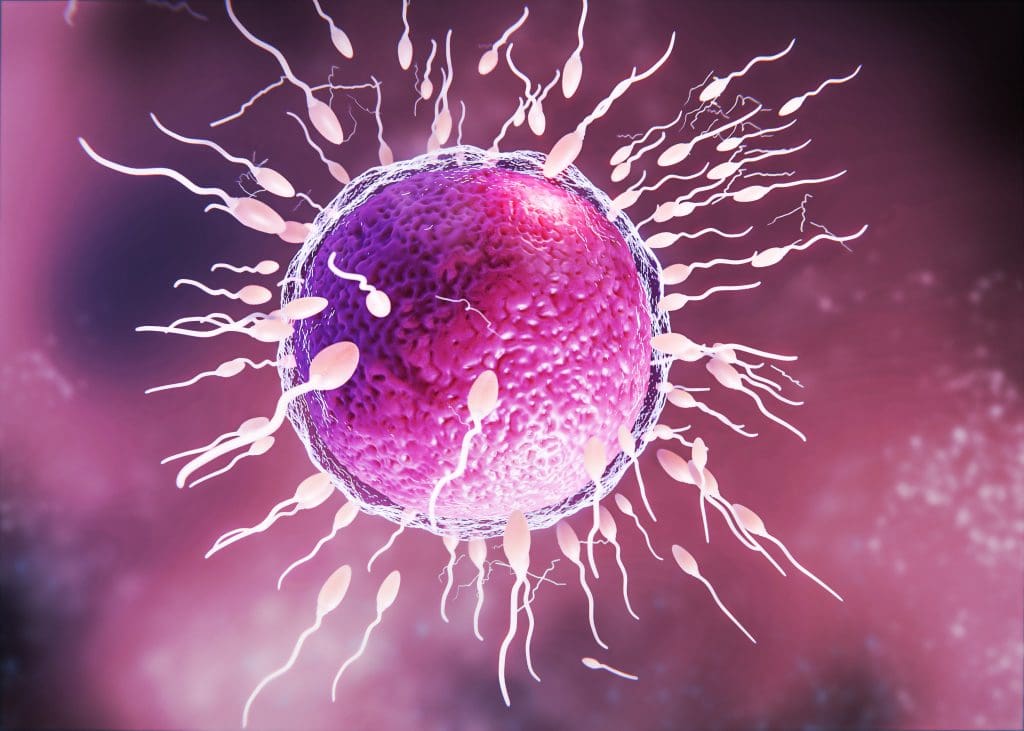
These cells form right after fertilization, when the zygote starts dividing. At this time, they are totipotent. This means they can turn into any cell type in the organism, including the embryo and supporting tissues.
Totipotent cells have special traits that set them apart. Their ability to become any cell type is very useful for studying early development. Some of their main abilities include:
Research on totipotent embryonic stem cells is important for many fields. This includes developmental biology, genetics, and regenerative medicine. Some main research areas include:
By studying totipotent embryonic stem cells, scientists can learn about the basic processes of organism development. This could lead to new medical treatments and a better understanding of human biology.
Embryonic stem cells, known as pluripotent, can turn into almost any cell in our bodies. This makes them very useful for medical studies and possible treatments.
These cells come from the inner part of an early embryo called a blastocyst. They can keep growing and change into different cell types. This process is controlled by special genes and signals.
Key characteristics of pluripotent embryonic stem cells include:
These cells can become many types of cells, which is great for research. They can turn into neurons, muscle cells, or even cells in the pancreas, with the right conditions.
“The ability to generate cells that can replace damaged or diseased cells in the body opens new avenues for treating a wide range of medical conditions.”
| Cell Type | Potential Applications |
| Neurons | Treatment of neurodegenerative diseases, such as Parkinson’s disease |
| Cardiomyocytes | Repair of damaged heart tissue |
| Pancreatic Islet Cells | Treatment of diabetes |
Scientists are studying these cells to learn more about them. They’re working on better ways to get and grow these cells. They also look into using adult cells that can become like these stem cells, as an alternative.
As research goes on, these cells might help in treating many diseases. This is very exciting for regenerative medicine and studying diseases.
Learning about multipotent embryonic stem cells is key for improving tissue repair and regeneration research. These cells can turn into many cell types but only within certain groups or tissues.
Multipotent embryonic stem cells start from early embryonic stages. They can only become certain cell types within a specific germ layer. This both limits and helps their use in medicine.
The growth of these stem cells is controlled by genes and the environment. Knowing how they grow is vital for using them in medical treatments.
Multipotent embryonic stem cells are great because they can become specific tissue cells. For example, mesenchymal stem cells can become bone, cartilage, and fat cells. This makes them useful for fixing bone, cartilage, and fat tissue problems.
Scientists are looking into how these cells can help with many health issues. This includes muscle and bone problems and diseases that get worse over time.
The healing power of multipotent embryonic stem cells is huge. They can fix or replace damaged tissues. Scientists are working on using them in treatments for degenerative diseases.
Studying these stem cells also helps us understand how bodies grow and repair. This could lead to big advances in regenerative medicine.
As we learn more about multipotent embryonic stem cells, their importance in medicine grows. They could help a lot in stem cell therapy and tissue engineering. This opens up new ways to treat many diseases.
Understanding ES cells is key for their use in research and medicine. These cells can grow and change into many types. This makes them very useful.
ES cells have a special cell structure. This structure helps them grow into different cell types. The cell membrane, cytoplasm, and nucleus work together to keep the cell’s ability to change.
The nucleus of an ES cell has a big nucleolus. This shows the cell is very active in making new proteins. This activity is important for the cell’s growth and change.
ES cells have special genes that help them stay in a state of change. Genes like Oct4, Sox2, and Nanog are key. They control the genes needed for change.
“The expression of these transcription factors is critical for ES cells to stay in a state of change. This lets them become any cell type in the body.”
A study looked at the genes in ES cells and changed cells. It found big differences in important genes.
| Gene | ES Cells | Differentiated Cells |
| Oct4 | Highly Expressed | Not Expressed |
| Sox2 | Highly Expressed | Lowly Expressed |
| Nanog | Highly Expressed | Not Expressed |
ES cells divide quickly. This is important for their growth. The cell cycle in ES cells is fast, with a short G1 phase and a quick S phase for DNA replication.
The quick division of ES cells is vital for research and medicine. Knowing how they divide helps us use them better.
Embryonic stem cell cultivation is key to keeping ES cells in a pluripotent state. It involves several important steps. These range from the initial cell isolation to keeping them undifferentiated over time.
The first step in getting embryonic stem cells is to dissociate embryonic cells from the inner cell mass of a blastocyst. This step needs meticulous care to prevent contamination and keep the cells alive. Methods like immunosurgery or mechanical dissection are often used.
“The derivation of embryonic stem cells is a delicate process that requires precision and patience.”
After isolating ES cells, they must be grown in specific conditions to keep them pluripotent. This includes using feeder layers or feeder-free systems and defined culture media with growth factors like bFGF. Keeping the culture conditions just right is essential for growing ES cells long-term.
Keeping ES cells in a stem state for a long time is a big challenge. Issues like genetic drift and epigenetic changes can happen, affecting their pluripotency. Researchers must use rigorous quality control measures to check the cells’ status. This ensures they are good for research or therapy.
By improving how we grow embryonic stem cells, researchers can use ES cells better. This is for things like regenerative medicine and finding new drugs.
It’s important to know the difference between embryonic stem cells and adult stem cells for regenerative medicine. Both are studied for their role in cell therapy. Yet, they have unique traits.
Embryonic stem cells can turn into any cell type in the body. In contrast, adult stem cells can only turn into specific cell types from their original tissue.
| Characteristics | Embryonic Stem Cells | Adult Stem Cells |
| Differentiation Ability | Broad (pluripotent) | Limited (multipotent or unipotent) |
| Availability | Limited, often from embryos | More available from adult tissues |
| Ethical Concerns | High due to embryo use | Less due to adult tissue origin |
Embryonic stem cells can become any cell type, making them valuable for research and therapy. But, their use is limited by ethics and the risk of uncontrolled growth. Adult stem cells are easier to get and have fewer ethical issues. Yet, they can only turn into specific cell types.
Both embryonic stem cells and adult stem cells are key to regenerative medicine and cell therapy. Research on both types helps each other, bringing unique insights and uses. By using both, scientists can move forward in regenerative medicine.
In summary, embryonic stem cells and adult stem cells have different properties and uses. Embryonic stem cells have wide differentiation ability, while adult stem cells are more available and ethically simpler. Both are vital for regenerative medicine and cell therapy.
ES cells are leading the way in medical innovation. They can turn into different cell types. This makes them key for fixing damaged tissues and studying diseases.
Regenerative medicine has made big strides with ES cells. These cells can become specific types of cells. This could help treat heart disease, Parkinson’s, and spinal cord injuries.
Key Applications:
“Using ES cells in regenerative medicine is a game-changer. It gives us hope for treating diseases we thought were untreatable.”
– A Stem Cell Researcher
ES cells are also key for studying diseases and testing drugs. By turning into specific cell types, researchers can study diseases in the lab. They can see how diseases progress and test new drugs.
| Disease | Cell Type | Research Application |
| Parkinson’s Disease | Dopaminergic Neurons | Modeling disease progression, drug testing |
| Heart Disease | Cardiomyocytes | Regenerative therapies, drug development |
ES cells are used in personalized medicine to create patient-specific cells. This can lead to treatments that are more tailored and have fewer side effects.
As research keeps moving forward, ES cells will likely play an even bigger role in medicine. This could bring new hope for treating many diseases.
The ethics of using embryonic stem cells for research are complex. This is because many people have different views on the topic. These views come from various moral, religious, and legal standpoints.
People from different cultures and religions have different opinions on using embryos for research. Some think embryos could become human beings and should not be used for research. Others believe the benefits of such research outweigh the ethical concerns.
“The question of whether human embryonic stem cell research is morally justifiable is a matter of ongoing debate, reflecting diverse ethical and religious perspectives.”
” Expert in Bioethics
How countries regulate embryonic stem cell research varies a lot. Some have strict rules or bans, while others are more open to it.
One big challenge in this research is finding a balance between scientific progress and ethics. Researchers, policymakers, and ethicists need to work together to solve these complex issues.
Key considerations include:
By tackling these ethical issues, scientists can move forward with research. They can do this while respecting different moral and legal views.
Embryonic stem cell research is growing fast. New discoveries are happening all the time. Many research centers worldwide are working together to learn more about ES cells.
Some places are leading the way in ES cell research. The Harvard Stem Cell Institute and the Stanford University School of Medicine are at the top. They study ES cells in many ways, from basic science to using them in medicine.
Recently, ES cell research has made big strides. Scientists have found better ways to turn ES cells into different types of cells. This is good for fixing damaged tissues. Also, new gene editing tools let researchers make precise changes to ES cells. This opens up new paths for research and treatments.
Funding and policies for ES cell research in the U.S. change often. Sometimes, there’s a lot of support, and other times, there’s not enough. Now, there’s a mix of government and private money for ES cell research. Some states are more supportive than others. The National Institutes of Health (NIH) gives grants to projects that meet certain standards.
To really understand ES cell research today, you need to know about these funding and policy issues. They affect how fast and in what direction research moves.
New advancements in stem cell technology have brought alternatives to ES cells. These options help solve ethical and scientific issues with embryonic stem cell research.
Induced pluripotent stem cells (iPSCs) are a big step forward in stem cell science. They turn adult cells into a state where they can become many different cell types. This method avoids using embryos, which helps with ethical concerns.
iPSCs are great for personalized medicine. They can be made from a patient’s own cells, lowering the chance of immune reactions. They also work well for studying diseases and testing drugs.
Adult stem cells are found in adult bodies and have been used for treatments for years. New techniques have made it easier to get, grow, and change these cells. Adult stem cells can become a few different cell types, but not as many as ES cells or iPSCs.
Adult stem cells are key for regenerative medicine. They help fix and grow tissues. For example, stem cells from bone marrow or fat have been tested in clinical trials for heart and bone problems.
Creating synthetic and engineered stem cells is a new area in stem cell research. These cells are made to act like natural stem cells or have special traits. Synthetic biology lets scientists make cells for specific uses.
These new options to ES cells help with regenerative medicine. They also solve some of the problems with using embryonic stem cells. As research keeps improving, using these alternatives in treatments is expected to grow. This brings hope for treating many diseases and conditions.
The future of embryonic stem cells looks promising. New methods and technologies are coming. These advancements could lead to exciting uses in medicine.
Gene editing tools like CRISPR/Cas9 are changing the game. They let scientists make precise changes to genes. This could fix genetic problems and create special ES cell lines.
New ways to turn ES cells into specific types are being explored. This is key for using them in treatments. Researchers are looking at small molecules and biomaterials to help.
ES cell research is on the verge of big advances. These could help fix or replace damaged tissues and organs. This offers hope for treating many diseases and injuries.
One exciting area is personalized medicine. By making ES cell lines from a patient’s cells, treatments can be made just for them. This could lower the chance of rejection.
Despite the promise, there are big challenges ahead. The ethics of using ES cells is a major issue. It affects funding and public opinion.
There are also technical hurdles. Making sure ES cell therapies are safe and work well is critical. This requires a lot of testing and validation.
In summary, while there are obstacles, the future of ES cell research is promising. New technologies and methods are set to lead to major breakthroughs in regenerative medicine.
Embryonic stem cells (ES cells) have changed the game in regenerative medicine and stem cell research. There are three types: totipotent, pluripotent, and multipotent. Each type has special abilities that make them useful for different things.
Studying ES cells has brought us big wins in understanding human growth and disease. They can turn into many different cell types. This makes them super important for finding new ways to heal and treat diseases.
As we keep moving forward, ES cells could become even more useful for helping people. But we need to think about the ethics and how to keep them healthy. New technologies and ideas are coming that could help a lot.
In short, ES cells are key to understanding our bodies and finding new treatments. We need to keep supporting research to make the most of ES cells in healing and medicine.
Embryonic stem cells (ES cells) come from early embryos. They can turn into different cell types. This makes them useful for research and possible treatments.
There are three types: totipotent, pluripotent, and multipotent. Each type can do different things in research and medicine.
Totipotent cells can become any cell in the body, including placental cells. Pluripotent cells can become almost any cell, but not placental cells. Multipotent cells can only become specific cell types.
They could help in regenerative medicine, disease modeling, and personalized medicine. This could lead to new ways to treat diseases and injuries.
Using these cells raises ethical questions because they come from embryos. These questions vary by culture and law.
They are grown using special lab techniques. This includes taking them from embryos and keeping them in the right conditions.
They can become more types of cells than adult stem cells. This makes them more useful for research and treatments.
iPSCs are made from adult cells that are changed to be like ES cells. They offer a choice to ES cells, possibly avoiding some ethical issues
Yes, there are alternatives like iPSCs, adult stem cells, and synthetic stem cells. Each has its own benefits and uses.
They are a great model for studying early development and disease. This helps researchers understand how cells develop and model diseases in the lab.
Keeping ES cells in a stem-like state is hard. It requires the right culture conditions, including specific growth factors and careful handling.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!