Learning how to get ready for frozen embryo transfer (FET) is key to a successful pregnancy. FET is a big part of fertility treatments. It has live birth rates of 37% to 59%, based on how well the uterus is prepared and other factors. Explaining the role of birth control before frozen embryo transfer in protocol synchronization.
We’ll walk you through FET preparation. We’ll talk about why the FET protocol matters and how it affects success. Knowing the FET protocol helps people on their fertility journey.
Key Takeaways
- FET is a key part of fertility treatments.
- Success rates change based on uterus preparation and other factors.
- Understanding the FET protocol is important for success.
- Good preparation is essential for a good chance of pregnancy.
- FET is flexible and has high success rates for many.
Understanding Frozen Embryo Transfer (FET)

Frozen Embryo Transfer (FET) is a hope for many facing infertility. It’s a key part of assisted reproductive technology (ART). FET has changed how we tackle fertility issues.
What Is a Frozen Embryo Transfer?
A Frozen Embryo Transfer involves thawing and placing frozen embryos in a woman’s uterus. It’s a part of in vitro fertilization (IVF). This method lets embryos be saved for later use.
First, eggs are taken during an IVF cycle. Then, they’re fertilized with sperm to make embryos. Instead of using them right away, they’re frozen. FET helps time the transfer for better chances of pregnancy.
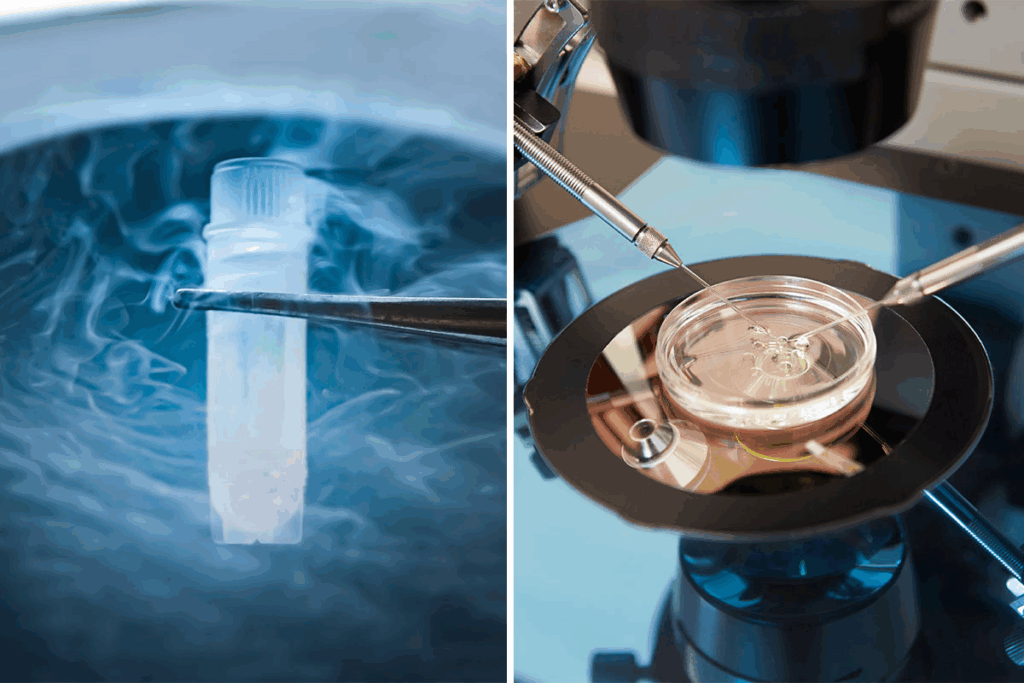
The Embryo Freezing and Thawing Process
Embryo freezing, or cryopreservation, cools embryos to stop all activity. This is done with vitrification to keep the embryos safe. It prevents ice crystals from damaging them.
Thawing is the opposite, warming the embryos for transfer. It’s a delicate process to keep them alive and ready for transfer.
Success Rates of FET
FET success rates have gone up thanks to better freezing and choosing the right embryos. Studies show success rates from 37% to 59%. This depends on the woman’s age, embryo quality, and how the uterus is prepared.
- Key Factors Influencing FET Success Rates:
- Age of the woman
- Quality of the embryos
- Endometrial preparation method
- Embryo freezing and thawing techniques
Large studies show different ways to prepare the uterus work just as well. This means FET can be tailored to fit each person’s needs. It helps increase success rates.
For those facing infertility, FET is a glimmer of hope. Knowing about FET’s process and success rates helps patients choose the right fertility treatment.
Benefits of Choosing FET Over Fresh Transfer
Frozen Embryo Transfer (FET) is becoming more popular. It offers better results and fewer risks than fresh transfers. This makes FET a top choice for many IVF patients.
Reduced Risk of Ovarian Hyperstimulation Syndrome
One big benefit of FET is less risk of Ovarian Hyperstimulation Syndrome (OHSS). OHSS is a serious issue linked to fresh IVF cycles. Freezing embryos and then transferring them later lowers this risk. This makes the treatment safer for our patients.
Improved Endometrial Receptivity
FET helps match the embryo with the uterine lining better. This is key for successful implantation. It can lead to higher success rates in FET cycles than in fresh transfers.
Opportunity for Genetic Testing
Frozen embryo transfers let us test embryos before transfer. This genetic testing of embryos can spot genetic issues. It boosts the chance of a healthy pregnancy and lowers the risk of miscarriage or genetic problems.
Flexibility in Timing Your Transfer
FET cycles offer more flexibility in planning the transfer. This lets patients and doctors pick the best time for the procedure. This is great for those needing more time or adjusting their treatment plans.
In summary, the benefits of choosing FET over fresh transfer are many. They include fewer risks and better results. As IVF technology advances, FET is proving to be a reliable and effective way for people to start families.
Types of FET Protocols and Their Effectiveness
FET protocols are made for each person’s needs and health history. The right protocol can greatly affect the success of the Frozen Embryo Transfer cycle.
An FET cycle usually needs 3-4 visits to the doctor. The timing is key to get the body ready for the embryo transfer. The choice depends on the patient’s health and the clinic’s rules.
Natural Cycle FET
Natural Cycle FET is best for women with regular periods. It doesn’t need a lot of hormone medicine. Instead, it uses the body’s natural cycle to get the uterus ready.
Advantages: Less medicine, lower risk of OHSS, and fewer side effects.
Medicated/Artificial Cycle FET
Medicated or Artificial Cycle FET uses estrogen and progesterone to get the uterine lining ready. It’s good for women with irregular cycles or using donor eggs.
Key benefits: Better timing and uterine lining preparation, which can help with implantation.
Modified Natural Cycle with Trigger
This mix of natural and medicated cycles monitors the natural cycle and uses a trigger shot for timing. It’s a balance between natural and medicated cycles.
Benefits: Combines the best of both worlds.
GnRH Agonist Downregulation Protocol
The GnRH Agonist Downregulation Protocol uses a GnRH agonist to stop the pituitary gland before starting hormones. It’s not as common for FET but works for some.
Considerations: Needs careful management to avoid too much suppression and side effects.
Knowing about the different FET protocols is key for a good IVF journey. Choosing the right one can help increase the chances of a successful Frozen Embryo Transfer.
Birth Control Before Frozen Embryo Transfer: Purpose and Timeline
Using birth control before FET is a common practice. It helps match the menstrual cycle with the transfer date. This makes it easier to prepare the uterus for the embryo.
Why Birth Control Is Used in FET Preparation
Birth control is used to regulate the menstrual cycle. This makes scheduling the transfer easier. It also suppresses ovarian activity, which can increase the chances of a successful transfer.
- Regulates menstrual cycle for better scheduling
- Suppresses ovarian activity to improve transfer success
- Prepares the uterus for the embryo
Optimal Timing for Birth Control Before Starting FET
The timing of birth control before FET is key. It starts at the beginning of the menstrual cycle. A baseline visit is then scheduled about 4 days after stopping birth control pills or on day 2-3 of the cycle.
“The strategic use of birth control before FET can significantly impact the success of the transfer by ensuring the uterus is optimally prepared.”
A fertility specialist
Types of Birth Control Medications Used
Several types of birth control medications are used before FET. These include oral contraceptive pills (OCPs) and other hormonal contraceptives. The choice depends on the individual’s health and fertility needs.
Type of Birth Control | Purpose in FET |
Oral Contraceptive Pills (OCPs) | Regulate menstrual cycle |
Hormonal Contraceptives | Suppress ovarian activity |
Transitioning from Birth Control to FET Medications
Switching from birth control to FET medications is a carefully managed process. It involves stopping birth control and starting FET medications at the right time. This ensures the uterus is ready for the embryo.
Understanding the role of birth control in FET preparation is key. It’s a critical step for a successful Frozen Embryo Transfer.
Complete FET Medication Protocol Guide
The FET medication protocol is key for a successful embryo transfer. It helps increase the chances of getting pregnant. This guide will explain the medications, how they are given, and why they are used.
Estrogen Supplementation Methods and Dosing
Estrogen is used to make the uterine lining thick enough for implantation. It mimics the natural menstrual cycle. This makes the endometrium ready for the embryo.
There are different ways to give estrogen, like tablets, patches, and injections. The method and dose depend on the patient’s needs and medical history.
Common estrogen supplementation protocols include:
- Oral estradiol valerate tablets, starting at 2mg daily and increasing to 6-8mg daily
- Transdermal estradiol patches, changed every 3-4 days
- Intramuscular estradiol injections, given every few days
Progesterone Options and Administration
Progesterone is also vital in the FET protocol. It supports implantation and early pregnancy. We offer different ways to give progesterone based on individual needs.
Progesterone can be given through:
- Vaginal suppositories or gels, which are often preferred for direct delivery to the uterus
- Intramuscular injections, used in some cases
- Oral progesterone, though less common due to variable absorption
The timing and dose of progesterone are carefully planned with the embryo transfer. It usually starts a few days before.
Letrozole-Based Protocols for Reduced Side Effects
Letrozole-based protocols can help reduce side effects from high estrogen levels. Letrozole is an aromatase inhibitor. It helps stimulate ovulation and prepare the uterus for FET.
“The use of letrozole in FET protocols has gained popularity due to its ability to minimize estrogen-related side effects while maintaining a receptive endometrium,” says Medical Expert, a fertility specialist.
Additional Medications and Supplements
Depending on individual needs, additional medications or supplements may be recommended. These can include:
- Low-dose aspirin to improve blood flow to the uterus
- Sildenafil (Viagra) to enhance endometrial thickness
- Antibiotics or other medications to address specific health concerns
It’s important to follow the medication protocol closely. Report any side effects or concerns to your healthcare provider.
Understanding and following the FET medication protocol can increase chances of a successful pregnancy. Our fertility specialists tailor the protocol to each patient’s unique needs. This ensures the best possible outcome.
Step-by-Step FET Preparation Timeline
Knowing the FET preparation timeline is key for success. The FET process includes steps like initial consultation, baseline appointment, and endometrial preparation. These steps are planned carefully for the best results.
Initial Consultation and Testing (1-2 Months Before)
The FET journey starts with an initial consultation. Your fertility specialist will look at your medical history and previous IVF cycles. They will also consider any health conditions you have. This meeting is vital for a personalized treatment plan.
- Review of medical history and previous IVF cycles
- Discussion of treatment options and expectations
- Initial testing, including blood work and ultrasound
Baseline Appointment and Monitoring
After the initial consultation, a baseline appointment is set. It checks your hormonal status and uterine condition. This includes:
- Blood tests to check hormone levels
- Ultrasound to evaluate the uterus and ovaries
This helps your doctor find the best start date for your FET cycle.
Endometrial Preparation Phase (2-3 Weeks)
The endometrial preparation phase focuses on getting your uterus ready for the embryo. This involves:
- Estrogen supplementation to thicken the endometrial lining
- Monitoring through ultrasounds and blood tests
- Progesterone administration to support implantation
Final Preparation Before Transfer Day
In the final stages before the FET, your healthcare team will:
- Confirm the embryo is ready for transfer
- Schedule the transfer procedure
- Provide instructions on medication and post-transfer care
By following this step-by-step FET preparation timeline, patients can ensure they are well-prepared for a successful Frozen Embryo Transfer.
The Frozen Embryo Transfer Procedure Explained
Learning about the FET procedure can ease worries and get patients ready for this key step in their fertility journey. The FET procedure is a key part of assisted reproduction. It offers a good option for those wanting to start or grow their families.
Pre-Transfer Instructions and Preparation
Before the FET, patients get detailed instructions to get ready. They learn about medication, lifestyle changes, and any tests or paperwork needed.
The Embryo Thawing Process
Thawing embryos is a careful step that needs precision. Our skilled embryologists thaw the frozen embryos. They check if they are healthy before moving to the transfer.
The Transfer Procedure Step-by-Step
The FET procedure is quick, lasting about 10 to 15 minutes. Here’s how it goes:
- Preparation for Transfer: The patient gets ready on the procedure table.
- Guidance with Ultrasound: Ultrasound guides the transfer to place the embryo right.
- Embryo Transfer: The embryo is carefully put into the uterus with a catheter.
- Confirmation of Transfer: The ultrasound confirms the embryo’s placement.
Immediate Post-Transfer Care
After the FET, patients get care tips to help the process succeed. They learn about rest, medication, and when to come back for check-ups.
Post-FET Care and Medication Support
The time after FET is very important. Knowing how to care for yourself is key. We’ll talk about post-FET care, including medication, activity, and managing side effects.
Progesterone Support Through 12 Weeks of Pregnancy
Supporting the embryo with progesterone is vital. We give progesterone through 12 weeks to help the pregnancy. This hormone support is usually stopped by the end of the first trimester.
The type and amount of progesterone depend on each patient. It can be given through injections, suppositories, or capsules.
Activity Guidelines After Transfer
After FET, we suggest some activity guidelines. While you don’t need to stay in bed, avoid hard activities.
Here are some tips:
- Avoid heavy lifting and bending
- Don’t do high-impact exercises
- Take gentle walks to keep blood flowing
When to Take a Pregnancy Test
Timing is everything when taking a pregnancy test after FET. We tell patients to wait about two weeks before a blood test.
Home pregnancy tests are not reliable at this time. We do a blood test at our clinic to confirm pregnancy.
Managing Side Effects of FET Medications
FET medications are usually safe, but side effects can happen. Common ones include:
- Bloating and water retention
- Mood swings
- Breast tenderness
To handle these, we suggest:
- Drink plenty of water
- Eat a balanced diet
- Do gentle exercises
If side effects are bad or last too long, we change the medication. This helps keep you comfortable while supporting the pregnancy.
Troubleshooting Common FET Challenges
Dealing with FET can be tough, but knowing the common problems helps. FET is a top treatment, but some face specific hurdles. These need careful handling.
Thin Endometrial Lining
A thin endometrial lining is a big issue in FET. The lining must be thick enough for implantation to work. We use estrogen supplementation and endometrial scratching to help.
Method | Description | Benefits |
Estrogen Supplementation | Administering estrogen to promote endometrial growth | Enhances endometrial receptivity |
Endometrial Scratching | A minor procedure to stimulate endometrial regeneration | May improve implantation rates |
Failed Implantation After Transfer
Failed implantation is tough after FET. It can be due to embryo quality, endometrial receptivity, or synchronization. We look into these closely to find the best solution.
Medication Side Effects Management
FET meds can cause side effects, from mild to severe. Common ones are bloating, mood swings, and fatigue. We help manage these to keep you comfortable.
- Adjusting medication dosages
- Implementing lifestyle changes
- Offering supportive care
When to Consider Protocol Adjustments
Changing the FET protocol might be needed. We watch how you respond and adjust as necessary. This helps get the best results.
Understanding and tackling FET challenges is key to success. Our team is here to offer personalized care and support. We’re with you every step of the way.
Conclusion: Navigating Your FET Journey with Confidence
Understanding the FET process is key to success. Knowing the steps and care after transfer can boost your chances. This knowledge helps you prepare for what’s ahead.
Stay informed and work with your healthcare provider during your FET journey. The FET protocol aims to increase success rates. Knowing about different protocols helps you make better choices.
Frozen embryo transfer success rates are promising, ranging from 37-59%. Following the FET protocol and guidelines can help you achieve a successful transfer and a healthy pregnancy.
Remember, being informed and prepared is vital during your FET journey. Knowing what to expect helps you approach it with confidence and hope.
FAQ
What is a Frozen Embryo Transfer (FET) protocol?
A Frozen Embryo Transfer (FET) protocol is a set of steps to get a woman’s uterus ready for a frozen embryo. It’s designed to increase the chances of a successful pregnancy.
What are the different types of FET protocols?
There are several FET protocols, like Natural Cycle FET and Medicated/Artificial Cycle FET. The choice depends on the patient’s history and the clinic’s approach.
Why is birth control used before FET?
Birth control before FET helps sync the menstrual cycle and prepare the uterus. It improves the timing and chances of a successful pregnancy.
What medications are used in FET?
FET uses estrogen and progesterone. Estrogen thickens the uterine lining, and progesterone supports embryo implantation.
How is the FET procedure performed?
The FET procedure involves thawing and transferring the embryo into the uterus. It’s done under ultrasound to place the embryo correctly.
What is the success rate of FET?
FET success rates vary. They depend on embryo quality, the woman’s age, and the protocol used. Rates range from 37% to 59%.
How long does it take to prepare for FET?
Preparing for FET takes about 2-3 weeks. This includes estrogen supplementation and ultrasound monitoring.
What are the benefits of choosing FET over fresh embryo transfer?
FET has benefits like lower risks of ovarian hyperstimulation syndrome and better endometrial receptivity. It also allows for genetic testing on embryos.
What is the role of progesterone support after FET?
Progesterone support after FET is key for embryo implantation and pregnancy maintenance. It’s continued until about 12 weeks of pregnancy.
How can I manage side effects of FET medications?
Managing FET medication side effects involves adjusting dosage or medication type. Always follow the clinic’s guidelines and report any side effects.
What are the common challenges encountered during FET?
FET challenges include thin endometrial lining, failed implantation, and medication side effects. These can be addressed by adjusting the protocol or seeking support.
References
- Eleftheriadou, A., et al. (2022). Frozen Blastocyst Embryo Transfer: Comparison of Different Endometrial Preparation Protocols and Factors Affecting Outcomes. Fertility and Sterility, 5037 women study. https://pmc.ncbi.nlm.nih.gov/articles/PMC8836366/