Last Updated on November 25, 2025 by Ugurkan Demir
Knowing bladder cancer survival rates by stage is key for patients and their families. It helps them make smart treatment choices. Get the latest bladder cancer survival statistics by stage. Understand the data on prognosis and survival rates for bladder cancer patients.
The overall 5-year survival rate for bladder cancer is about 78%, says the American Cancer Society.
Survival rates change a lot based on the stage at diagnosis. They are high for early-stage disease but lower for advanced cases.
We will look at how survival rates change by stage, from non-muscle-invasive to advanced bladder cancer. We will also talk about what affects these rates.

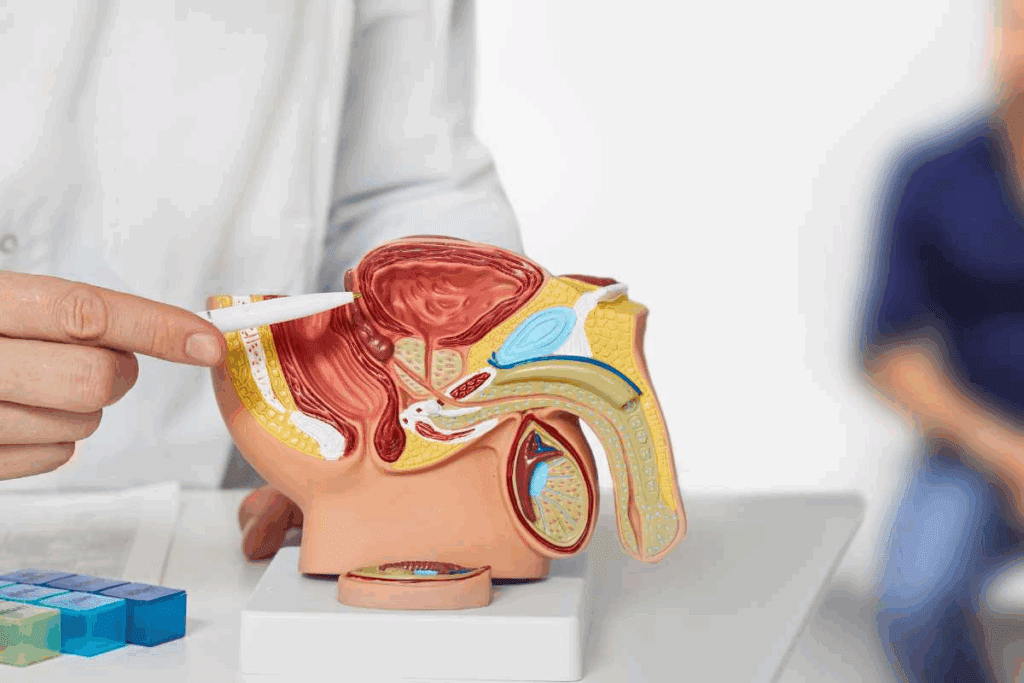
To tackle bladder cancer effectively, it’s vital to grasp its underlying nature and manifestations. Bladder cancer originates in the bladder’s lining. Understanding its basics is key for early detection and effective treatment.
Bladder cancer is a type of cancer that begins in the bladder. The bladder is a hollow organ in the pelvis that stores urine. Most bladder cancers start in the urothelial cells that line the inside of the bladder.
Urothelial carcinoma, also known as transitional cell carcinoma, is the most common type. It accounts for about 90% of all bladder cancer cases.
While urothelial carcinoma is the most prevalent form, other types of bladder cancer include:
Understanding these different types is essential for determining the best treatment approach.
Several factors increase the risk of developing bladder cancer, including:
Common symptoms include:
Recognizing these risk factors and symptoms can lead to earlier diagnosis and more effective treatment strategies.

Getting the right stage for bladder cancer is key to finding the best treatment. We use a set system to figure out how far the cancer has spread. This helps predict how well a patient will do and what treatment to use.
The TNM system is used a lot for bladder cancer staging. It looks at three main things:
Doctors use these details to find the cancer’s overall stage. This is very important for planning treatment.
Getting the cancer stage right is very important. It helps make sure patients get the right treatment for them, like surgery or chemotherapy.
Accurate staging is important in many ways:
To figure out the cancer stage, doctors use different tests. These include:
These tests give important info about the tumor and how far the cancer has spread. This helps doctors stage the disease accurately and plan the best treatment.
Non-muscle-invasive bladder cancer is found in the bladder lining and has a good survival rate if caught early. It’s divided into stages 0 and I, each with its own survival stats.
Stage 0 bladder cancer has a very good prognosis. It’s split into Ta and CIS (carcinoma in situ). The 5-year survival rate for stage 0 is about 98%.
The American Cancer Society says Ta lesions have a high survival rate. This is because these tumors are usually low-grade and don’t invade deeply.
Stage I bladder cancer has grown from the urothelium into the lamina propria but hasn’t reached the muscle layer. The 5-year survival rate for stage I is about 88%.
This is lower than stage 0 but is considered relatively good, thanks to effective treatments.
To show the survival rates for non-muscle-invasive bladder cancer, here’s a table:
| Stage | 5-Year Survival Rate | Description |
| Stage 0 (Ta/CIS) | 98% | Cancer is confined to the bladder lining |
| Stage I | 88% | Cancer has grown into the lamina propria |
Treatment is key for non-muscle-invasive bladder cancer survival. Treatments include TURBT, intravesical therapy, and sometimes radical cystectomy. The choice depends on the stage, grade, and recurrence risk.
Intravesical BCG therapy can lower recurrence and progression risk in high-risk cases. Good treatment improves survival and quality of life.
Non-muscle-invasive bladder cancer has a high risk of coming back. Regular checks are vital to catch any recurrence early. This includes cystoscopy, imaging, and urine cytology.
Knowing the risks and staying proactive with follow-up care can greatly improve long-term outcomes.
Knowing the survival chances for muscle-invasive bladder cancer is key for both patients and doctors. This cancer has grown into the bladder’s muscle layer, which changes the outlook. The American Cancer Society says the 5-year survival rate is about 69%.
Survival rates for stage II bladder cancer depend on treatment success and the patient’s health. This stage means the cancer has reached the bladder’s muscle but hasn’t spread further. The 5-year survival rate for stage II is a key number doctors use to talk about a patient’s chances.
| Stage | 5-Year Relative Survival Rate |
| Stage II | 63% |
| Localized | 69% |
| Regional | 39% |
Treatment choices for muscle-invasive bladder cancer greatly impact the patient’s future. Radical cystectomy, a surgery to remove the bladder, is a main treatment. Chemotherapy and radiation therapy might also be used, depending on the patient’s situation and wishes.
The treatment chosen can change both survival chances and life quality after treatment. We will look at the different treatments and their effects on patients with muscle-invasive bladder cancer.
Radical cystectomy is a big surgery that affects a patient’s life a lot. It can help control or cure the disease but changes how patients urinate and sometimes have sex. It’s important for patients to know about these changes and the support they can get.
Research shows many patients can live well after radical cystectomy with the right care and support. We will talk about what affects life quality after surgery and how to improve it.
Regional bladder cancer has spread to nearby tissues or lymph nodes. It’s considered advanced but not yet metastatic. Knowing the survival rates is key for patients and doctors to make treatment choices.
The 5-year survival rate for regional bladder cancer is about 39.5%, according to the SEER database. This rate includes cancers that have spread to nearby tissues or lymph nodes but not to distant parts of the body. Survival rates can change based on many factors, like the patient’s health and the tumor’s characteristics.
“Survival rates are not a prediction of individual outcomes but a guide to understanding the general prognosis for a particular stage of cancer,” say cancer research institutions. This helps set realistic expectations and plan treatment.
Lymph node involvement in bladder cancer affects the prognosis. Cancer spreading to lymph nodes means a more advanced stage. Studies show that the number and location of lymph nodes involved can change survival rates. Generally, more lymph nodes involved means a poorer prognosis.
Lymph node involvement makes treatment harder but also offers chances for better outcomes. Knowing how many and where lymph nodes are involved is key for customizing treatment plans.
For regional bladder cancer, a mix of treatments is often recommended. This can include surgery, chemotherapy, radiation therapy, and immunotherapy. The aim is to control the cancer, manage symptoms, and improve quality of life.
Using a mix of treatments can help improve survival for patients with regional bladder cancer. It shows the progress in cancer care and the importance of personalized treatment plans.
Metastatic bladder cancer, also known as stage IV bladder cancer, is a tough challenge in treatment. It has spread to distant parts of the body. This makes treatment harder and affects survival rates.
The 5-year survival rate for metastatic bladder cancer is about 8.8%, according to the SEER database. This shows how serious stage IV bladder cancer is. It highlights the need for aggressive and new treatment methods.
Survival rates can change based on several things. These include the patient’s health, how far the cancer has spread, and how well they respond to treatment. Knowing these stats helps patients and doctors make better care choices.
For patients with metastatic bladder cancer, treatment aims to control symptoms, improve quality of life, and extend life. There are many treatments available, including:
These treatments can be used alone or together to get the best results.
Palliative care is key in managing symptoms and improving life quality for patients with advanced bladder cancer. It focuses on:
Palliative care is important for complete patient care, even when treatments aim to cure.
New research is bringing hope for better outcomes in metastatic bladder cancer. New treatments include:
These new treatments are vital for improving survival rates and life quality for stage IV bladder cancer patients.
We are dedicated to giving our patients the latest and most effective treatments. We want to ensure they get the best care possible.
Many factors beyond the stage of bladder cancer affect survival rates. The stage is important, but other influences are key too.
Age and overall health are big factors in bladder cancer survival. Older patients or those with health issues may find treatment harder. We look at these when predicting patient outcomes.
A study by the American Cancer Society found that health issues can greatly impact survival in bladder cancer patients.
The grade and molecular traits of the tumor are also important. High-grade tumors or those with certain markers may need more aggressive treatment.
Research shows that tumors with specific genetic mutations may react differently to treatments. This can affect survival rates.
There are gender and racial disparities in bladder cancer outcomes. Men are more likely to get bladder cancer, and survival rates vary by race.
| Demographic Group | 5-Year Survival Rate |
| Men | 77% |
| Women | 73% |
| White | 75% |
| Black | 68% |
How well a patient responds to treatment and any complications can greatly affect survival. Effective treatment and managing complications are key to better outcomes.
We understand that each patient’s journey with bladder cancer is unique. By considering all factors, we can tailor treatments to improve survival and quality of life.
Effective treatments are key for bladder cancer patients to live longer. The right treatment depends on the cancer’s stage, grade, and the patient’s health.
Surgery is a main treatment for bladder cancer. There are different surgeries based on the cancer’s stage and how far it has spread. Transurethral resection of bladder tumor (TURBT) is used for early cancer. It removes tumors from the bladder lining without open surgery.
For more serious cases, radical cystectomy might be needed. This surgery removes the bladder and nearby tissues. It can greatly increase survival chances for muscle-invasive bladder cancer patients.
| Surgical Procedure | Description | Indications |
| TURBT | Removal of bladder tumors through the urethra | Early-stage bladder cancer |
| Radical Cystectomy | Removal of the bladder and surrounding tissues | Muscle-invasive bladder cancer |
Non-surgical treatments are also important for bladder cancer. Intravesical chemotherapy puts chemotherapy directly into the bladder. It treats superficial tumors and lowers the chance of them coming back.
Immunotherapy, like Bacillus Calmette-Guérin (BCG), boosts the immune system to fight bladder cancer. These treatments can be used alone or with surgery to better outcomes.
It’s important for bladder cancer patients to know about treatment options. By looking at both surgical and non-surgical methods, patients can work with their doctors. Together, they can create a treatment plan that helps the patient live longer.
After bladder cancer treatment, ongoing care is key. It helps catch any signs of cancer coming back early. This can greatly improve patient outcomes.
Seeing your doctor regularly is important. It helps spot any cancer signs early. How often you see your doctor depends on your cancer type and treatment.
At first, you might see your doctor every few months. This can slow down as time goes on if everything looks good.
A typical monitoring schedule may include:
| Year After Treatment | Frequency of Follow-Up | Tests/Procedures |
| 1-2 | Every 3-6 months | Cystoscopy, Imaging tests |
| 2-5 | Every 6-12 months | Cystoscopy, Laboratory tests |
| 5+ | Annually | Annual check-ups, Imaging tests as needed |
Follow-up care also means dealing with treatment side effects. This can include issues like trouble controlling urine or sexual problems. It’s important to talk to your doctor about any symptoms.
Strategies for managing common side effects include:
Changing your lifestyle can help a lot. Eating well, staying active, and not smoking are all good choices. These habits can lower your chance of cancer coming back.
By sticking to a healthy lifestyle and regular check-ups, you can live a better life after bladder cancer.
Knowing about bladder cancer prognosis is key for patients and their families. It helps them make smart choices about their care. We’ve looked at the different stages of bladder cancer, talked about what affects survival, and covered treatment options.
Survival rates for bladder cancer change a lot based on when it’s found. By learning about these rates, patients can understand their life expectancy better. This knowledge helps them see what to expect from their treatment.
It’s very important to work with your healthcare team. They can help find the best treatment for you. With the right care and support, many people with bladder cancer can have a good outcome.
Survival rates for bladder cancer depend on the stage. Non-muscle-invasive bladder cancer has a high survival rate if caught early.
The 5-year survival rate for bladder cancer varies. It’s high for stages 0 and I but lower for more advanced stages.
The stage of bladder cancer is key to survival rates. Early stages have better chances, while advanced stages have poorer outcomes.
Stage I bladder cancer has a high survival rate. Quick and effective treatment is important.
Survival is influenced by age, health, tumor grade, molecular characteristics, gender, and racial disparities.
Treatment response and complications greatly affect survival. Effective treatment and managing complications can improve outcomes.
Treatments include surgical options like TURBT and radical cystectomy. Non-surgical options include intravesical chemotherapy and immunotherapy.
Follow-up care and surveillance are vital. They help detect recurrence early and manage side effects, improving outcomes.
Lifestyle changes can significantly improve survival. They help reduce recurrence risk and manage side effects.
Life expectancy varies based on stage and other factors. Earlier stages have a better prognosis.
Survival rates vary by stage. Early stages have high rates, while advanced stages have lower rates. Early detection is key.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!