Last Updated on October 21, 2025 by mcelik
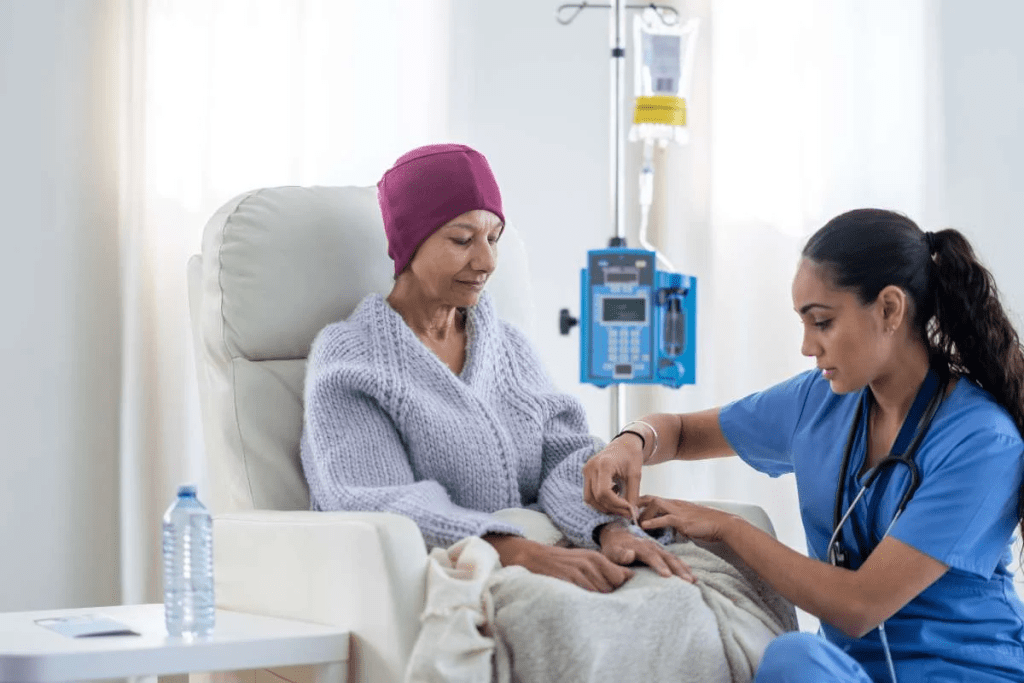
blood and blood iseases :- Chemotherapy is a key treatment for many hematologic disorders. It helps patients all over the world. We aim to give full care and support to those with these conditions.
Recent stats show many patients need chemotherapy for blood ailments. Knowing about these diseases is key for good treatment and care.
We know how important it is to teach patients about blood and blood diseases. This helps them understand their treatment options. It lets them make better health choices.
It’s important to know about blood diseases to treat them well. Blood is key to our health, and problems with it can be serious. We’ll look at different blood diseases and how to treat them, including chemotherapy.
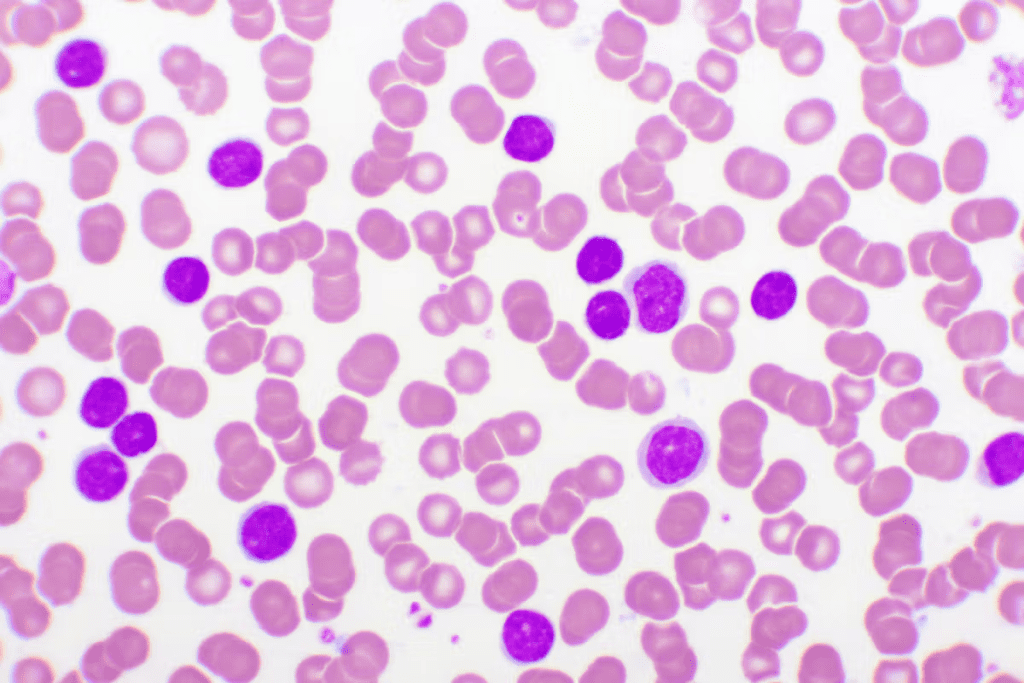
Blood carries oxygen and nutrients and takes away waste. It has parts like red and white blood cells, platelets, and plasma. Each part does something special, and problems with them can cause health issues.
Components of Blood and Their Functions:
| Component | Function |
| Red Blood Cells | Carry oxygen throughout the body |
| White Blood Cells | Play a key role in the immune system |
| Platelets | Involved in blood clotting |
| Plasma | Transports cells, proteins, and other substances throughout the body |
Blood diseases can be non-cancerous or cancerous. Non-cancerous ones include anemia and bleeding disorders. Cancerous ones, like leukemia, need strong treatments, including chemotherapy.
Chemotherapy uses drugs to kill cancer cells. Whether to use it depends on the disease type, stage, and the patient’s health.
We’ll keep exploring blood diseases and treatments. This will give you a full view of hematology’s complex world.
Understanding blood and its disorders is crucial for effective management due to their complexity. We will cover the blood’s parts, common disorders, and the difference between cancerous and non-cancerous conditions.
Blood has several important parts, each vital for our health. These include:
Any problem with these parts can cause serious health issues.
There are many blood disorders, including:
These conditions can greatly affect a person’s life quality.
Leukemia is the most common blood cancer. It needs quick and effective treatment, with chemotherapy being a key part. This cancer makes abnormal white blood cells grow too much, causing health problems if not treated.
There are many types of leukemia, each with its own traits and treatment plans. The main types are:
AML is a fast-growing leukemia that needs quick treatment. Chemotherapy is key in treating AML, aiming to get the cancer into remission and stop it from coming back.
ALL is a fast and aggressive leukemia that needs fast action. Chemotherapy is very important in ALL treatment, often used with other treatments.
CML grows slower and can be managed with specific treatments, like tyrosine kinase inhibitors. Sometimes, chemotherapy is also used.
CLL grows slowly and might not need treatment right away. But when it does, chemotherapy can be effective, often with other treatments.
Chemotherapy is very important in leukemia treatment. It helps many patients get into remission and live longer.
| Type of Leukemia | Characteristics | Treatment Approach |
| AML | Rapidly progressing, abnormal myeloid cells | Chemotherapy, potentially followed by stem cell transplant |
| ALL | Aggressive, abnormal lymphoblasts | Chemotherapy, often with other therapies |
| CML | Slow-progressing, abnormal myeloid cells | Tyrosine kinase inhibitors, potentially chemotherapy |
| CLL | Slow-progressing, abnormal lymphocytes | Watchful waiting, chemotherapy, or targeted therapies |
It’s important to know about the different leukemias and how to treat them. By using chemotherapy and other treatments, we can help people with this complex disease.
Lymphoma is a cancer that starts in the lymphatic system. This system helps fight off infections and diseases. It happens when lymphocytes, a type of white blood cell, grow out of control.
There are two main types of lymphoma: Hodgkin and non-Hodgkin. Knowing the difference is key to finding the right treatment.
Hodgkin lymphoma is rare and moves slowly from one lymph node group to the next. Chemotherapy is a main treatment for Hodgkin lymphoma, often paired with radiation.
Non-Hodgkin lymphoma is more common and has many subtypes. The treatment varies based on the subtype and stage. Chemotherapy is a key part of treating many non-Hodgkin lymphomas, along with targeted and immunotherapies.
Choosing the right treatment for lymphoma depends on several factors. These include the disease type and stage, and the patient’s health. Thanks to advances in blood disorder treatment, lymphoma patients have better outcomes. We’re always looking for new ways to fight this complex disease.
It’s key to understand multiple myeloma and plasma cell disorders to find good treatments. These issues happen when plasma cells in the bone marrow grow too much. This can cause many problems.
Multiple myeloma is a blood cancer that affects plasma cells, which are important for our immune system. It can cause anemia, bone pain, and make us more likely to get sick. Early diagnosis is critical for effective management.
The main signs of multiple myeloma are:
Understanding blood and its disorders is crucial for effective management due to their complexity.
These conditions might turn into multiple myeloma, so regular check-ups are important. The treatment depends on the disorder and how severe it is.
We aim to give the best care for plasma cell disorders, including multiple myeloma. Our team creates treatment plans that meet each patient’s needs. This helps improve their life quality.
Myelodysplastic syndromes (MDS) are complex blood disorders. They affect the bone marrow’s ability to make healthy blood cells. This leads to health problems. We will look at MDS types, risk factors, and how it can get worse.
MDS is divided into types based on the blood cells affected and how severe it is. The main types are:
Several things can make MDS worse or lead to it. These include:
MDS can turn into more serious conditions like acute myeloid leukemia (AML). Knowing these risk factors helps with early diagnosis and treatment.
Myeloproliferative neoplasms (MPNs) are a group of blood disorders. They affect how the bone marrow makes blood cells. This can cause too many blood cells to be made, leading to health problems.
Polycythemia vera makes the bone marrow produce too many red and white blood cells, and platelets. This can make blood thick, raising the risk of blood clots and heart problems.
Essential thrombocythemia causes too many platelets. This can increase the risk of blood clots. Symptoms include headaches, dizziness, and feeling tired.
Primary myelofibrosis replaces bone marrow with fibrotic tissue. This lowers blood cell production. It can cause anemia, fatigue, and more infections.
MPNs can cause serious problems like blood clots, leukemia, and other health issues. Knowing these risks helps manage the condition better.
| MPN Type | Key Characteristics | Common Complications |
| Polycythemia Vera | Overproduction of red blood cells, white blood cells, and platelets | Thrombosis, cardiovascular events |
| Essential Thrombocythemia | Excessive production of platelets | Thrombosis, bleeding complications |
| Primary Myelofibrosis | Bone marrow fibrosis, decreased blood cell production | Anemia, infections, bone marrow failure |
Understanding MPNs and their complications helps doctors create better treatment plans. This way, they can manage these conditions more effectively.
Chemotherapy is not just for cancer. It’s also used for non-malignant blood disorders. These conditions can really affect a person’s life. In some cases, chemotherapy is needed to manage them well.
Severe aplastic anemia is a rare condition where the bone marrow doesn’t make enough blood cells. It’s serious and needs quick treatment. Chemotherapy, along with immunosuppressive therapy, is used to treat it.
Immunosuppressive therapy helps a lot, with success rates between 40% to 70%. Chemotherapy helps the bone marrow to recover.
Hemophagocytic lymphohistiocytosis (HLH) is a rare immune system disorder. It causes too much inflammation and damage to organs. Chemotherapy is key in treating HLH to control the immune system.
“The treatment of HLH involves the use of immunosuppressive and chemotherapeutic agents to control the hyperinflammatory state.”
The treatment for HLH includes etoposide, a chemotherapy drug, and other immunosuppressive medicines. This combo helps manage the condition and improves patient results.
Autoimmune hematologic disorders happen when the immune system attacks the body’s blood cells. Conditions like autoimmune hemolytic anemia and immune thrombocytopenia are serious. Chemotherapy is sometimes used to stop the immune system’s attack.
In these disorders, chemotherapy can help control the immune response. It can ease symptoms and help manage the condition. The chemotherapy choice depends on the disorder and its severity.
Diagnosing blood diseases involves a detailed process. It uses both traditional and modern diagnostic tools. We will look at the steps from noticing symptoms to using advanced tests and assessing risk.
The first step in diagnosing blood diseases is noticing symptoms. Symptoms can be different for each disease but often include feeling tired, losing weight without trying, or getting sick often. Doctors use medical history, physical exams, and initial tests to decide what tests to do next.
Initial tests usually include:
After initial tests show a problem, we use more detailed tests to confirm the diagnosis. These tests help find the exact disease. They include:
After finding out what disease someone has, we stage and assess risk. Staging shows how far the disease has spread. Risk assessment looks at genetic factors, age, and overall health.
For many blood diseases, we use staging systems. These systems divide the disease into stages based on cancer cell count, symptoms, and spread. This helps us create a treatment plan that fits each patient’s needs.
Chemotherapy is a key treatment for blood diseases like leukemia and lymphoma. It targets and kills cancer cells. This helps manage or cure these conditions.
Chemotherapy uses drugs to kill or stop cancer cells from growing. It works by messing with the DNA or RNA of cancer cells. This stops them from multiplying.
Key aspects of chemotherapy’s mechanism of action include:
There are many types of chemotherapy drugs for blood diseases. They are grouped by how they work. Here are a few examples:
| Drug Category | Examples | Mechanism |
| Alkylating Agents | Cyclophosphamide, Chlorambucil | Damage DNA to prevent cell division |
| Anthracyclines | Doxorubicin, Daunorubicin | Interfere with DNA replication |
| Antimetabolites | Methotrexate, Cytarabine | Mimic nutrients needed for cell growth, disrupting cell metabolism |
Chemotherapy can be given in different ways. It depends on the drug and the patient’s health. Here are some common methods:
We pick the best way to give chemotherapy based on the treatment plan and the patient’s health.
Chemotherapy is key in treating blood cancers. Each cancer type gets its own treatment plan. We’ll look at how chemotherapy helps in treating blood cancers, focusing on the treatment stages.
Induction therapy is the first step in treatment. It aims to get the cancer into remission. This phase uses strong chemotherapy to kill cancer cells.
The goal is to make the cancer undetectable. We pick the right chemotherapy drugs for each blood cancer type.
In Acute Myeloid Leukemia (AML), we often use anthracyclines and cytarabine. How well the patient responds to this therapy decides the next steps.
After achieving remission, consolidation therapy aims to get rid of any cancer cells left. This phase is vital to lower the chance of cancer coming back. It might include high-dose chemotherapy or stem cell transplantation.
The choice of consolidation therapy depends on the blood cancer type and how well the patient did in induction therapy. For example, Acute Lymphoblastic Leukemia (ALL) patients might get high-dose chemotherapy and treatments for the central nervous system.
Maintenance therapy is for keeping remission going and stopping cancer from coming back. It uses less intense chemotherapy for a longer time. This therapy is very important for some blood cancers, like Acute Lymphoblastic Leukemia (ALL).
We adjust maintenance therapy based on the patient’s risk and how they did in previous treatments. We aim to keep treatment effective while also considering the patient’s quality of life.
Chemotherapy plans for blood cancers are complex and made just for each patient. Knowing about the different treatment phases is key to managing these diseases well.
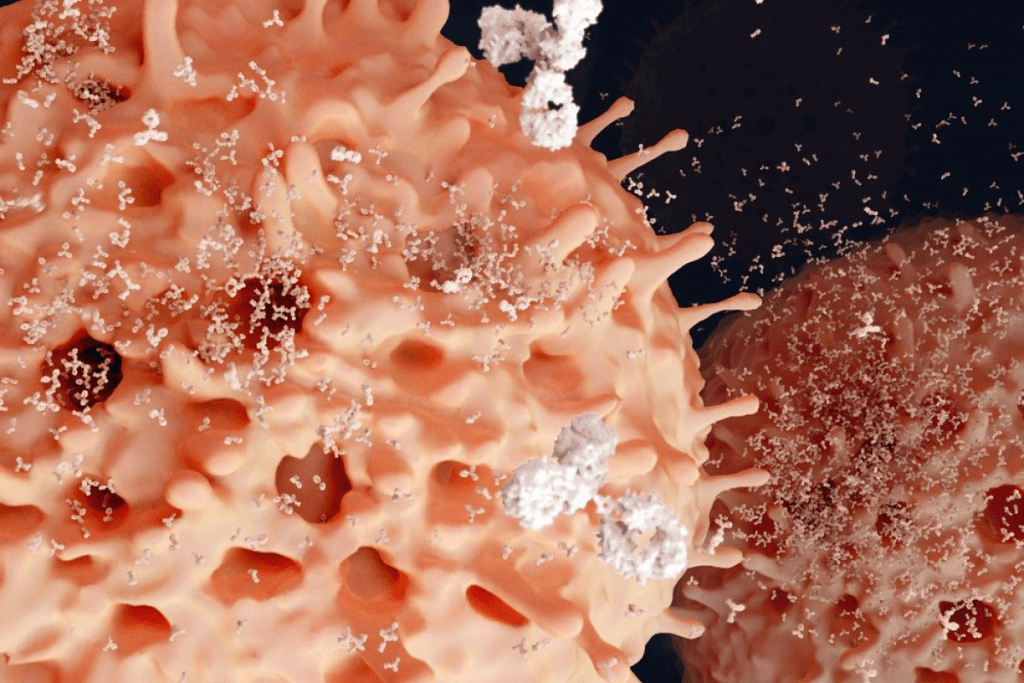
Targeted therapies and immunotherapies are changing how we treat blood diseases. They offer new ways to manage blood disorders. These treatments are more precise and effective.
These treatments use the body’s immune system to fight cancer cells. They are different from traditional chemotherapy. Traditional chemotherapy can harm both healthy and cancerous cells.
Monoclonal antibodies are a promising treatment for blood cancers. They target specific proteins on cancer cells. This makes the immune system destroy them. Rituximab is used to treat lymphomas.
Tyrosine kinase inhibitors (TKIs) have changed how we treat some blood diseases. They block enzymes that help cancer cells grow. Imatinib is used to treat Chronic Myeloid Leukemia (CML).
CAR T-cell therapy is a form of immunotherapy. It modifies T cells to attack cancer cells. This treatment has shown great results in some blood cancers. It’s for patients who haven’t responded to other treatments.
These treatments are a big step forward in treating blood diseases. They offer new hope for patients and their families. They provide more targeted and effective options.
Stem cell transplantation is a key treatment for blood diseases. It gives hope to patients around the world. This method replaces a patient’s sick or damaged stem cells with healthy ones. These can come from the patient or a donor.
Autologous transplants use the patient’s own stem cells. First, stem cells are taken from the patient’s blood or bone marrow. Then, the patient gets high-dose chemotherapy and sometimes radiation to kill the sick cells.
After treatment, the saved stem cells are put back into the patient. This helps the bone marrow work right again.
Benefits of Autologous Transplants:
Allogeneic transplants use stem cells from a donor. This donor can be a family member, someone unrelated, or umbilical cord blood. This transplant is good for genetic blood disorders or severely damaged bone marrow.
The graft-versus-leukemia effect is a big plus of allogeneic transplants. It means the donor’s immune cells fight the cancer cells. But, this transplant also has a higher risk of GVHD.
| Characteristics | Autologous Transplants | Allogeneic Transplants |
| Source of Stem Cells | Patient’s own cells | Donor’s cells |
| Risk of GVHD | Low | High |
| Graft-versus-Leukemia Effect | No | Yes |
The transplant process is detailed and involves many steps. First, patients are checked to see if they can get a stem cell transplant. This includes looking at their health, disease stage, and finding a good donor if needed.
After the transplant, patients need to be watched closely for problems like infections and GVHD. They also get medicines to prevent GVHD and infections while they recover.
Stem cell transplantation is tough, but medical tech and care have improved a lot. Many patients do well. As we keep working on treatments, the outlook for blood disease patients is getting better.
Managing side effects of chemotherapy is key to improving life quality for patients. Chemotherapy is effective against many blood cancers but can cause side effects. These can vary in severity and impact.
Chemotherapy leads to several common side effects, including:
Supportive care is essential in managing chemotherapy side effects. This includes:
Chemotherapy aims to cure or control blood diseases but also has long-term effects. These include:
Understanding and managing these effects can improve patient outcomes and quality of life during and after chemotherapy.
The world of blood disease treatment is changing fast. This is thanks to ongoing clinical trials and new therapies. It’s important to know how clinical trials help create new treatments.
Research in blood diseases is moving forward. It aims to improve patient care with new treatments. Some key areas include:
These new treatments are being tested in clinical trials. They check if these treatments are safe and work well.
Getting into clinical trials is key for patients looking for new treatments. Here’s how to do it:
By learning how to find clinical trials, patients can be more involved in their treatment. They might also get to try new therapies.
Recent advances in treating blood diseases have greatly improved patient results. Studies have shown that treatments like chemotherapy, targeted therapies, and immunotherapies work well. Now, treatments are more personalized, fitting each patient’s unique needs.
New treatment methods and innovative therapies have opened up more options for blood disease treatment. This means patients can now get more effective and targeted care. This leads to better lives and higher survival rates.
It’s vital to keep researching and developing new treatments for blood diseases. By finding new options and improving existing ones, we can keep making care better. This will help those with blood diseases get the best possible treatment.
Hematologic disorders affect the blood, bone marrow, and lymphatic system. Treatment varies by disorder. It may include chemotherapy, targeted therapies, immunotherapies, and stem cell transplantation.
Chemotherapy kills cancer cells. It’s used for blood diseases like leukemia, lymphoma, and multiple myeloma.
Leukemia types include Acute Myeloid Leukemia (AML), Acute Lymphoblastic Leukemia (ALL), Chronic Myeloid Leukemia (CML), and Chronic Lymphocytic Leukemia (CLL). Treatment depends on the type and stage. It may include chemotherapy, targeted therapies, and stem cell transplantation.
Lymphoma is cancer of the lymphatic system. It has two main types: Hodgkin lymphoma and non-Hodgkin lymphoma. Treatment may include chemotherapy, radiation therapy, and immunotherapy.
MDS disorders affect the bone marrow, causing anemia, infection, and bleeding. Treatment may include supportive care, chemotherapy, and stem cell transplantation.
MPNs are disorders that cause the bone marrow to overproduce blood cells. Treatment may include medications to reduce blood cell counts. Chemotherapy and stem cell transplantation may also be used in some cases.
Yes, chemotherapy can treat some non-malignant blood disorders. Examples include severe aplastic anemia and hemophagocytic lymphohistiocytosis (HLH).
Stem cell transplantation is a treatment for blood diseases like leukemia, lymphoma, and multiple myeloma. It replaces the patient’s bone marrow with healthy stem cells. These can come from the patient themselves or a donor.
Managing chemotherapy side effects involves supportive care. This includes medications for nausea and vomiting. It also involves monitoring and managing long-term effects.
Clinical trials offer new treatments and help advance medical knowledge. They contribute to the development of new therapies.
You can find clinical trials online or through healthcare providers. Websites like and patient advocacy organizations are good resources.
Brihi, J. El. (2024). Normal and abnormal complete blood count with differential. National Center for Biotechnology Information. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK604207/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!