Last Updated on October 21, 2025 by mcelik
Did you know that nearly 1 in 3 people who experience a clotting disorder will have another event within 10 years? This shows how important it is to spot clotting disorders early.
We’re here to help you understand clotting disorders and recognize blood clot symptoms before they become serious. These conditions happen when the body can’t form clots right, which can cause too much bleeding or clotting.
It’s key to know the signs and what causes them. Things like family history, some medicines, and health issues can lead to clotting disorders. Knowing this helps us find the right treatment and respond quickly to any blood clot symptoms that appear.

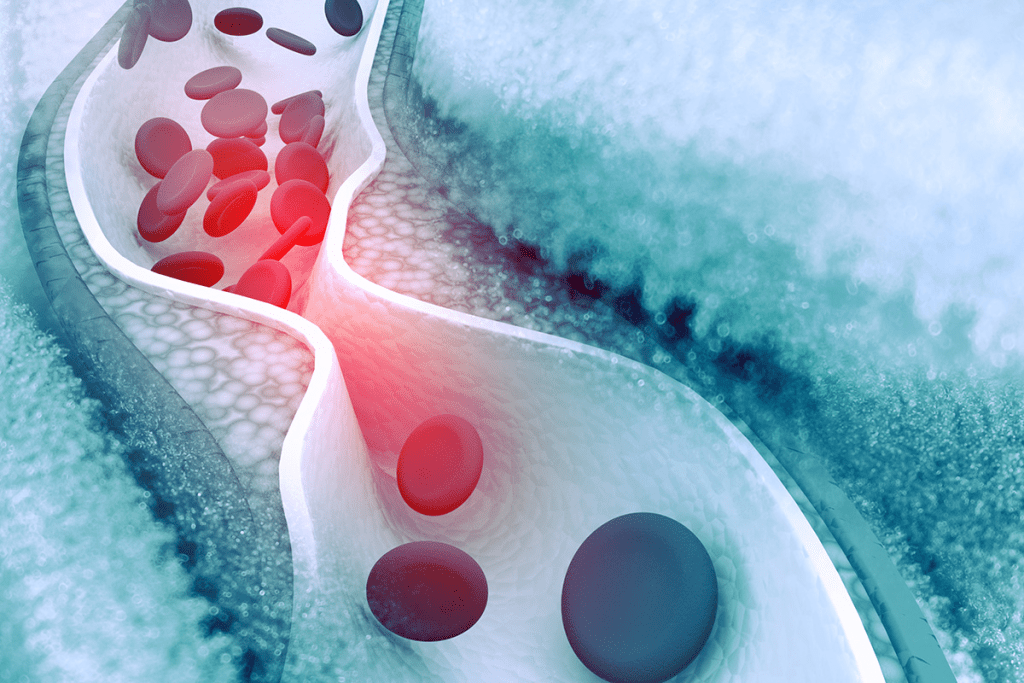
Blood clotting is key to stopping bleeding when we get hurt. But, if it goes wrong, it can cause big health problems. We’ll look at how clotting works normally and what happens when it doesn’t.
The normal clotting process, or hemostasis, is complex. It involves many cells and proteins. When a blood vessel gets hurt, the body first tightens it to cut down blood flow.
Platelets then stick to the injury, making a plug. The coagulation cascade starts, making a fibrin clot. This clot holds the plug in place, stopping too much bleeding.
Clotting is good, but it can be bad if it happens too much or in the wrong place. Clots in the wrong spot can block blood flow. This can lead to serious problems like deep vein thrombosis (DVT) or pulmonary embolism (PE).
Things that can make clots form include genes, some health conditions, and lifestyle choices.

Blood clotting disorders come in many forms. We’ll look at the most common ones. We’ll learn about their characteristics and what they mean.
Factor V Leiden is a genetic disorder that raises the risk of blood clots. It’s caused by a gene mutation. This condition is more common in people of European descent.
The Prothrombin Gene Mutation affects how prothrombin is made. Prothrombin is a clotting factor. This mutation can cause more prothrombin to be made, raising the risk of blood clots.
Protein C and Protein S are proteins that help control blood clotting. Without enough of these proteins, the risk of blood clots goes up. These deficiencies are often passed down through families.
Antithrombin is a protein that helps manage blood clotting. Without enough antithrombin, the risk of blood clots increases. This condition is usually inherited.
| Disorder | Cause | Risk |
| Factor V Leiden | Genetic mutation in F5 gene | Increased risk of blood clots |
| Prothrombin Gene Mutation | G20210A mutation | Elevated prothrombin levels, increasing thrombosis risk |
| Protein C and S Deficiencies | Inherited deficiencies | Increased risk of blood clots |
| Antithrombin Deficiency | Inherited deficiency | Significantly increased risk of thrombosis |
Many things can make you more likely to get blood clots. This includes your genes and how you live. Knowing what these factors are is key to stopping blood clots before they start.
Genes can really affect your risk of blood clots. Some people are born with conditions that make their blood clot more easily. Factor V Leiden and Prothrombin Gene Mutation are two common ones.
If your family has a history of blood clots, you might be at higher risk. It’s a good idea to talk to your doctor about this. They can help you figure out what you can do to stay safe.
How you live can also raise your risk of blood clots. For example, sitting for a long time can make clots more likely. Smoking, being overweight, and not moving enough are other risks.
Changing these habits can help lower your risk. Try to move more, eat well, and avoid smoking. These steps can make a big difference.
Some health issues can also up your risk of blood clots. This includes cancer, heart disease, and problems with blood flow. For instance, irregular heartbeats can lead to clots in the heart.
| Risk Factor | Description | Prevention/ Management |
| Genetic Predisposition | Inherited conditions affecting blood clotting | Consult healthcare provider, potentially anticoagulant therapy |
| Prolonged Immobility | Long periods of inactivity, e.g., during travel or bed rest | Regular movement, compression stockings |
| Smoking and Obesity | Lifestyle factors that increase clotting risk | Smoking cessation, weight management |
Knowing and dealing with these risks can help prevent blood clots. It’s vital to stay aware and take steps to manage these factors. This way, you can avoid the problems that come with blood clots.
It’s important to know the signs of a blood clot to get help quickly. Blood clots can happen in different parts of the body. Their symptoms can change based on where they form.
Common signs of blood clots include swelling and pain in a limb. You might also feel warmth and redness. A heavy or aching feeling in the area is another symptom.
Being aware of these signs is key. They can mean you have a blood clot.
Some symptoms are more serious and need quick medical help. Chest pain or trouble breathing could mean a pulmonary embolism. This is a serious condition.
Sudden numbness or weakness in your face or limbs is also a warning sign. It’s important to see a doctor right away if you notice these symptoms.
Deep Vein Thrombosis is a serious condition where a blood clot forms in a deep vein, usually in the legs. It’s important to recognize the symptoms early for proper treatment.
Pain or tenderness in the leg is a key sign of DVT. The pain can be mild or severe. Swelling also occurs, making it hard to walk or stand.
Look out for redness or discoloration of the skin around the affected area too.
If you notice any of these symptoms, get medical help right away. Early treatment can prevent serious complications.
Pulmonary embolism is a serious condition. It happens when a blood clot from the legs goes to the lungs. This can block blood flow and cause severe damage or even death. It’s important to know the symptoms and get medical help right away.
The symptoms of pulmonary embolism can vary. They often include sudden shortness of breath and chest pain that gets worse with deep breathing. Coughing up blood is another symptom. These signs are serious and need quick action.
Breathing problems are a key symptom of pulmonary embolism. People may feel like they can’t breathe or are suffocating. The chest pain can be sharp and stabbing, getting worse with deep breaths or coughing.
Other symptoms include a fast heart rate, feeling lightheaded, or fainting. In severe cases, it can even lead to cardiac arrest.
| Symptom | Description |
| Shortness of Breath | Sudden difficulty breathing |
| Chest Pain | Sharp pain that worsens with deep breathing |
| Rapid Heart Rate | Increased heart rate |
Blood clots can show up in unexpected places in the body. This is why it’s important to get medical help right away. While many know about deep vein thrombosis (DVT) in the legs, clots can also form in other areas. This makes diagnosis and treatment tricky.
Cerebral venous thrombosis is a blood clot in the brain’s venous sinuses. It’s rare but serious. Symptoms include severe headaches, confusion, and seizures. This condition often affects younger people, like children and pregnant women.
Key symptoms to watch for:
Clots can also form in the veins of the arm. This is less common than DVT in the legs. Symptoms include pain, swelling, and discoloration in the affected arm.
| Symptom | Description |
| Pain | Aching or cramping sensation in the arm |
| Swelling | Noticeable swelling of the arm or hand |
| Discoloration | Redness or bluish discoloration of the skin |
Blood clots can also occur in the abdominal veins. This is known as portal vein thrombosis when it affects the vein to the liver. Symptoms include abdominal pain, nausea, and fever. Diagnosis often needs imaging studies.
“The diagnosis of abdominal blood clots can be challenging due to the nonspecific nature of the symptoms, requiring a high index of suspicion and appropriate imaging techniques.”
In conclusion, blood clots in unusual locations are hard to diagnose because of their varied symptoms. It’s important for healthcare providers and patients to be aware of these conditions. This ensures timely and proper treatment.
Diagnosing blood clotting disorders is a detailed process. It includes a thorough medical history, physical examination, and various tests.
A physical examination is the first step. Healthcare providers look for signs like swelling, redness, or warmth in the affected limb.
Blood tests are key in diagnosing clotting disorders. Important tests include:
Imaging studies are vital for confirming the diagnosis and assessing the extent of the clot. Common techniques include ultrasound, CT scans, and MRI.
Ultrasound is often used to diagnose DVT. CT scans can help identify clots in the lungs or other areas. MRI can be used to visualize clots in the brain or other areas.
Diagnostic test results give you key insights into how your body clots blood. When you get your test results, it’s important to know what they mean for your health and treatment.
Your doctor might run different tests to find out if you have a blood clotting disorder. These tests check clotting factor levels and do genetic testing. Let’s look at what these tests show about your condition.
Clotting factor levels show how your blood clots. If these levels are off, it could mean you have a clotting disorder. Here’s what different test results might show:
| Test | Normal Range | Abnormal Result Indication |
| Prothrombin Time (PT) | 10-14 seconds | Clotting factor deficiency or anticoagulant effect |
| Activated Partial Thromboplastin Time (aPTT) | 25-35 seconds | Coagulation pathway abnormalities or heparin effect |
| Fibrinogen Level | 200-400 mg/dL | Dysfibrinogenemia or afibrinogenemia |
Knowing these test results helps your doctor create a treatment plan just for you.
Genetic testing can find inherited conditions that affect blood clotting. This info is key for knowing your risk and taking steps to prevent problems.
Some common genetic mutations linked to clotting disorders include:
Genetic testing can give you clarity on your condition. It helps your doctor suggest the best ways to manage it.
By understanding your test results, you can play a big role in managing your health. It’s important to talk about your results with your doctor to make sure you’re on the right path.
Managing blood clotting disorders requires a variety of treatments. Each plan is made to fit the person’s condition and medical history. The goal is to stop new clots from forming and prevent existing ones from growing. This helps lower the risk of serious health problems.
Anticoagulant medications are key in treating blood clotting disorders. They stop new clots from forming and prevent existing ones from getting bigger. Common types include warfarin, apixaban, rivaroxaban, and dabigatran.
Thrombolytic therapy is used in severe cases. It’s when there’s a big risk to health. This treatment involves drugs that break down the clot.
Surgery is an option when other treatments don’t work. It can include removing clots or fixing damaged blood vessels.
New research is looking into better treatments. This includes new anticoagulants and gene therapy. The aim is to offer safer and more effective ways to manage blood clotting disorders.
Untreated blood clotting disorders can lead to serious health problems. These issues can affect a person’s quality of life and overall health. It’s important to manage these disorders to avoid complications.
Short-term complications can be severe and even life-threatening. One major risk is deep vein thrombosis (DVT). This can cause a pulmonary embolism if the clot moves to the lungs.
Symptoms of DVT include leg pain, swelling, and redness. A pulmonary embolism can cause sudden shortness of breath, chest pain, and even loss of consciousness. It’s vital to seek medical help quickly.
Another risk is stroke. It happens when a blood clot forms in the brain or travels there. Symptoms include sudden weakness, difficulty speaking, vision changes, and severe headache. Quick medical care is essential to reduce damage.
Long-term risks are also serious. Recurrent DVT and pulmonary embolism can lead to chronic health issues. One such issue is post-thrombotic syndrome, causing chronic pain, swelling, and skin ulcers.
People with untreated blood clotting disorders also face a higher risk of chronic thromboembolic pulmonary hypertension (CTEPH). This condition raises blood pressure in the pulmonary arteries due to chronic clots. It can cause right heart failure and reduce exercise tolerance and quality of life.
Managing these risks often requires long-term anticoagulation therapy. In some cases, surgery may be needed to address complications like CTEPH.
Living with a blood clotting disorder means you need to manage your life carefully. You must understand your condition, make lifestyle changes, and watch out for complications.
When you have a blood clotting disorder, you need to be careful with your body. Drinking water, avoiding sitting too long, and wearing comfy clothes can help a lot. Keeping a healthy weight and doing gentle exercises also improve blood flow.
It’s important to plan your day around your meds and doctor visits. Use a calendar or reminders to stick to your treatment plan.
Monitoring your condition over time is key. Regular blood tests check if your meds are working right. Working with your doctor to adjust your treatment is vital.
Knowing the signs of serious problems like DVT or pulmonary embolism is important. Learning about your condition helps you manage it better.
The emotional side of having a blood clotting disorder is real. It can cause anxiety and make you feel scared or vulnerable. Having support from loved ones or groups can help a lot.
Handling the emotional side means staying positive and informed. Try stress-reducing activities like meditation or yoga. Celebrating small wins is also important.
By being proactive and informed, people with blood clotting disorders can live well. They can reduce the condition’s impact on their daily life and overall health.
To lower the risk of blood clots, it’s key to mix healthy habits with preventive meds if needed. Knowing what causes blood clots helps us take steps to stop them.
Changing your lifestyle can greatly cut down blood clot risk. Here are some important changes:
Knowing your risk factors and talking to your doctor is also vital. For example, a family history of clotting disorders means you should be extra careful.
For some, lifestyle changes might not be enough to stop blood clots. In these cases, meds can help.
Following your doctor’s advice on meds is critical. They tailor advice to your risk and health history.
Combining lifestyle changes with meds when needed can greatly lower blood clot risk. Regular check-ups and advice from healthcare providers are also key to managing clotting disorders.
It’s important to know when to get help fast if you have a blood clotting disorder. If you see any of these serious signs, get emergency care right away.
Some symptoms mean you need help fast. Watch out for these red flags:
If you’re in a medical emergency, call your local emergency number. Or have someone take you to the nearest emergency room. Don’t drive yourself unless you have to. If you’re feeling very sick, stay calm and follow these steps:
It’s key to understand blood clotting disorders early on. This helps in managing them effectively. We’ve looked at different types of clotting disorders, their causes, and signs of trouble.
Knowing the warning signs of blood clots is vital. These include leg pain and swelling, breathing issues, and chest pain. Tests like blood tests and imaging studies help find these disorders.
Treatment options are available to lower the risk of serious problems. These range from medicines to surgery. Making lifestyle changes and taking preventive steps can also help manage the condition.
If symptoms don’t go away or get worse, seek medical help right away. With the right care, people with blood clotting disorders can live active and healthy lives.
Symptoms include leg pain or swelling, and redness or discoloration. You might also feel warmth or tenderness. In severe cases, you could have chest pain, shortness of breath, or cough up blood.
Look for swelling, pain, or tenderness in one leg. Also, watch for redness or discoloration, and warmth or heaviness. If you notice these signs, get medical help right away.
Blood clots can form due to genetic factors, lifestyle choices, or medical conditions. Prolonged immobility or smoking can increase your risk. Conditions like cancer or clotting disorders also play a role.
Yes, you can prevent blood clots by making lifestyle changes. Regular exercise, maintaining a healthy weight, and avoiding prolonged immobility are key. In some cases, preventive medications are prescribed.
Diagnosis involves a physical exam, blood tests, and imaging studies. Ultrasound or CT scans are often used to check for clots.
Treatment options include anticoagulant medications and thrombolytic therapy. Surgery and emerging treatments are also available. The right treatment depends on the clot’s severity and location.
Untreated disorders can lead to short-term complications like pulmonary embolism. Long-term risks include post-thrombotic syndrome and chronic thromboembolic pulmonary hypertension.
Managing daily activities means taking your medications as prescribed. Monitor your condition closely and make lifestyle changes to reduce clot risk.
Seek emergency care for severe symptoms like difficulty breathing, chest pain, or severe leg pain. Also, get help if you suspect a pulmonary embolism.
Yes, but talk to your healthcare provider first. They will help determine the right level of physical activity and any necessary precautions.
Yes, new treatments are being developed. These include new anticoagulant medications and innovative therapies to improve patient outcomes.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!