Last Updated on October 21, 2025 by mcelik
Did you know millions of people worldwide suffer from blood diseases? These can really change their life quality. These diseases affect the blood and stop it from working right.
We’ll look at the most common blood disorders. This includes anemia and bleeding disorders like hemophilia. Knowing about these is key for the right treatment.
Key Takeaways
- Millions worldwide are affected by various blood diseases.
- Blood disorders can significantly impact quality of life.
- Common blood disorders include anemia and bleeding disorders.
- Understanding these conditions is crucial for proper diagnosis and treatment.
- There are several types of blood diseases that will be discussed.
Understanding Blood and Its Components

A highly detailed, 3D digital illustration of the internal components of human blood, including red blood cells, white blood cells, platelets, and plasma, showcased in a cutaway view against a dark, minimalist background with a focus on the intricate, microscopic structures and textures of each element. The lighting is dramatic and evocative, casting shadows and highlights to enhance the sense of depth and dimension. The composition is carefully balanced, with the various blood components arranged in an organized and visually compelling manner. The overall mood is one of scientific precision and medical exploration, conveying a sense of the complexity and importance of blood within the human body.
Blood is a living tissue made of different parts that keep us healthy. It has a liquid part called plasma and solid parts like red and white blood cells, and platelets.
The Composition of Blood
Most of blood is plasma, making up about 55%. Plasma is mostly water, salts, and proteins. The solids include red blood cells for oxygen transport, white blood cells for fighting infections, and platelets for clotting.
Functions of Blood in the Human Body
Blood does many important jobs in our bodies. It carries oxygen and nutrients to cells and organs and takes away waste. It also helps control body temperature and keeps the body’s acid-base balance.
The parts of blood work together for our bodies to function well. Red blood cells carry oxygen, white blood cells fight infections, and platelets stop bleeding. Knowing how blood works helps us understand its health and disorders.
Common Blood Disorders: An Overview
A detailed, high-resolution medical illustration depicting four common blood disorders. The foreground showcases magnified cellular-level views of red blood cells, white blood cells, and platelets affected by conditions like anemia, leukemia, and thrombocytopenia. The middle ground features diagrams and infographics highlighting the underlying mechanisms and symptoms of these disorders. The background provides an atmospheric healthcare setting with subtle medical equipment and a muted color palette to convey a sense of study and analysis. Bright, directional lighting casts dramatic shadows to enhance the scientific precision. Rendered with a photorealistic aesthetic using advanced 3D modeling and textural details.
Blood disorders affect how blood works. They can change how blood cells are made, work, or last. This includes red, white blood cells, and platelets.
Definition and Classification of Blood Disorders
Blood disorders stop blood from doing its job. This can lead to problems with clotting or bleeding. Blood disorders are grouped by the type of blood cell and the problem it causes.
Some common types include:
- Anemia and other red blood cell disorders
- Leukemia and other white blood cell disorders
- Bleeding disorders, such as hemophilia
- Clotting disorders
Impact on Global Health
Blood disorders affect millions globally. They vary in how common they are in different places.
| Disorder | Prevalence | Global Impact |
| Anemia | Affects approximately 30% of the global population | Significant cause of morbidity worldwide |
| Leukemia | Affects about 5% of all cancer patients | Major contributor to cancer-related deaths |
| Hemophilia | Rare, affecting about 1 in 5,000 male births | Significant impact on quality of life for affected individuals |
Risk Factors and Predispositions
Knowing what increases the risk of blood disorders is key. This includes genetics, environment, and lifestyle.
Healthcare providers can use this knowledge to help those at risk. They can take steps to prevent these disorders.
Anemia: The Most Common Blood Disorder
A examination room with modern medical equipment and diagnostic tools. In the foreground, a close-up view of a healthcare professional’s hands drawing blood from the patient’s arm, with a tourniquet and syringe visible. The middle ground shows the patient, a middle-aged person, sitting upright and attentive, their expression conveying concern. The background features a detailed wall-mounted chart depicting the various stages and symptoms of anemia, complemented by anatomical diagrams and medical references. Soft, directional lighting illuminates the scene, creating a sense of professionalism and attention to detail. The overall atmosphere conveys the gravity and importance of the anemia diagnosis process.
Anemia is a common condition found in millions around the world. It happens when there’s not enough red blood cells or hemoglobin. This makes it hard to get enough oxygen to our bodies, affecting our daily lives.
There are many types of anemia, each with its own cause and effects. We group them based on how they happen.
Types of Anemia
Here are some common types of anemia:
- Iron-deficiency anemia: This is the most common type. It’s often caused by not eating enough iron or losing blood too much.
- Vitamin deficiency anemia: This happens when we don’t get enough vitamins like B12 or folate.
- Anemia of chronic disease: This is linked to long-term illnesses like rheumatoid arthritis or cancer.
- Sickle cell anemia: A genetic disorder that affects how our bodies make hemoglobin.
Each type needs a specific treatment plan.
Symptoms and Diagnosis
Symptoms of anemia can be different for everyone. They often include feeling very tired, weak, and pale. A complete blood count (CBC) is usually used to diagnose anemia. It checks the number of red blood cells and hemoglobin levels.
| Symptom | Description |
| Fatigue | A persistent feeling of tiredness or lack of energy. |
| Weakness | Muscle weakness that can impair physical performance. |
| Pale Skin | A decrease in the normal skin color due to reduced hemoglobin. |
Treatment Options
Treatment for anemia depends on its cause. It might include changing what we eat, taking supplements, or treating other health issues. Sometimes, blood transfusions are needed to quickly increase red blood cells.
Knowing about the different types of anemia helps give better care. This improves how patients feel and live their lives.
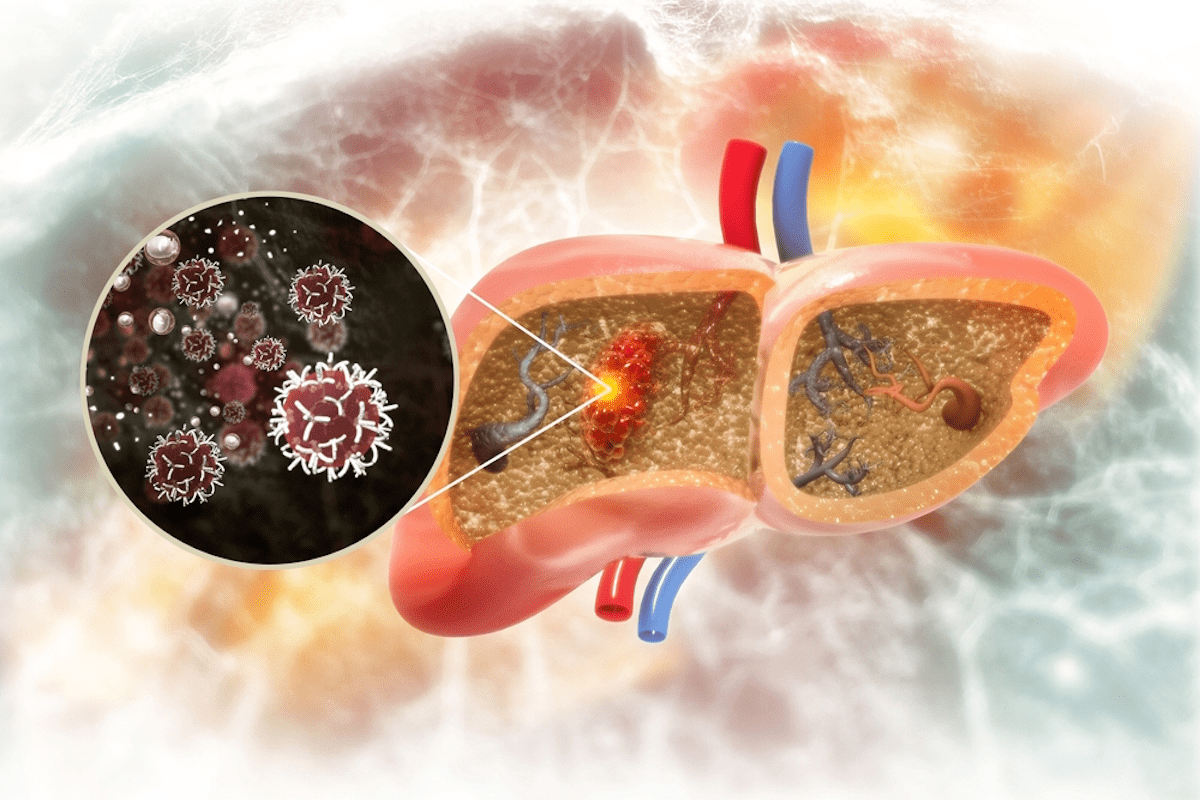
Leukemia: Cancer of the Blood
A detailed close-up of a cancerous leukemia blood cell, illuminated under a bright microscope lens. The cell’s irregular shape, enlarged nucleus, and abnormal chromatin structure are clearly visible against a stark black background. Subtle yet ominous red and orange hues cast an unsettling glow, evoking the serious nature of the disease. The image is crisp, high-resolution, and scientifically accurate, capturing the essence of leukemia at the cellular level.
Leukemia is a blood cancer that affects the body’s immune system. It happens when white blood cells grow too much. These cells are made in the blood and bone marrow.
Different Forms of Leukemia
There are four main types of leukemia: Acute Lymphoblastic Leukemia (ALL), Acute Myeloid Leukemia (AML), Chronic Lymphocytic Leukemia (CLL), and Chronic Myeloid Leukemia (CML). ALL is common in kids, while AML affects adults more. CLL and CML are slower-growing and mostly seen in older adults.
Each type needs its own treatment. For example, ALL needs quick action with chemotherapy and targeted therapy.
Risk Factors and Causes
Leukemia’s exact cause is still a mystery. But we know some risk factors. These include radiation, genetic disorders, and past treatments. Genetic mutations are also key, with some passed down through families.
Other risks include age and environmental factors like benzene. Knowing these risks helps us catch and prevent leukemia early.
Modern Treatment Approaches
Today’s leukemia treatments are much better. Chemotherapy is still a mainstay, often paired with targeted therapy. This targets specific cancer growth factors.
Immunotherapy is also promising, using the body’s immune system against leukemia. Sometimes, stem cell transplantation is needed for high-risk cases.
We’re always learning more about leukemia and finding new treatments. By using these modern methods, we can help patients live better lives.
Hemophilia: When Blood Doesn’t Clot
A close-up view of a human hand with visible bruises and red splotches, representing the uncontrolled bleeding associated with hemophilia. The hand is positioned against a neutral, soft-focus background, creating a sense of vulnerability and emphasis on the medical condition. Warm, diffused lighting illuminates the hand, casting subtle shadows that highlight the skin’s texture and imperfections. The image conveys a sense of delicacy and the challenges faced by individuals living with this blood disorder.
Hemophilia is a genetic disorder that makes it hard for blood to clot. This leads to long-lasting bleeding. It happens because the body lacks proteins needed for clotting, called clotting factors.
Genetic Basis of Hemophilia
Hemophilia is mainly caused by gene mutations in clotting factors VIII (Hemophilia A) or IX (Hemophilia B). These genes are on the X chromosome. This makes hemophilia mostly affect males, as it’s an X-linked recessive disorder.
The genetic problem means less or no clotting factor is made. This stops blood from clotting properly. Knowing the genetics is key for diagnosis and planning families.
Living with Hemophilia
Managing hemophilia means getting regular infusions of clotting factors to stop bleeding. People with hemophilia must also be careful to avoid injuries. They might need to change their lifestyle to reduce bleeding risks.
Support from , family, and support groups is crucial. It helps manage the condition and improves life quality.
Advances in Hemophilia Treatment
New treatments for hemophilia include recombinant clotting factors. These reduce disease transmission risks. Gene therapy is also being explored as a cure, aiming to fix the genetic issue.
Treatment Options:
| Treatment Type | Description | Benefits |
| Recombinant Clotting Factors | Produced through genetic engineering | Reduced risk of infectious disease transmission |
| Gene Therapy | Aims to correct the genetic defect | Potential for a cure, reduced treatment frequency |
| Prophylactic Treatment | Regular infusions to prevent bleeding | Reduces frequency of bleeding episodes |
These new treatments bring hope for better management and a possible cure for hemophilia in the future.
Sickle Cell Disease: An Inherited Blood Disorder
A detailed anatomical illustration of sickle cell disease pathophysiology, depicting red blood cells with a characteristic sickle-like shape. The foreground should showcase the abnormal hemoglobin molecules causing the distorted red blood cell structure. The middle ground should illustrate the vascular occlusion and reduced blood flow resulting from the sickle-shaped cells. The background should provide a contextual medical setting, such as a cross-section of a blood vessel or tissue, to provide a clear understanding of the condition. Render the image in a realistic, high-quality photorealistic style, with accurate anatomical details and lighting that enhances the scientific and medical nature of the subject.
Sickle cell disease is a genetic disorder that affects how red blood cells work. It changes how hemoglobin is made, leading to health problems.
Pathophysiology of Sickle Cell Disease
This disease comes from a gene change in the HBB gene. This change makes abnormal hemoglobin, or HbS. When HbS doesn’t have enough oxygen, it forms clumps. This makes red blood cells bend into a sickle shape.
These sickle-shaped cells break down easily and can block blood vessels. This can cause tissues to not get enough blood.
Complications and Management
People with sickle cell disease face many health issues. These include pain episodes, infections, and damage to organs. To manage these, use:
- Regular check-ups and care
- Hydroxyurea to lessen pain episodes
- Blood transfusions to reduce sickle red blood cells
- Support during pain episodes
The table below shows common problems and how to handle them:
| Complication | Management Strategy |
| Acute Pain Episodes | Supportive care, hydration, pain management |
| Infections | Prophylactic antibiotics, vaccinations |
| Organ Damage | Regular monitoring, specific organ support |
Research and Future Treatments
Scientists are working hard to find new treatments for sickle cell disease. They’re looking into gene therapy, new medicines, and better care. These could lead to better lives for those with the disease.
We aim to bring the latest in treating inherited blood disorders like sickle cell disease. Understanding and managing the disease can greatly improve patient care.
Thrombocytopenia: Low Platelet Count
A detailed microscopic view of red blood cells and platelets, with a focus on the decreased presence of platelets characteristic of thrombocytopenia. The image should convey a , medical atmosphere, with a depth of field that highlights the foreground elements while softening the background. Utilize realistic lighting and textures to enhance the scientific, diagnostic nature of the scene. The color palette should lean towards muted, subdued tones that evoke a sense of seriousness and professionalism. An overall sense of precision and attention to detail should permeate the composition.
A low platelet count, known as thrombocytopenia, can cause serious bleeding. It happens when there are not enough platelets in the blood. Platelets are key for blood to clot, and without enough, bleeding can last a long time.
Causes and Risk Factors
Thrombocytopenia can come from many sources. These include problems with the bone marrow, certain medicines, and autoimmune diseases. We will look into these causes to understand how they lead to thrombocytopenia.
- Bone marrow disorders affecting platelet production
- Medications that interfere with platelet production or function
- Autoimmune diseases where the immune system attacks platelets
The symptoms of thrombocytopenia can differ based on how severe it is. Common signs include:
- Easy bruising and petechiae (small spots on the skin)
- Prolonged bleeding from cuts or injuries
- Nosebleeds or bleeding gums
In severe cases, thrombocytopenia can cause dangerous bleeding.
Treatment Approaches
Treatment for thrombocytopenia depends on the cause and how severe it is. We will talk about different treatments, such as:
| Treatment | Description |
| Medications | Corticosteroids or immunoglobulins to boost platelet count |
| Platelet Transfusions | Transfusing platelets to temporarily increase platelet count |
| Splenectomy | Surgical removal of the spleen in severe cases |
A hematologist says, “Managing thrombocytopenia needs a full plan, including diagnosis, treatment, and lifestyle changes.”
“The key to managing thrombocytopenia is early diagnosis and proper treatment to avoid complications.”
Polycythemia: Excess Red Blood Cells
Understanding polycythemia is key to managing it well. This condition makes the body produce too many red blood cells. It can make blood thicker, leading to heart problems and other health issues.
Primary vs. Secondary Polycythemia
There are two types of polycythemia: primary and secondary. Primary polycythemia, or polycythemia vera, is a rare blood cancer. It causes the bone marrow to make too many red blood cells. Secondary polycythemia happens due to things like low oxygen or tumors that make more red blood cells.
Symptoms and Complications
Symptoms of polycythemia include headaches, dizziness, and itching. Problems like blood clots and heart issues can also happen. It’s important to manage these symptoms and prevent complications.
Treatment Strategies
Treatment for polycythemia focuses on lowering blood viscosity. This can be done through phlebotomy, medicines to slow bone marrow, and treating underlying causes. These steps help prevent serious problems.
Lymphoma: Cancer of the Lymphatic System
Lymphoma is a cancer that affects the immune system. It starts in the lymph system, which is part of our immune system.
Hodgkin vs. Non-Hodgkin Lymphoma
Lymphoma is divided into two main types: Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL). Hodgkin lymphoma has Reed-Sternberg cells. Non-Hodgkin lymphoma does not have these cells. Knowing the difference is key for the right treatment.
Diagnosis and Staging
To diagnose lymphoma, use physical exams, imaging tests, and biopsies. The disease’s extent determines its stage. Accurate staging is vital for choosing the best treatment.
Treatment Options
Treatment for lymphoma varies based on the type and stage. It can include chemotherapy, radiation, immunotherapy, or a mix. Targeted therapies and immunotherapies offer new hope.
We aim to provide top-notch care for lymphoma patients. We use the latest medical science to improve their outcomes.
Diagnosis and Testing for Blood Disorders
Diagnosing blood disorders requires different tests and techniques. We will look at how these methods help identify conditions. This ensures patients get the right care.
Common Blood Tests
Blood tests are key in finding blood disorders. Here are some common ones:
- Complete Blood Count (CBC): Checks blood components like red and white cells, hemoglobin, and platelets.
- Blood Smear: Looks at blood cell shapes to spot issues.
- Coagulation Tests: See if blood can clot, helping find problems like hemophilia.
These tests give important info about the patient’s health. They help decide on the next steps for treatment.
Advanced Diagnostic Techniques
There are also advanced tests for complex blood disorders. Some include:
- Molecular Testing: Finds genetic changes linked to blood disorders.
- Flow Cytometry: Studies blood cells to diagnose diseases like leukemia.
- Cytogenetic Analysis: Looks at blood cell chromosomes for abnormalities.
Using these tests together helps accurately diagnose and treat blood disorders. This leads to better health outcomes for patients.
Treatment Approaches for Blood Disorders
Managing blood disorders well needs a deep understanding of treatment options. These disorders are complex and varied. So, treatments must be specific to each condition and patient.
Medication Therapies
Medicine is key in treating many blood disorders. For example, anticoagulant medications stop blood clots. Clotting factor concentrates help those with hemophilia clot their blood. Also, immunosuppressive drugs treat aplastic anemia by calming the immune system’s attack on the bone marrow.
Blood Transfusions
Blood transfusions are a common treatment for many blood disorders. They help with deficiencies or abnormalities in blood cells. Red blood cell transfusions treat anemia and boost oxygen to tissues. Platelet transfusions prevent or treat bleeding in patients with low platelets.
Stem Cell Transplantation
Stem cell transplantation, like bone marrow transplantation, can cure some blood disorders. It replaces the patient’s sick bone marrow with healthy stem cells. These can come from the patient (autologous transplant) or a donor (allogeneic transplant).
Emerging Treatments
New treatments for blood disorders are being researched. Gene therapy tries to fix genetic problems in these disorders. Other new methods include targeted therapies and immunotherapies that use the immune system to fight blood cancers.
Every patient is different, and treatments are made just for them. Knowing all the treatment options helps give the best care for blood disorders.
Living with Blood Disorders: Coping Strategies
Coping with a blood disorder requires a mix of medical care, psychological support, and lifestyle changes. It’s tough, but the right strategies can help people live well despite their condition.
Psychological Impact
Getting a blood disorder diagnosis can really affect your mind. Many feel anxious, depressed, or lonely. Recognizing these feelings is the first step to healing. Getting professional help is key to managing your mental health.
Support Systems and Resources
Having a strong support network is crucial. This includes family, friends, support groups, and . Support groups provide a sense of community and understanding that’s really helpful. Using resources like counseling and educational materials can also help you understand and manage your condition.
Lifestyle Adaptations
Changing your lifestyle can greatly improve life with a blood disorder. This might mean eating differently, exercising regularly, and avoiding activities that could make things worse. Working with your healthcare team to create a care plan is vital for managing your condition well.
| Lifestyle Adaptation | Benefit |
| Dietary Changes | Improves overall health and can help manage symptoms |
| Regular Exercise | Enhances physical and mental well-being |
| Avoiding Risky Activities | Reduces the risk of complications associated with the blood disorder |
By using these coping strategies and making lifestyle changes, people with blood disorders can live better and manage their condition more effectively.
Prevention and Risk Reduction
To prevent blood disorders, we need to understand genetic risks and make healthy choices. Regular health screenings are also key. By being proactive, we can lower our risk of these conditions.
Genetic Counseling
Genetic counseling is very important for those worried about inherited blood disorders. Genetic testing and family history analysis help counselors give valuable advice. This advice is based on your genetic risks.
Lifestyle Modifications
Living a healthy lifestyle is crucial to avoid blood disorders. Eating well, exercising, and staying away from harmful substances like tobacco and too much alcohol are important. These actions help keep your blood system healthy.
Regular Screening
Regular health checks are essential for catching blood disorders early. Routine blood tests can spot problems before symptoms show up. We suggest regular check-ups as part of a good prevention plan.
Genetic counseling, healthy living, and regular screenings are key to preventing blood disorders. This approach helps people take charge of their health. It’s a way to be proactive about your well-being.
Conclusion
We’ve looked at many blood disorders like anemia, leukemia, and hemophilia. It’s key to know about these to manage and treat them well.
Diagnosing these conditions is crucial. Blood tests and advanced methods help find the right treatment.
Treatment often includes medicines, blood transfusions, and stem cell transplants. New treatments give hope to patients.
Living with a blood disorder means finding ways to cope and adapting your lifestyle. Prevention and risk reduction are also important.
In short, blood disorders need a lot of care. Knowing about them helps us work towards a healthier future for those affected.
FAQ
What are blood disorders?
Blood disorders affect the blood and its parts, like red and white blood cells, platelets, and plasma. They can change how blood cells are made, work, or last. This can lead to health problems.
What are the common types of anemia?
Anemia types include iron deficiency, vitamin deficiency, anemia of chronic disease, and sickle cell anemia. Each has its own cause and treatment.
What is leukemia, and how is it treated?
Leukemia is cancer that affects blood and bone marrow. It causes abnormal white blood cells. Treatment includes chemotherapy, targeted therapy, or stem cell transplant, based on the disease’s type and stage.
What is hemophilia, and how is it managed?
Hemophilia is a genetic disorder that makes blood hard to clot. It leads to too much bleeding. Treatment involves replacing clotting factors and taking steps to prevent bleeding.
What is sickle cell disease, and what are its complications?
Sickle cell disease is a genetic disorder that makes red blood cells break down early. It can cause anemia, infections, stroke, and organ damage.
How is thrombocytopenia treated?
Thrombocytopenia, or low platelet count, treatment varies by cause. It might include medicines to boost platelet production, transfusions, or treating the underlying issue.
What is polycythemia, and how is it managed?
Polycythemia means having too many red blood cells. It raises the risk of blood clots. Treatment includes phlebotomy to lower red blood cell count and medicines to manage symptoms.
What are the differences between Hodgkin and non-Hodgkin lymphoma?
Hodgkin lymphoma has Reed-Sternberg cells, while non-Hodgkin lymphoma does not. Treatment and outlook differ between the two.
What are the treatment options for blood disorders?
Treatments vary by disorder and include medicines, transfusions, stem cell transplants, and new treatments like gene therapy.
How can I cope with the psychological impact of living with a blood disorder?
Coping with a blood disorder’s mental effects involves seeking support, adapting your lifestyle, and managing symptoms. Healthcare professionals, support groups, and loved ones can help.
Can blood disorders be prevented?
Some blood disorders are genetic or unavoidable. But, preventive steps like genetic counseling, lifestyle changes, and screenings can reduce risk.
What is the importance of regular screening for blood disorders?
Regular screening can catch blood disorders early. This allows for timely treatment, improving outcomes and quality of life.