Last Updated on November 17, 2025 by Ugurkan Demir

It’s important to know about bone marrow disorders for our health. Bone marrow makes healthy blood cells. Any problems here can cause serious issues.
Leukemia, multiple myeloma, and myelodysplastic syndromes are serious bone marrow conditions. They affect thousands each year. These conditions make it hard for the body to fight off infections and heal.
At LivHospital, we focus on top-notch care for bone marrow abnormalities. Our team works hard to help those with these conditions. We offer a patient-focused approach and trusted global expertise.
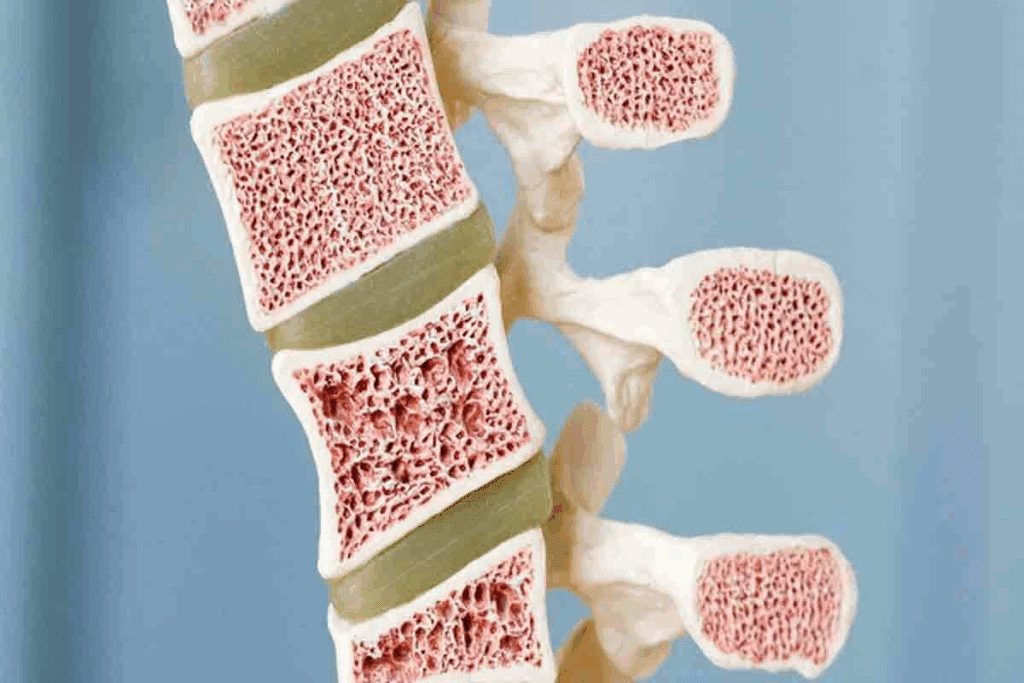
Bone marrow is key to making blood cells, which is vital for our health. It’s the soft tissue inside bones like hips and thighbones. It makes red blood cells, white blood cells, and platelets.
This process is essential for carrying oxygen, fighting infections, and clotting blood.
Bone marrow is a soft, fatty tissue in our bones. It’s a vital organ that makes blood cells through hematopoiesis. There are two types: red marrow for blood cells and yellow marrow for fat and energy.
As we age, some red marrow turns into yellow. But we always have enough red marrow to make the blood cells we need.
Healthy bone marrow makes blood cells through a regulated process. It starts with hematopoietic stem cells that can become different blood cells. Growth factors and cytokines work together to make the right blood cells.
“The bone marrow is a highly dynamic organ, constantly producing billions of blood cells daily to meet the body’s needs.”
Bone marrow makes three main blood cells: red blood cells, white blood cells, and platelets. Red blood cells carry oxygen. White blood cells fight infections. Platelets help blood clot, stopping bleeding when we’re hurt.
Understanding bone marrow’s role in blood cell production shows its importance for our health. Any problem in this process can cause blood disorders.
It’s important to know about blood marrow diseases to catch them early. These diseases affect how the bone marrow makes blood cells. They can cause serious health problems.
Symptoms of blood marrow diseases vary. You might feel fatigue, infections, and bleeding disorders. These signs can mean there’s a problem with your bone marrow.
Some symptoms are more serious. For example, severe anemia, neutropenia, or thrombocytopenia can lead to infections and bleeding. Seeing a doctor quickly is key.
Several things can lead to blood marrow diseases. These include genetic predisposition, exposure to chemicals, and radiation therapy. Viral infections can also raise the risk.
| Risk Factor | Description |
| Genetic Predisposition | Family history of blood marrow diseases |
| Chemical Exposure | Exposure to chemicals like benzene |
| Radiation Therapy | Previous radiation therapy, even at low doses |
Bone marrow disorders can harm your health a lot. They can cause many problems, from mild to severe. For example, anemia can make you weak, and thrombocytopenia can make bleeding more likely.
These conditions can affect not just the person but their family too. Spotting symptoms and risk factors early is key. Working with doctors can help improve life for those with blood marrow diseases.
Acute leukemia is a serious blood cancer that grows fast. It affects the blood and bone marrow, causing too many bad white blood cells. This makes it hard to make normal blood cells. Because it’s aggressive, it needs quick treatment to prevent serious problems.
AML starts in the myeloid cells, which make blood cells. It grows fast, filling the bone marrow with bad cells. This can make you tired, short of breath, and more likely to get infections or bleed.
ALL affects the lymphoid cells and is more common in kids. It makes too many immature white blood cells, taking over the bone marrow. Symptoms include fever, anemia, and bone pain.
AML and ALL treatments often include chemotherapy and targeted therapy. Sometimes, a bone marrow transplant is needed. The right treatment depends on the leukemia type, the patient’s health, and other factors.
Thanks to better treatments, survival rates have gone up. For AML, the 5-year survival rate is about 40%. But it can vary a lot based on age and other things. For ALL, kids have a 68% 5-year survival rate, while adults have around 30-40%.
| Type of Leukemia | Typical Age Group | 5-Year Survival Rate | Common Treatment Approaches |
| AML | Adults (median age 68) | ~40% | Chemotherapy, Targeted Therapy, Bone Marrow Transplant |
| ALL | Children (peak age 2-5) | ~68% (children), ~30-40% (adults) | Chemotherapy, Targeted Therapy |
Knowing about AML and ALL, including treatments and survival chances, helps patients and families deal with these tough diseases.
Chronic leukemias grow slower than acute ones. This allows for different treatments and ways to manage the disease. They are caused by abnormal growth of mature blood cells, leading to health problems if not managed well.
Chronic Myeloid Leukemia (CML) affects white blood cells and grows slowly. It’s often linked to the Philadelphia chromosome, a genetic change from chromosomes 9 and 22.
Targeted therapies, like tyrosine kinase inhibitors (TKIs), have changed CML treatment. These drugs target the molecular defect causing CML, reducing the growth of cancer cells.
Chronic Lymphocytic Leukemia (CLL) mainly affects lymphocytes, a key white blood cell. It’s more common in older adults and can progress at different rates. Some patients may need treatment sooner than others.
CLL treatment varies from watchful waiting to targeted therapies and immunotherapy. The choice depends on the disease stage and genetic markers.
Managing chronic leukemias requires a long-term plan. It focuses on controlling the disease, managing symptoms, and improving quality of life. Regular blood tests and diagnostic tools are key to tracking disease changes.
Patients with chronic leukemias need ongoing care and treatment adjustments. For CML, TKIs might need to be changed due to resistance or intolerance. CLL treatment starts when symptoms appear or the disease progresses. An expert says knowing CLL specifics is vital for the right treatment.
Long-term care also includes managing treatment side effects and improving patient outcomes. A detailed and personalized care plan helps patients with chronic leukemias live better lives.
Understanding multiple myeloma is key for early detection and effective treatment. It’s a cancer that forms in plasma cells, a type of white blood cell. Plasma cells help fight infections by making antibodies.
Multiple myeloma can cause bone damage, anemia, and increase the risk of infections. We will look at the stages, modern treatments, and how to keep patients’ quality of life high.
Multiple myeloma is staged based on myeloma protein levels, anemia, and bone damage. The Revised International Staging System (R-ISS) is used. It looks at albumin levels, beta-2 microglobulin, and chromosomal abnormalities.
The stages help determine prognosis and guide treatment. There are three stages:
| Stage | Characteristics | Prognosis |
| I | Low beta-2 microglobulin, high albumin | Generally better |
| II | Intermediate values | Intermediate |
| III | High beta-2 microglobulin | Generally poorer |
Treatment for multiple myeloma has improved a lot. New treatments offer hope to patients. These include:
Managing multiple myeloma is not just about treating the disease. It’s also about keeping the patient’s quality of life good. This includes managing symptoms, preventing complications, and providing supportive care.
Supportive care includes:
By focusing on both the disease and the patient’s well-being, we can improve outcomes. This enhances the quality of life for those with multiple myeloma.
MDS stands for myelodysplastic syndromes, a group of bone marrow disorders. They cause the bone marrow to not make enough healthy blood cells. This can lead to anemia, infections, and bleeding problems.
MDS is divided into types based on the bone marrow and blood cells. The World Health Organization (WHO) system is the most used. It looks at the number of blasts, genetic changes, and affected cell lines.
The main types of MDS include:
MDS can turn into acute myeloid leukemia (AML). The risk depends on the MDS type and genetic mutations. Higher-risk MDS is more likely to turn into AML.
The International Prognostic Scoring System (IPSS) helps predict AML risk. It looks at blasts, karyotype, and cytopenias.
Treatment for MDS depends on the patient’s risk level. Lower-risk patients focus on symptom management and improving life quality. This might include:
Higher-risk patients aim to prevent AML progression. Treatment options include:
Managing MDS needs a detailed plan. We consider the patient’s risk, health, and needs. Tailored treatment improves outcomes and quality of life for MDS patients.
Myeloproliferative neoplasms are blood cancers where the bone marrow makes too many blood cells. This can cause problems like blood clots, bleeding, or a big spleen.
There are three main types: Polycythemia Vera, Essential Thrombocythemia, and Primary Myelofibrosis. Each has its own signs and health effects.
Polycythemia Vera makes too many red blood cells. This makes blood thick and raises the risk of blood clots. Symptoms include headaches, dizziness, and itching after bathing.
Treatment involves removing blood to lower red cell count and medicines to prevent clots.
In Essential Thrombocythemia, the bone marrow makes too many platelets. This can cause blood clots or bleeding. Symptoms are headaches, dizziness, or numbness in hands and feet.
Doctors use medicines to lower platelet count and stop clots.
Primary Myelofibrosis scars the bone marrow, making blood cell production poor. This can lead to anemia, a big spleen, and other issues. Treatment may include medicines for symptoms, and sometimes bone marrow transplant.
Knowing about these diseases helps us find better treatments. We keep working to improve life for those affected.
Bone marrow failure syndromes are serious conditions where the bone marrow can’t make enough blood cells. This can cause severe health problems like anemia, infections, and bleeding disorders.
Aplastic anemia is when the bone marrow can’t make blood cells. This includes red blood cells, white blood cells, and platelets. It can happen due to toxins, certain medicines, or viral infections. Symptoms include feeling very tired, getting sick easily, and bruising easily.
We find out if someone has aplastic anemia through blood tests and a bone marrow biopsy. Treatment depends on how bad it is and what caused it. It can range from medicines to help the immune system to getting a new bone marrow.
PNH is a rare and serious blood disease. It causes red blood cells to break down, the bone marrow to fail, and can lead to blood clots. It’s caused by a gene mutation.
Symptoms of PNH include dark urine, feeling very tired, and shortness of breath. We treat PNH to stop the breakdown of red blood cells and prevent blood clots.
Pure red cell aplasia is when the bone marrow can’t make red blood cells. It can be caused by autoimmune disorders, certain medicines, or viral infections. The main symptom is severe anemia.
We treat pure red cell aplasia based on what caused it. This can include medicines to suppress the immune system or, in some cases, getting a new bone marrow.
The following table summarizes key aspects of the bone marrow failure syndromes discussed:
| Condition | Primary Characteristics | Common Symptoms | Treatment Approaches |
| Aplastic Anemia | Failure to produce all blood cells | Fatigue, infections, bruising | Immunosuppressive therapy, bone marrow transplantation |
| PNH | Destruction of red blood cells, bone marrow failure | Dark urine, fatigue, shortness of breath | Treatments to reduce hemolysis, prevent thrombosis |
| Pure Red Cell Aplasia | Failure to produce red blood cells | Severe anemia | Immunosuppression, bone marrow transplantation |
It’s important to understand bone marrow failure syndromes to provide the right care. Early diagnosis and the right treatment can greatly improve a person’s life.
Inherited bone marrow disorders are rare conditions that affect blood cell production. They are caused by genetic mutations. These mutations can harm the bone marrow’s ability to make healthy blood cells.
Fanconi anemia is a rare genetic disorder. It causes bone marrow failure, birth defects, and a higher risk of cancer. It is caused by mutations in genes that are key for DNA repair. People with Fanconi anemia often have aplastic anemia. This can lead to leukemia or other cancers if not treated.
Diamond-Blackfan anemia affects red blood cell production. It is characterized by a failure of the bone marrow to produce enough red blood cells, leading to anemia. This condition is often found in infants or young children. It may also be linked to physical anomalies.
Shwachman-Diamond syndrome is a rare genetic disorder. It affects the bone marrow, pancreas, and other organs. It is marked by exocrine pancreatic insufficiency and bone marrow dysfunction. People with this syndrome face risks of infections and blood cancers.
Dyskeratosis congenita is a condition linked to bone marrow failure. It is known for a classic triad of symptoms: oral leukoplakia, nail dystrophy, and skin hyperpigmentation. It is caused by mutations in genes involved in telomere maintenance. This condition shows how genetics and bone marrow function are connected.
Getting a correct diagnosis for bone marrow issues is key for good treatment and care. We use many tests to find and understand these problems.
The first step is often a Complete Blood Count (CBC) and Peripheral Blood Smear. A CBC shows the blood’s different parts, like red and white cells and platelets. The Peripheral Blood Smear looks closely at these cells’ shapes, spotting any oddities.
These tests help find issues like anemia, infections, and leukemia. For example, a CBC can spot odd blood cell counts. A Peripheral Blood Smear can find abnormal or young cells.
Bone Marrow Aspiration and Biopsy are key for diagnosing bone marrow problems. Aspiration takes a bone marrow liquid sample. Biopsy removes a small bone marrow tissue piece. These are then checked for cell production and structure issues.
These steps give important info on the bone marrow’s cells. They help diagnose leukemia, lymphoma, and myelodysplastic syndromes.
| Diagnostic Test | Purpose | Information Provided |
| Complete Blood Count (CBC) | Evaluate blood cell counts | Red and white blood cell counts, platelet count |
| Peripheral Blood Smear | Examine blood cell morphology | Presence of abnormal or immature cells |
| Bone Marrow Aspiration | Analyze bone marrow cells | Cellular composition and abnormalities |
| Bone Marrow Biopsy | Examine bone marrow tissue structure | Architecture and cellular abnormalities |
Cytogenetic and molecular tests look at bone marrow cell genetics. They find chromosomal and genetic mutations linked to bone marrow disorders.
Cytogenetic testing checks bone marrow cell chromosomes. Molecular tests, like PCR and FISH, find specific genetic changes.
Imaging like X-rays, CT scans, MRI, and PET scans also help. They show the disease’s spread and any complications. These images help doctors see the bone marrow and nearby tissues, aiding in diagnosis and treatment plans.
Medical science has made big strides in treating blood marrow diseases. This brings new hope to those affected. We’ve looked at different conditions like leukemias, multiple myeloma, and myelodysplastic syndromes. We’ve talked about their symptoms, risk factors, and how to treat them.
Understanding these diseases better has led to new treatments. Now, many patients with blood marrow diseases have better options. These treatments can make their lives better and increase their chances of survival.
We’re excited about the future for patients with blood marrow diseases. We’re committed to keeping them updated on the latest treatments and support. With ongoing research, we’re hopeful for a brighter future for those affected by these conditions.
Bone marrow disorders affect the bone marrow’s ability to make healthy blood cells. This can cause anemia, infections, and bleeding problems.
Bone marrow disease includes cancers like leukemia and myeloproliferative neoplasms. These diseases disrupt blood cell production.
Symptoms vary but often include fatigue, weight loss, and frequent infections. You might also bleed or bruise easily. Some diseases cause bone pain or swollen lymph nodes.
Tests like complete blood count and bone marrow biopsy are used. Cytogenetic and molecular testing also help identify genetic issues.
Acute leukemia grows fast and needs quick treatment. Chronic leukemia grows slower and may not need immediate treatment but needs ongoing care.
Multiple myeloma is a cancer that affects plasma cells in the bone marrow. It leads to an overproduction of abnormal plasma cells, causing bone damage, anemia, and infections.
MDS is a group of disorders with poorly formed blood cells. It often causes anemia and can lead to acute leukemia.
Myeloproliferative neoplasms are diseases where the body makes too many blood cells. This can cause blood clots and other complications.
Bone marrow failure means the marrow can’t make enough blood cells. This can lead to conditions like aplastic anemia, where no blood cells are made.
Some disorders, like Fanconi anemia, are inherited. Others are caused by toxins or infections.
Treatment varies by disease. It can include watchful waiting, chemotherapy, targeted therapy, or bone marrow transplantation.
Cure chances depend on the disease and its stage. Some, like certain leukemias, can be cured. Others need ongoing care.
Ongoing care helps manage symptoms and monitor disease. It ensures the best quality of life and outcomes.
Risk factors include genetic predisposition, exposure to chemicals or radiation, infections, and previous treatments like chemotherapy.
These disorders can severely impact health by affecting blood cell production. This can lead to anemia, infections, and bleeding complications, reducing quality of life.
References
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!