Why Cancer Patients Need Blood Transfusions
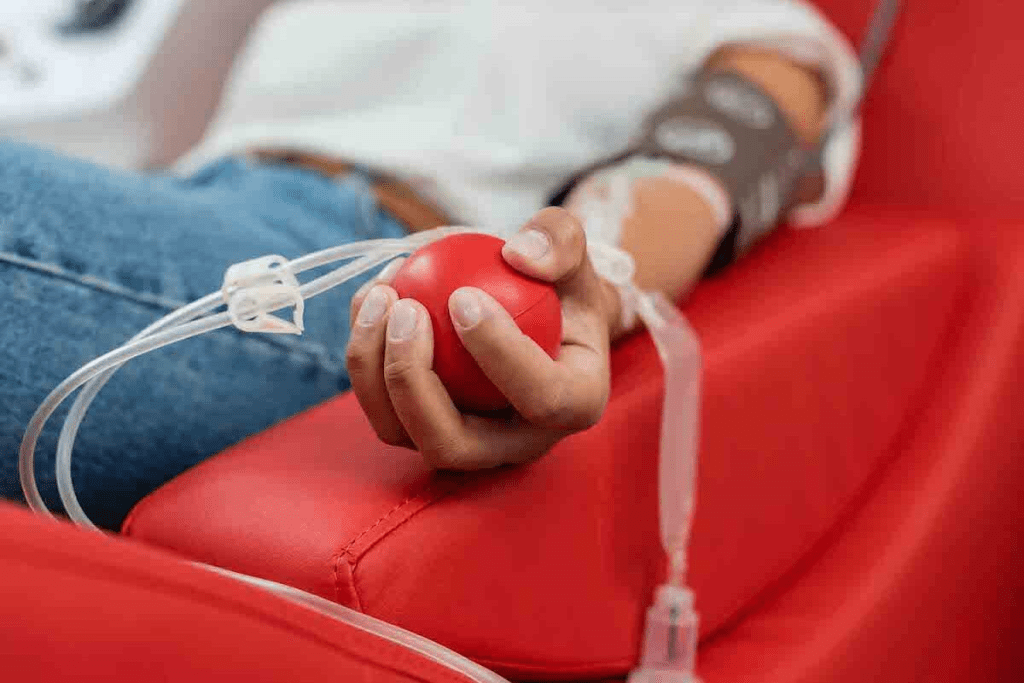
Cancer and its treatments can significantly affect the body’s ability to produce healthy blood cells. This makes transfusions a vital part of modern oncology care. To understand why cancers require blood transfusions, it is important to explore blood therapy for cancer and the medical reasons behind it. Many patients experience anemia, low platelets, or weakened immunity as a direct result of their illness or the treatments used to fight it.
Cancer patients often face anemia or dangerously low platelet counts because their bone marrow is suppressed by the disease or by chemotherapy. According to the American Cancer Society, a large number of cancer treatments lead to the need for transfusions, and up to 50 percent of advanced cancer patients require them to manage severe anemia. In these situations, blood therapy for cancer becomes essential, helping stabilize patients, improve energy levels, reduce complications, and support their ability to continue treatment safely.

Key Takeaways
- Cancer treatments can cause anemia or thrombocytopenia, requiring transfusions.
- The cancer itself may necessitate a transfusion due to its impact on blood cell production.
- Transfusions help manage treatment side effects and support patient care.
- Packed Red Blood Cells are given for decreased hemoglobin levels.
- Platelet transfusions are given for low platelet count or bleeding.
Understanding Blood Transfusions in Cancer Care
Blood transfusions play a key role in cancer care, helping patients manage both the disease and the side effects of treatment. As an important part of blood therapy for cancer, transfusions stabilize blood counts, improve energy levels, and support the body during intensive treatments. Understanding how blood therapy for cancer works is essential for both patients and healthcare providers, ensuring safer care and better overall outcomes.
How Cancer Affects Blood Production
Cancer can seriously affect the body’s ability to produce healthy blood cells. Blood cancers such as leukemia often damage the bone marrow, reducing the body’s ability to make red cells, white cells, and platelets. This drop in blood components makes transfusions necessary as part of blood therapy for cancer to stabilize the patient and support vital functions. In many cases, blood therapy for cancer becomes essential to help patients manage symptoms, prevent complications, and continue receiving life saving treatments.
Types of Blood Components Used in Transfusions
Blood transfusions include red blood cells, platelets, and plasma. The American Red Cross explains how these help patients. For example, red blood cells treat anemia, and platelets prevent bleeding.
When Transfusions Become Necessary
Why would someone need a blood transfusion? It becomes necessary when blood cell counts fall too low, which can happen due to cancer itself or the effects of treatment. Signs such as fatigue, shortness of breath, and easy bruising often indicate the need for support.
In many cases, transfusions are part of blood therapy for cancer, helping restore healthy blood levels and improve overall stability. Getting a transfusion is usually a simple process that can often be done outside the hospital, and discussing these needs with a doctor ensures that blood therapy for cancer is used safely and effectively.
Blood Cancers and Transfusion Requirements
Blood cancers such as leukemia and lymphoma often lead to a strong need for blood transfusions because these diseases damage the bone marrow, the place where blood cells are produced. When the bone marrow cannot function properly, patients experience serious drops in red cells, white cells, and platelets, leading to complications that require transfusions as part of blood therapy for cancer.
The National Cancer Institute explains that many cancer patients rely on growth factors to help manage anemia, yet blood cancers frequently overwhelm the bone marrow to the point where transfusions become essential. This demonstrates how critical blood therapy for cancer is in supporting patients with these conditions and helping them continue their treatment safely.
Leukemia and Its Impact on Blood Production
Leukemia is a blood cancer that makes too many bad white blood cells in the bone marrow. This can lower the number of good blood cells. Patients with leukemia often get blood transfusions to fight anemia, stop bleeding, and boost their immune system.
Leukemia patients need blood transfusions for several reasons:
- Red blood cell transfusions to fight anemia.
- Platelet transfusions to stop bleeding.
- Granulocyte transfusions to fight severe infections.
Myelodysplastic Syndromes (MDS)
Myelodysplastic syndromes (MDS) are disorders that make blood cells not work right. They often cause anemia and other problems. Patients with MDS need blood transfusions to manage their condition, improve their lives, and avoid complications.
Transfusions in MDS patients help in several ways:
- They increase red blood cell count and fight anemia.
- They support platelet counts to prevent bleeding.
- They improve overall health and well-being.
Lymphomas Requiring Blood Support
Lymphomas are cancers of the lymphatic system. They can affect blood cell production. Not all lymphomas affect blood production, but some types and treatments might need blood transfusions.
Patients with lymphoma may need transfusions for:
- Chemotherapy-induced myelosuppression.
- Disease-related bone marrow involvement.
- Splenomegaly causes sequestration of blood cells.
Multiple Myeloma
Multiple myeloma is a cancer of plasma cells in the bone marrow. It can cause anemia, bone pain, and more infections. Blood transfusions are key in managing anemia and improving life for patients with multiple myeloma.
Managing multiple myeloma often includes:
- Red blood cell transfusions to correct anemia.
- Supportive care to reduce treatment side effects.
- Monitoring for complications that may need transfusions.
In conclusion, blood cancers greatly affect blood cell production, often requiring blood transfusions. Understanding the specific needs of patients with different blood cancers is vital for the best care.
Gastrointestinal Cancers Needing Blood Support
Blood transfusions are key in treating gastrointestinal cancers because these cancers, including colorectal, stomach, esophageal, and pancreatic types, can cause significant blood loss. This blood loss often leads to anemia, making transfusions an essential part of blood therapy for cancer to stabilize patients and support their recovery. In many cases, blood therapy for cancer helps maintain strength, reduce symptoms, and ensure patients can continue receiving the treatments they need.
Colorectal Cancer
Colorectal cancer affects the colon or rectum. It’s a common type of cancer. Treatments like surgery and chemotherapy can cause blood loss and anemia. An expert says blood transfusions help by adding back blood components.
Stomach and Esophageal Cancers
Cancers in the stomach and esophagus can bleed a lot. This is because of where the tumors are and the treatments used. Blood transfusions help manage anemia and keep patients healthy during treatment.
Pancreatic Cancer
Pancreatic cancer also needs blood support. It and its treatments can cause bleeding and anemia. Blood transfusions are important for patient care.
Bleeding Complications in GI Cancers
Bleeding is a major concern in gastrointestinal cancers, and it can occur either from the tumor itself or as a side effect of treatment. Blood transfusions play an important role in managing this bleeding and keeping patients stable enough to continue therapy. As part of blood therapy for cancer, transfusions help restore lost blood volume and support overall safety during treatment.
Why do people need a blood transfusion in these cases? Gastrointestinal cancers often interfere with blood production and cause significant anemia. Transfusions help reduce fatigue, improve strength, and enhance quality of life throughout the treatment process. This connection highlights why blood therapy for cancer is essential for patients facing these conditions, ensuring they receive comprehensive care that supports both their cancer treatment and their overall well being.
Gynecologic Cancers and Transfusion Needs
Treatment for gynecologic cancers often includes blood transfusions to manage significant blood loss. Cancers such as ovarian, cervical, and uterine can lead to heavy bleeding either from the tumor itself or during treatment. In these situations, transfusions become an important part of blood therapy for cancer, helping stabilize patients and maintain safe blood levels.
Understanding how these cancers affect the body highlights why blood therapy for cancer plays such a crucial role in supporting treatment. By restoring lost blood and improving overall strength, transfusions help patients continue their therapy with better stability and improved quality of life.
Ovarian Cancer
Ovarian cancer can cause significant blood loss, especially during surgery, making blood transfusions an important part of care. Transfusions help maintain healthy hemoglobin levels and ensure vital tissues receive enough oxygen during recovery. As a key component of blood therapy for cancer, red blood cell transfusions can reduce fatigue and improve overall strength.
Research shows that transfusions play an important role in improving quality of life for patients with ovarian cancer. By supporting oxygen delivery and stabilizing blood counts, blood therapy for cancer helps patients tolerate treatment better and maintain a higher level of daily functioning.
Cervical Cancer
Cervical cancer treatment, which can include surgery, chemotherapy, and radiation, often causes anemia. Anemia management through blood transfusions is key to preventing fatigue and improving quality of life. It also helps patients tolerate ongoing treatment better.
Uterine Cancer
Advanced uterine cancer can cause a lot of bleeding. Blood transfusions help manage this blood loss, keeping red blood cell counts up. Effective blood loss management is essential to prevent complications and support overall health during treatment.
Managing Blood Loss During Treatment
Managing blood loss is a key part of caring for patients with gynecologic cancers. Blood transfusions are used carefully to manage anemia and prevent complications, serving as an important component of blood therapy for cancer. Understanding the transfusion needs of these patients allows clinicians to provide more effective support, improving outcomes and maintaining quality of life.
Patients with gynecologic cancers may require transfusions for several reasons, including surgical blood loss, anemia caused by chemotherapy, or the effects of radiation therapy. By addressing these needs through well planned blood therapy for cancer, healthcare teams help patients tolerate treatment more comfortably and maintain better overall health throughout their cancer journey.
Blood Therapy for Cancer: Breast and Lung Malignancies
Blood therapy for cancer (Blood transfusions) plays a vital role in managing breast and lung cancers, especially during chemotherapy. These cancers are common and need a full treatment plan. Blood therapy helps manage side effects from treatment.
Breast Cancer Treatment-Related Anemia
Anemia is a big problem for breast cancer patients, caused by chemotherapy and radiation. Treating anemia is key to a better quality of life and treatment results. It’s important to manage iron deficiency and anemia in cancer patients.
- Monitoring hemoglobin levels regularly
- Administering iron supplements or erythropoiesis-stimulating agents as needed
- Considering blood transfusions when necessary
Small Cell Lung Cancer
Small cell lung cancer (SCLC) is a fast-growing lung cancer that needs strong treatments like chemotherapy and radiation. Blood transfusions help manage anemia and low platelets caused by treatment.
Supportive care, including blood transfusions, is key in handling SCLC treatment side effects. It helps improve patient results.
Non-Small Cell Lung Cancer
Non-small cell lung cancer (NSCLC) is the most common lung cancer. Treatment methods differ, but blood transfusions are vital in supportive care. They are important in advanced cases or during chemotherapy.
Transfusion Protocols During Chemotherapy
Transfusion protocols during chemotherapy aim to manage anemia and low platelets. Guidelines suggest transfusing blood based on the patient’s health and lab results.
- Checking the patient’s hemoglobin and platelet count before each chemotherapy cycle
- Transfusing blood as needed to keep levels safe
- Watching for signs of bleeding or anemia
Genitourinary Cancers Requiring Transfusions
Blood transfusions are key in treating genitourinary cancers like kidney, bladder, and prostate cancer. These cancers can cause anemia and bleeding, making transfusions essential. We’ll look at which cancers need transfusions and how to manage anemia in advanced cases.
Renal Cell Carcinoma
Renal cell carcinoma affects kidney function and can lead to anemia. Advanced cases often need blood transfusions to fight fatigue and shortness of breath. The Association for the Advancement of Blood & Biotherapies stresses the importance of managing anemia for a better quality of life.
Bladder Cancer
Bladder cancer can cause bleeding, requiring blood transfusions. Transfusion therapy replaces lost blood and ensures tissues get enough oxygen. We’ll explore how to manage bleeding in bladder cancer patients further.
Prostate Cancer
Advanced prostate cancer can lead to anemia due to bone metastasis. Blood transfusions are often needed to manage anemia and improve outcomes. Severe anemia and significant blood loss during surgery are common reasons for transfusions in prostate cancer patients.
Managing Anemia in Advanced Disease
Managing anemia is vital for patients with advanced genitourinary cancers. This includes blood transfusions, erythropoiesis-stimulating agents (ESAs), and iron supplements. Why do you need a blood transfusion? Transfusions quickly boost red blood cell count, improve oxygen delivery, and reduce symptoms like fatigue. The decision to transfuse depends on hemoglobin levels, symptoms, and overall health.
Factors That Increase Transfusion Likelihood in Cancer Patients
Cancer patients may need blood transfusions for many reasons. Their treatment and health are key factors. Knowing these reasons is important for good cancer care.
Treatment-Related Factors
Cancer treatments like chemotherapy and radiation can harm blood cell production. Chemotherapy can lower blood cell counts, causing anemia or other issues. This might mean patients need blood transfusions to help.
Radiation therapy, too, can reduce blood cell production. This is more likely if the treatment area has a lot of bone marrow. The dose and area treated affect this risk. So, radiation therapy can also lead to a need for blood transfusions.
Disease-Related Factors
The type and stage of cancer matter a lot. Some cancers, like leukemia, directly harm the blood and bone marrow. This can cause severe anemia or low platelet counts.
Advanced cancer stages also increase the risk of needing a transfusion. This is because the disease affects the body’s blood-making abilities more. Cancers that cause bleeding, like some in the gut, also raise the need for transfusions. Knowing the cancer’s details helps doctors assess transfusion risk.
Patient-Related Factors
Other factors, like the patient’s health and medical history, also matter. Patients with existing blood issues or poor nutrition might need transfusions more often. Age and nutrition status also play a part, with older or malnourished patients being more at risk.
Understanding these factors helps doctors plan better for blood transfusions in cancer patients. By looking at treatment, disease, and patient factors, we can support patients better during their cancer treatment.
Conclusion: The Vital Role of Blood Transfusions in Cancer Care
Blood transfusions play a key role in supporting cancer patients throughout their treatment journey. Every year, about 1.9 million Americans are diagnosed with cancer, and many rely on transfusions as an essential part of blood therapy for cancer. These transfusions help manage anemia, control bleeding, and support patients undergoing intensive treatments.
They are needed across many cancer types, including blood cancers as well as cancers of the stomach, uterus, and lungs. Transfusions help stabilize patients with low blood counts, replace lost blood, and improve energy for those going through chemotherapy. Understanding why a transfusion might be necessary helps patients feel more informed and confident in their care. By improving strength and overall well being, blood therapy for cancer becomes a vital part of modern oncology, enhancing both treatment outcomes and quality of life.
FAQ
Why do cancer patients need blood transfusions?
Cancer patients often face anemia or low platelet counts. This is due to their disease or treatment. Blood transfusions are key to replacing lost or missing blood cells.
What are the signs that you need a blood transfusion?
Signs include fatigue, shortness of breath, dizziness, and pale skin. These are often signs of anemia or low blood cell count.
Why would someone need a blood transfusion?
Blood transfusions are needed when the body can’t make enough blood cells. This can happen due to surgery, injury, or disease. Cancer patients may need them because of chemotherapy, radiation, or the cancer’s impact on blood production.
What types of cancer may require blood transfusions?
Many cancers may need blood transfusions. This includes blood cancers like leukemia and lymphoma. Also, cancers of the gastrointestinal, gynecologic, breast, lung, and genitourinary systems may require them.
How does cancer affect blood production?
Cancer can harm blood production by attacking the bone marrow. It can also cause inflammation that disrupts blood cell production. Treatments like chemotherapy and radiation can damage the bone marrow, leading to anemia or low blood cell counts.
What are the different types of blood components used in transfusions?
Blood transfusions use red blood cells, platelets, and plasma. Red blood cells carry oxygen. Platelets help the blood clot. Plasma contains clotting factors and proteins.
Do blood transfusions shorten your life?
Research shows blood transfusions don’t necessarily shorten life when used correctly. The decision to have one depends on many factors, like the medical condition and overall health.
What factors increase the likelihood of needing a blood transfusion in cancer patients?
Several factors can increase the need for blood transfusions in cancer patients. These include treatment-related factors, the type and stage of cancer, and the patient’s overall health and medical history.
Why do people need blood transfusions during cancer treatment?
People may need blood transfusions during cancer treatment to replace lost or missing blood cells. This helps manage anemia, bleeding complications, and other side effects of treatment.
What is the role of blood transfusions in managing treatment side effects?
Blood transfusions are key in managing treatment side effects. They help with anemia, thrombocytopenia, and bleeding complications. This improves patient outcomes and quality of life.

































