Last Updated on December 2, 2025 by Bilal Hasdemir
Every year, thousands of children get blood transfusions for different health issues. The main reason is severe anemia. This is when the body doesn’t have enough healthy red blood cells to carry enough oxygen. Discussing the unique pediatric conditions (e.g., sickle cell crisis, cancer) that make a Blood transfusion necessary for a child.
Learning your child needs a transfusion can be scary. But, this procedure is a key treatment. It can greatly help children with anemia, trauma, or who are having surgery.
Key Takeaways
- Children may need a blood transfusion due to various medical conditions, including severe anemia, trauma, or surgery.
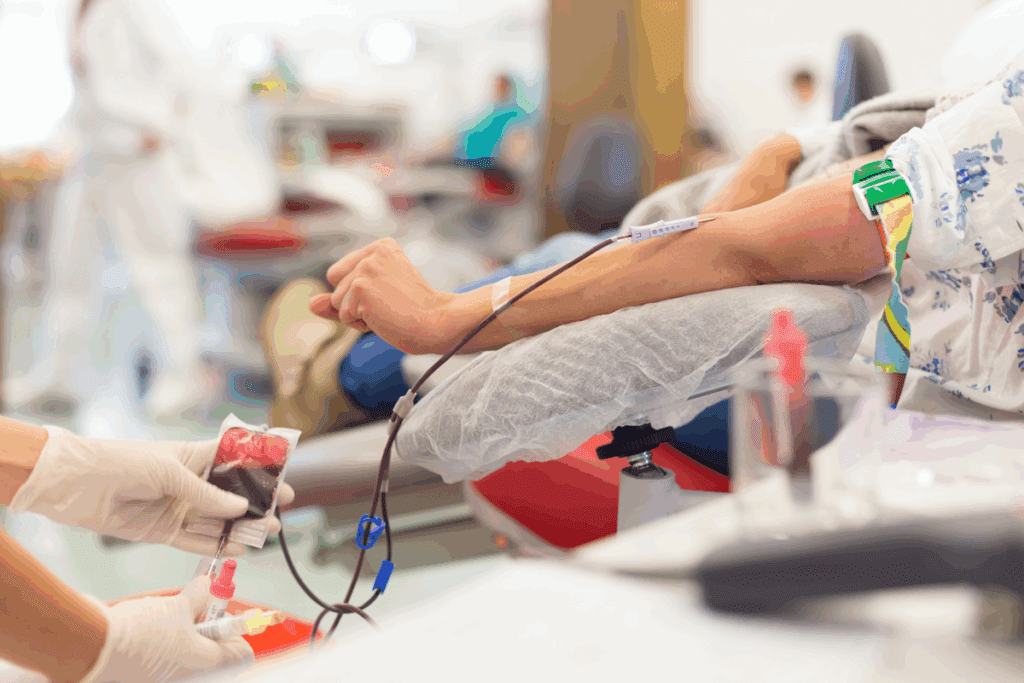
- A blood transfusion involves transferring blood or blood components into a patient’s bloodstream.
- Understanding the reasons for and the process of a transfusion can help alleviate concerns.
- Medical care providers closely monitor children throughout the transfusion process.
- The transfusion process is designed to be safe and effective.
Understanding Blood Transfusion Basics
It’s important for parents and caregivers to know about blood transfusions. A blood transfusion is when blood or blood parts are given to someone. It’s needed for many health issues, like severe anemia and during surgeries.
What is a Blood Transfusion?
A blood transfusion is a life-saving medical intervention. It’s when blood or blood parts are given to someone. This helps get oxygen to the body’s tissues and organs. There are different types of transfusions, like red blood cells or plasma.
The American Red Cross says blood transfusions help in surgeries and treating blood disorders. The versatility of blood transfusions makes them a critical component of healthcare.
How Does Blood Transfusion Work?
The blood transfusion process is careful to ensure safety. First, the patient’s blood type is checked. Then, the blood types are matched to avoid bad reactions.
“The key to a successful blood transfusion lies in ensuring compatibility between the donor’s blood and the recipient’s blood.”
The steps in the blood transfusion process are:
- Blood typing and cross-matching
- Choosing the right blood components
- Checking the blood product before giving it
- Watching the patient during and after
| Blood Component | Purpose | Common Use |
| Red Blood Cells | Improve oxygen delivery | Anemia, Blood Loss |
| Plasma | Replace clotting factors | Bleeding Disorders, Burns |
| Platelets | Prevent or treat bleeding | Low Platelet Count, Surgery |
Knowing about blood transfusions helps parents and caregivers support their kids. We’ll look at why kids might need blood transfusions next.
Reasons Children Might Require a Blood Transfusion

Blood transfusions are vital for kids with serious health issues. We’ll look at why kids need these lifesaving treatments.
Severe Anemia in Children
Anemia is a big problem for kids. It can come from not eating right, chronic illnesses, or genetic issues. Anemia can really lower a child’s quality of life, making them tired, weak, and short of breath. Blood transfusions help by adding more red blood cells, which carry oxygen to important parts of the body.
| Cause of Anemia Description Treatment Approach | ||
| Nutritional Deficiencies | Lack of essential nutrients like iron, vitamin B12, or folate | Dietary adjustments and supplements |
| Chronic Diseases | Ongoing health issues such as chronic infections or inflammatory diseases | Managing the underlying condition |
| Genetic Disorders | Conditions like thalassemia or sickle cell disease affecting hemoglobin production | Blood transfusions and other supportive measures |
Surgery and Procedural Requirements
Kids having surgery or medical procedures might need blood transfusions. The amount of blood lost and the child’s health decide if they need a transfusion.
Some blood disorders, like leukemia or lymphoma, require blood transfusions. These conditions need a lot of care, including transfusions to help manage symptoms and support treatment. Understanding why kids need blood transfusions helps us see how important they are. They save lives and improve health outcomes for children.
Common Conditions Requiring Blood Transfusions
Blood transfusions are key in treating many medical issues in kids around the world. They are essential for treating life-threatening conditions. We will look at common conditions in kids that need blood transfusions.
Sickle Cell Disease
Sickle Cell Disease (SCD) is a genetic disorder that affects hemoglobin production. It causes red blood cells to be abnormally shaped. These cells can get stuck in small blood vessels, leading to pain and serious problems. Blood transfusions help by:
- Reducing sickled red blood cells
- Increasing healthy red blood cells
- Preventing serious complications like stroke
Regular blood transfusions can greatly improve life for kids with SCD. But, it’s important to manage transfusions carefully to avoid risks.
Thalassemia
Thalassemia is a genetic disorder that affects hemoglobin production. It causes severe anemia, leading to health issues if not managed. Blood transfusions are vital in treating thalassemia major, helping to:
- Keep hemoglobin levels healthy
- Support growth and development
- Reduce anemia-related complications
Children with thalassemia often need regular, sometimes lifelong, blood transfusions to manage their condition.
Leukemia and Other Cancers
Leukemia and other cancers can harm the body’s ability to make healthy blood cells. Treatments like chemotherapy can further weaken the bone marrow, making blood transfusions necessary. Blood transfusions help by:
- Replacing lost red blood cells
- Supporting the body during intense treatments
- Improving health and resilience during cancer treatment
For kids with leukemia or other cancers, blood transfusions are a critical part of their care. They help ensure a smooth recovery from treatment.
In conclusion, blood transfusions are lifesaving for kids with serious conditions like sickle cell disease, thalassemia, and leukemia. Understanding these conditions and the role of blood transfusions helps us better support affected children and their families.
The Blood Donation Process
Donating blood is a kind act that helps a lot in healthcare. It gives blood for transfusions. We need donors’ help to keep hospitals supplied with blood for their patients.
Importance of Donating Blood
Donating blood is very important. It helps patients who are having surgery, have blood disorders, or have severe anemia. By giving blood, people can save lives and help the healthcare system.
- Lives Saved: Blood transfusions are key in emergency cases, like accidents or surgeries, to save lives.
- Supporting Medical Treatments: Blood is needed for many medical treatments, including cancer therapy and surgeries.
- Helping Patients with Blood Disorders: Patients with conditions like sickle cell disease or thalassemia need regular blood transfusions.
As a hematologist, says, “Blood donation is a key part of healthcare. Without it, many medical treatments and surgeries wouldn’t be possible.”
How Blood is Collected
The blood collection process is safe and efficient. First, donors are checked to see if they can donate. This includes a health history questionnaire and a physical check-up.
- Donor Screening: Making sure the donor is eligible and the blood is safe for transfusion.
- Blood Collection: Using clean equipment, a needle is put into a vein to collect blood into a bag.
- Testing: The blood is then tested for diseases and typed for compatibility.
Safety Measures for Blood Transfusions
The safety of blood transfusions is a top priority. We test and cross-match blood carefully. This is to prevent bad reactions in children who get transfusions. We make sure the blood is of the highest quality.
Testing Blood for Safety
Blood testing is key to keeping transfusions safe. We test donated blood for diseases like HIV and hepatitis. We also check for bacteria. Advanced screening techniques help find small risks.
The testing process includes:
- Screening for viral infections
- Testing for bacterial contamination
- Checking for other infectious agents
By testing each unit of blood, we lower the risk of disease transmission.
Cross-Matching Blood Types
Cross-matching checks if the donor’s blood matches the recipient’s. This is vital to avoid bad reactions. Precise cross-matching makes sure the blood types and Rh factors are right. This keeps the recipient safe.
The cross-matching process is:
- Determining the blood type and Rh factor of both the donor and the recipient
- Conducting compatibility tests to ensure the donor’s blood is suitable for the recipient
- Verifying the results to confirm compatibility
“The importance of cross-matching cannot be overstated. It is a critical safety measure that prevents potentially life-threatening reactions.” – Transfusion Medicine Specialist
By testing blood thoroughly and cross-matching carefully, we make sure transfusions are safe and work well for children.
The Blood era; Transfusion Procedure
Blood transfusions are complex medical procedures. They require thorough preparation and monitoring. The process involves several critical steps to ensure the safe administration of blood to the patient.
Preparation Before the TransfusionPage 3>
Before a blood transfusion can take place, several preparatory steps must be taken.
- Patient Identification and Blood Typing: Verifying the patient’s identity and determining their blood type are critical to prevent adverse reactions.
- Cross-Matching: The donated blood is cross-matched with the patient’s blood to ensure compatibility.
- Informed Consent: Patients or their guardians must give informed consent after being explained the risks and benefits.
These steps are vital for the success of the transfusion process and patient safety.
Monitoring During the Transfusion
During the transfusion, healthcare professionals closely monitor the patient’s vital signs, including temperature, blood pressure, and heart rate. era p>
- Vital Sign Monitoring: Regular checks help in early detection of any adverse reactions.
- Signs of TRALI or Other Reactions: Healthcare staff are trained to recognize signs of TRALI (Transfusion-Related Acute Lung Injury) or other reactions, allowing for immediate intervention if necessary.
The monitoring continues even after the transfusion is complete, as some reactions may be delayed.
Potential Risks and Side Effects
Blood transfusions save lives but come with risks. It’s key to know the benefits often outweigh these risks, mainly in urgent cases.
Common Reactions to Blood Transfusion
Transfusions can lead to allergic reactions, fever, and chills. These are usually mild and can be handled with medical care.
- Allergic Reactions: These can range from mild to severe and may include symptoms like hives, itching, and difficulty breathing.
- Fever and Chills: These are common reactions that can occur during or after the transfusion.
Health and Well-being
Blood transfusions can greatly affect a child’s health. They help improve oxygen delivery and support recovery from surgery or illness.
It’s important to watch the patient’s health closely during and after the transfusion to manage any adverse effects promptly.
Long-term Outcomes for Children
It’s vital to understand the long-term effects of blood transfusions on children. While they can be lifesaving, there are long-term considerations.
| Condition | Potential Long-term Outcome | Management Strategy |
| Sickle Cell Disease | Regular transfusions can reduce complications but may lead to iron overload. | Monitoring iron levels and chelation therapy. |
| Thalassemia | Frequent transfusions are necessary, with a risk of iron overload. | Regular monitoring and chelation therapy to manage iron levels. |
| Leukemia and Other Cancers | Blood transfusions support treatment but may have varying long-term effects depending on the cancer type and treatment. | Tailored treatment plans and ongoing monitoring. |
Knowing the risks, benefits, and long-term effects helps families and healthcare providers make informed decisions about blood transfusions for children.
Parental Guidance and Support
Supporting your child through a blood transfusion can be tough. We know how important it is to guide and support them during this time.
Empowering Parents with Knowledge
It’s key for parents to understand the blood transfusion process. We suggest asking healthcare providers about the procedure, risks, and benefits. This helps make informed decisions for your child’s care.
Questions to Ask Healthcare Providers
Important questions include: Why is the blood transfusion needed? What are the possible risks and side effects? How will the transfusion be watched? Asking these can ease worries and help your child’s outcome.
Advances in Pediatric Transfusion Medicine
The field of pediatric transfusion medicine is growing fast. New research and innovations aim to improve patient results. Advances in technology and treatments offer hope for kids needing blood transfusions.
By staying informed and teaming up with healthcare providers, parents can offer the best support for their child during the blood transfusion.
FAQ
What is a blood transfusion?
A blood transfusion is when blood or blood parts are given to a patient. This is to replace lost or damaged blood in their body.
Why would a child need a blood transfusion?
Children might need blood transfusions for many reasons. This includes severe anemia, trauma, surgery, or blood disorders like sickle cell disease or leukemia.
What are the different types of blood components that can be transfused?
There are several types of blood components that can be transfused. These include red blood cells, platelets, plasma, and cryoprecipitate.
How is blood tested for safety before transfusion?
Blood is tested for safety by checking for infectious diseases. It’s also tested to make sure it’s compatible with the recipient’s blood type to avoid bad reactions.
What is cross-matching, and why is it important?
Cross-matching is when the donor’s blood type is matched with the recipient’s. This is key to prevent bad reactions. It ensures the blood transfusion is safe.
What are the possible risks and side effects of blood transfusions?
Common side effects of blood transfusions include allergic reactions, fever, and chills. But, rare serious problems can also happen. These include transfusion-related acute lung injury (TRALI) and graft-versus-host disease (GVHD).
How can parents prepare their child for a blood transfusion?
Parents can prepare their child by learning about the transfusion process. They should ask questions to healthcare providers. Also, providing emotional support is very important.
What questions should parents ask healthcare providers about blood transfusions?
Parents should ask about the reasons for the transfusion. They should also ask about the risks and benefits. And, they should ask about the safety measures in place.
What are the long-term outcomes for children who receive blood transfusions?
The long-term outcomes for children vary. It depends on their medical condition and how often they need transfusions. Regular monitoring and follow-up care are key for the best outcomes.
What is the future of blood transfusions in pediatrics?
The future of blood transfusions in pediatrics looks promising. There’s ongoing research and new technologies. These aim to improve patient outcomes in pediatric transfusion medicine.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8107874/