Last Updated on December 2, 2025 by Bilal Hasdemir
Did you know millions of people worldwide have anemia? It’s a condition where they don’t have enough healthy red blood cells. This makes it hard for their body to get enough oxygen. For many, a blood transfusion is a lifesaver that helps ease their symptoms. Everything you need to know about receiving a Blood transfusion for anemia, including guidelines and potential side effects.
We’ll dive into the world of blood transfusions for those with severe anemia. A blood transfusion adds blood to a patient’s blood to boost their red blood cell count. This helps their body get more oxygen to its tissues and organs. This treatment is key for people with anemia caused by chronic diseases, sudden blood loss, or not getting enough nutrients.
Key Takeaways
- A blood transfusion is a critical treatment for severe anemia Page.
- It involves transferring blood into a patient’s bloodstream to increase their red blood cell count.
- Anemia can result from chronic diseases, acute blood loss, or nutritional deficiencies.
- A low hemoglobin transfusion is often necessary for patients with significantly low hemoglobin levels.
- The procedure helps improve oxygen delivery to tissues and organs, alleviating anemia symptoms.
- Page
What is Anemia?
Anemia is when your body has too few red blood cells or they don’t have enough hemoglobin. Hemoglobin is a protein in red blood cells that carries oxygen. This can cause fatigue, weakness, and shortness of breath.
Definition of Anemia
Anemia means your body doesn’t have enough red blood cells. These cells are key for carrying oxygen. Without enough, your body’s tissues and organs don’t get enough oxygen.
Common Causes of Anemia
Many things can cause anemia, including:
- Iron deficiency: Not enough iron means your body can’t make enough hemoglobin.
- Vitamin deficiency: Not enough vitamins like B12 and folate can stop red blood cells from being made.
- Chronic diseases: Long-term illnesses like kidney disease, cancer, and HIV/AIDS can cause anemia.
- Blood loss: Losing blood, whether it’s from an injury, surgery, or heavy periods, can lead to anemia.
Symptoms to Watch For
The signs of anemia can vary. They depend on how bad it is and why it’s happening. Common signs include:
- Fatigue and weakness: Not enough red blood cells or hemoglobin can make you feel tired.
- Shortness of breath: When your body doesn’t get enough oxygen, breathing can be hard.
- Pale skin: Skin looks pale or washed out when there’s not enough hemoglobin.
- Dizziness or lightheadedness: Not enough oxygen to the brain can make you feel dizzy.
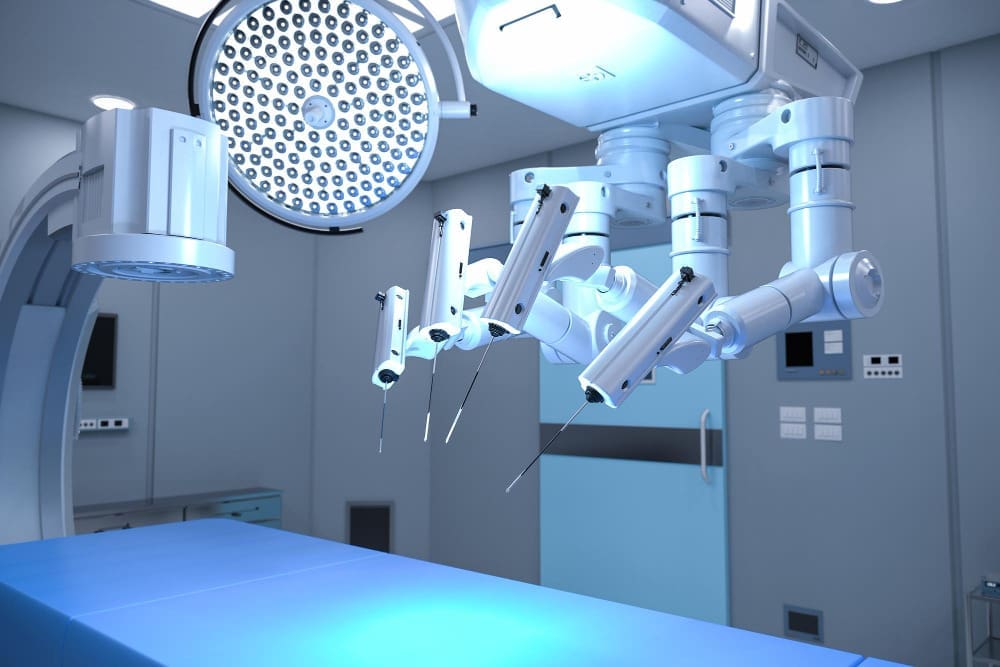
Understanding Blood Transfusion
A blood transfusion is a medical process where blood or blood parts are given to a patient. It’s a key treatment for many health issues, like anemia. It helps increase red blood cells and improves oxygen delivery to the body.
What is a Blood Transfusion?
A blood transfusion is a lifesaving process where blood or blood parts are given to a patient. It’s very important for people with anemia. It helps increase red blood cells and improves oxygen delivery to the body’s tissues. Blood transfusions are very important for people with severe anemia, as they help ease symptoms and support health.
Types of Blood Transfusions
There are many types of blood transfusions, each for different medical needs. The most common types include:
- Red Blood Cell Transfusions: Used to treat anemia by increasing the red blood cell count.
- Platelet Transfusions: Help patients with low platelet counts due to various medical conditions.
- Plasma Transfusions: Used to treat patients with blood clotting disorders or those who have experienced significant blood loss.
| Type of Transfusion | Primary Use |
| Red Blood Cell Transfusion | Treats anemia by increasing red blood cell count |
| Platelet Transfusion | Supports patients with low platelet counts |
| Plasma Transfusion | Treats blood clotting disorders and significant blood loss |
When is a Blood Transfusion Necessary?
A blood transfusion is needed when a patient’s blood count is very low. This can happen due to anemia, surgery, or injury. The decision to have a blood transfusion is made for each patient, based on their health, medical history, and current condition. For anemia patients, a transfusion may be suggested if the condition is severe or if other treatments haven’t worked.
Thinking about a blood transfusion can be scary. But, blood transfusions are common and usually safe. Our medical team is committed to giving personalized care and support during the transfusion. We aim to ensure the best possible results for our patients.
Blood Transfusion for Anemia
For those with severe anemia, blood transfusions can be a lifesaver. Anemia means not enough red blood cells or hemoglobin, making it hard for tissues and organs to get oxygen. This can really hurt someone’s quality of life, making treatment key.
How Blood Transfusions Help
Blood transfusions are a top choice for treating severe anemia. They give red blood cells to boost hemoglobin levels. This helps organs and tissues get the oxygen they need, easing symptoms like tiredness and shortness of breath.
“Blood transfusions can be a game-changer for patients with severe anemia, giving a quick and effective way to restore healthy red blood cell counts,” says a leading hematologist. This is vital for those with chronic anemia who often need regular transfusions.
Benefits of Blood Transfusion for Anemia
Blood transfusions offer many benefits for anemia. They not only raise hemoglobin levels but also help the body carry oxygen better. This can boost energy, reduce shortness of breath, and improve overall health.
- Rapid Improvement: Blood transfusions can quickly improve hemoglobin levels, providing relief from anemia symptoms.
- Enhanced Oxygen Delivery: By increasing red blood cell count, transfusions improve oxygen delivery to vital organs.
- Improved Quality of Life: Patients often experience a significant improvement in their overall condition and quality of life.
Risks and Considerations
While blood transfusions are safe, they come with risks. These include transfusion reactions, infectious disease transmission, and iron overload. It’s vital for healthcare providers to carefully consider these risks and monitor patients closely during and after transfusions.
Every patient’s needs and health status are unique. Healthcare providers must consider these factors to use blood transfusions wisely and effectively in treating anemia.
Alternative Treatments for Anemia
Blood transfusions are key for severe anemia. But, other treatments can also help, depending on the cause. We look at these options to ease anemia symptoms.
Iron Supplements
For iron deficiency anemia, iron supplements are often given. They help increase iron in the body. These can be taken by mouth or given through a vein, based on the severity and health of the patient.
Page
- Oral iron supplements are used for mild to moderate iron deficiency.
- For severe cases or those who can’t take oral iron, intravenous iron therapy is used.
Treating Vitamin Def Pageiciency An Page
When vitamin B12 deficiency causes anemia, vitamin B12 injections are a good solution. This type of anemia often comes from Atrophic gastritis, Crohn’s disease, or certain medicines that block vitamin B12 absorption.
- Vitamin B12 injections help bring vitamin levels back to normal.
- Regular injections may be needed for those with ongoing absorption problems.>
Erythropoiesis-Stimulating Agents
Page>
Erythropoiesis-stimulating agents (ESAs) are another option for anemia, mainly for those with chronic diseases like kidney disease. ESAs boost red blood cell production, cutting down on the need for blood transfusions.
- ESAs are given through injection, usually in a doctor’s office.
- It’s important to keep an eye on dosage to avoid side effects.
These treatments show how important it is to find the cause of anemia. By treating the cause, we can improve health and sometimes avoid blood transfusions.
Medical Conditions Requiring Blood Transfusion
Some health problems, like chronic diseases and injuries, need blood transfusions. These transfusions help manage severe blood loss or anemia. It’s important for both patients and doctors to know about these conditions and how transfusions help.
Chronic Diseases and Anemia
Chronic diseases, such as kidney disease, can cause anemia. This is because the body can’t make enough erythropoietin, a hormone needed for red blood cells. Anemia from chronic diseases makes people feel tired, weak, and short of breath. Blood transfusions are needed to help these symptoms.
Trauma and Acute Anemia
Trauma can cause sudden blood loss and anemia. In these cases, blood transfusions are key. They help replace lost blood, keep blood pressure stable, and ensure organs get enough oxygen.
Cancer and Blood Loss
Cancer treatments, like chemotherapy and radiation, can cause anemia or blood loss. This is because the treatments affect the bone marrow. Blood transfusions are often needed to manage these side effects. They help patients recover from anemia and keep up with their treatments.
era Page tr Page>
| Medical Condition | Reason for Blood Transfusion era> |
| Chronic Kidney Disease Pageоми chair폭 | Anemia due Page Page to reduced erythropoietin production |
| Traumatic Injuries | Acute blood loss leading to severe anemia |
| Cancer Treatments | Anemia or blood loss due to chemotherapy, radiation, or disease Page progression |
Preparing for a Blood Transfusion
Knowing about the blood transfusion process helps patients feel more at ease. We’ll walk you through the steps, so you know what to expect.
Pre-Transfusion Testing
We do pre-transfusion testing to make sure the blood is safe for you. This test checks if the donor’s blood matches yours.
The testing includes:
- Blood typing to find out your blood group
- Screening for antibodies that could react with the donor blood
- Cross-matching to confirm the blood is safe for you
| Test | Purpose |
| Blood Typing | Finds your blood group (A, B, AB, or O) and Rh factor |
| Antibody Screening | Looks for antibodies against blood group antigens |
| Cross-Matching | Checks if the donor blood is safe for you |
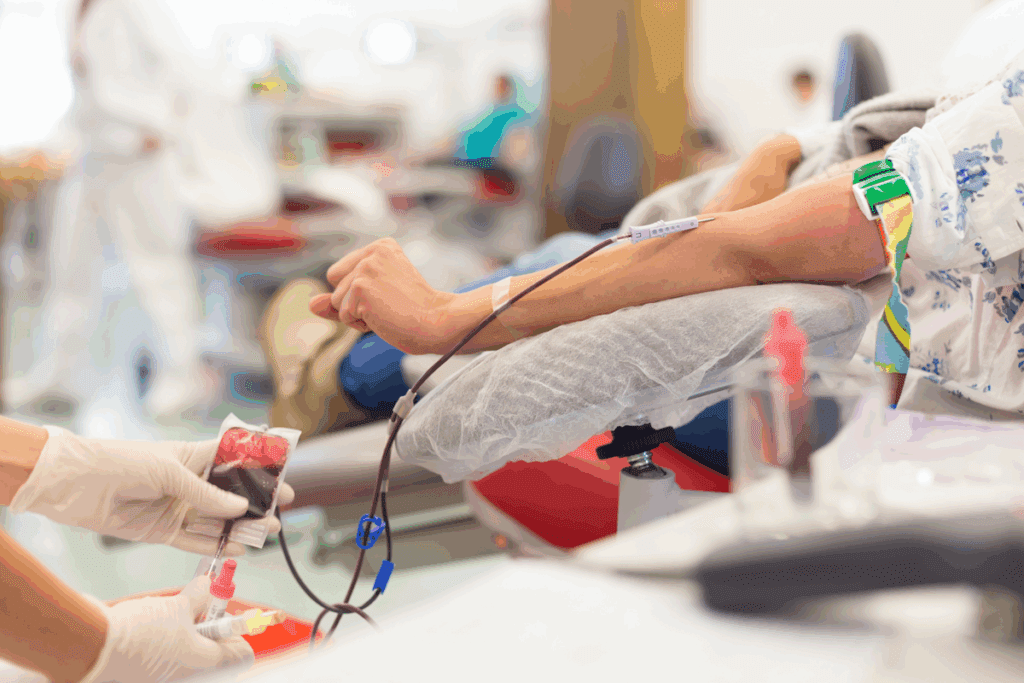
What to Expect During the Procedure
During the transfusion, we watch your vital signs closely. We’re ready to act if there’s a problem.
Here’s what you can expect:
- The transfusion goes through an IV line
- The time it takes depends on how much blood you need
- Our team is always there to check on you and answer any questions
By understanding these steps, you can feel more ready for the blood transfusion. It will make the experience less scary.
Post-Transfusion Care
Post-transfusion care is key to patient safety and recovery. After a blood transfusion, monitoring for complications and knowing the signs of adverse reactions are vital. We stress the need for constant watchfulness to quickly handle any problems.
Monitoring for Complications
Patients are closely watched for signs of adverse reactions after a blood transfusion. Prompt recognition of these signs is essential for quick action. We look out for symptoms like fever, chills, rash, or trouble breathing, and act fast if they show up.
We check vital signs like temperature, blood pressure, and heart rate regularly. We also run lab tests to see how the patient is doing and check for complications.
Signs of Adverse Reactions
It’s important for patients and caregivers to know the signs of adverse reactions. These can include:
- Fever or chills
- Rash or itching
- Difficulty breathing or shortness of breath
- Chest or back pain
- Nausea or vomiting
If any of these symptoms happen, it’s important to tell healthcare providers right away. We aim to offer the support and guidance needed to handle these reactions well.
Knowing about side effects and how to deal with them can help a lot in recovery and safety. We’re committed to giving our patients the best care after a transfusion.
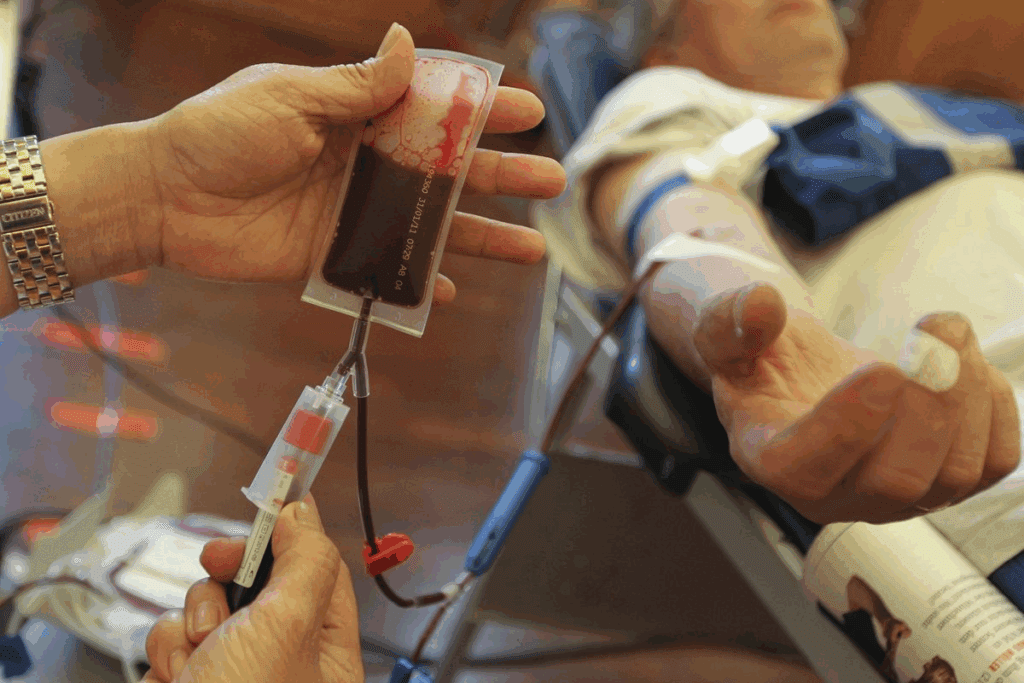
Blood Donation and Transfusion
Blood donation is a voluntary act that saves countless lives. It’s a key part of healthcare systems around the world. It provides the blood needed for surgeries, treatments, or when patients lose blood.
How Blood Donations Work
Blood donation involves several steps. From the initial registration and screening of donors to the collection, testing, and processing of the blood. Here’s a brief overview:
- Donor Registration and Screening: Donors register and go through a screening to check if they can donate.
- Blood Collection: Blood is collected from eligible donors in a clean environment.
- Blood Testing: The blood is tested for diseases and typed to see if it’s safe for transfusion.
- Processing: The blood is broken down into its parts, like red blood cells, plasma, and platelets. These parts can treat different medical conditions.
- Storage and Distribution: The blood parts are stored and sent to hospitals when they’re needed.
The Importance of Donors
Blood donors are the heart of the blood transfusion system. Their donations help hospitals save lives. Their contributions are vital for patient care in many clinical settings.
We need to keep attracting and keeping blood donors. Donors come from all walks of life. They donate because they want to help others. By giving blood, they can change the lives of patients undergoing treatments.
“The gift of blood is a gift to someone’s future.” This shows the big impact donors have on others. As we depend on blood donations, we must thank the donors for their kindness and generosity.
Special Populations and Blood Transfusion
Blood transfusions are key for managing anemia in vulnerable groups like children, pregnant women, and older adults. Each group has special needs that require careful thought when giving blood transfusions.
Considerations for Children
Children need different amounts and types of blood when they get transfusions. We must adjust the dosage and type based on their size and age. This ensures their safety and the success of the transfusion.
- Weight-based calculations: Blood component doses are often calculated based on the child’s weight.
- Age-specific considerations: Premature infants and neonates may require special blood components.
- Monitoring: Close monitoring is critical to avoid complications and ensure the transfusion works well.
Anemia in Pregnant Women
Pregnant women with severe anemia might need blood transfusions to keep them and their baby healthy. Anemia during pregnancy can cause serious problems if not treated right.
When thinking about blood transfusions for pregnant women, we look at several things:
- The severity of anemia and its effects on both mother and fetus.
- Any underlying conditions that might be causing the anemia.
- The stage of pregnancy and how it influences our decisions.
Older Adults Facing Anemia
Older adults might need blood transfusions for anemia caused by chronic diseases, nutritional deficiencies, or other health problems. When dealing with anemia in older adults, we consider their overall health and any other health issues they have.
Important things to think about include:
- Comorbid conditions: Conditions like heart disease or kidney disease can impact transfusion decisions.
- Medication interactions: Older adults often take many medications that could react with blood transfusions.
- Nutritional status: Fixing nutritional deficiencies is key in managing anemia.
By understanding the unique needs of these special populations, we can offer more effective and safe blood transfusion treatments.
Frequently Asked Questions about Blood Transfusions
Patients often have many questions about blood transfusions. They want to know how long it takes, if it’s safe, and what long-term effects it might have. We get it. Blood transfusions can be a big worry, and answering these questions can help ease that worry.
How Long Does a Blood Transfusion Take?
The time it takes for a blood transfusion can vary a lot. It depends on the person’s health and why they need the transfusion. Usually, it takes one to four hours. But, it can be shorter or longer depending on the situation.
For example, if someone has lost a lot of blood, the transfusion might be quicker. On the other hand, for people with certain health issues, the transfusion might be slower to avoid problems.
Is Blood Transfusion Safe?
When it comes to blood transfusions, safety is top priority. We do a lot to make sure they are safe for our patients. This includes testing the blood for diseases and matching it to the patient’s blood type.
Even though there are some risks, like allergic reactions or lung problems, these are rare. Our medical team watches patients closely during and after the transfusion. This way, they can quickly spot and handle any problems.
What are the Long-term Effects?
Most of the time, the long-term effects of blood transfusions are small. This is true when the transfusion is done right. But, like any medical treatment, there are some risks and possible problems.
Some people might get iron overload if they have many transfusions. This can harm organs over time if not treated. Our healthcare team keeps a close eye on patients to prevent or manage these long-term effects.
| FAQ | Key Points |
| Duration of Blood Transfusion | Typically 1-4 hours, varies based on individual condition |
| Safety of Blood Transfusion | Rigorous blood testing and matching; rare complications |
| Long-term Effects | Generally minimal; possible iron overload with frequent transfusions |
Future of Blood Transfusion
The world of blood transfusion is on the verge of a big change. This change comes from innovations in anemia treatment and research on blood alternatives. New treatments and technologies are coming to help patients more and maybe even cut down on the need for blood transfusions.
New therapies are being developed to tackle anemia at its source, not just its symptoms. This new approach is changing how we treat anemia in patients.
Innovations in Anemia Treatment
One exciting area is the creation of erythropoiesis-stimulating agents (ESAs). These agents help make more red blood cells, which might mean fewer blood transfusions for some patients with anemia.
- ESAs have been shown to be effective in treating anemia in patients with chronic kidney disease and cancer.
- Researchers are working to find the best doses and reduce side effects.
Research on Blood Alternatives
There’s also a push to make artificial blood substitutes. These substitutes aim to carry oxygen like red blood cells do. They could offer a safer, more reliable option than traditional blood transfusions.
| Blood Alternative | Description | Potential Benefits |
| Hemoglobin-based oxygen carriers (HBOCs) | Solutions that contain hemoglobin, which can carry oxygen to tissues | Potential to reduce the need for red blood cell transfusions, lower risk of transfusion-related complications |
| Perfluorocarbon-based oxygen carriers (PFCs) | Synthetic compounds that can dissolve and transport oxygen | Potential to provide a reliable and consistent source of oxygen, reduce the need for red blood cell transfusions |
As research keeps moving forward, we can look forward to better treatments for anemia and blood transfusions. The future of blood transfusion looks bright, with a focus on safer, more effective treatments for patients everywhere.
Resources for Patients and Caregivers
Dealing with anemia and blood transfusions can be tough. But, there are many resources to help patients and caregivers. It’s important to have the right information and a supportive community.
Connecting through Support Groups
Support groups are a great way to connect. They let people share their stories and find comfort in knowing they’re not alone. These groups offer emotional support and practical tips.
Many groups focus on anemia, providing a safe place to talk and get advice from others who understand.
Educational Materials and Guidance
It’s key to understand blood transfusions and anemia to manage them well. We offer materials on blood transfusions, anemia signs, and treatment options.
These resources give patients and caregivers the knowledge to make informed care decisions.
Finding Help When Needed
It’s important to know where to find help with anemia and blood transfusions. We help patients find trusted healthcare providers and treatment centers.
Our goal is to positively impact those dealing with anemia by providing these resources.
FAQ
Why do people need blood transfusions?
People need blood transfusions for many reasons. This includes severe anemia, chronic diseases, and blood loss from cancer treatments.
How long does a blood transfusion take?
The time for a blood transfusion varies. It depends on the person’s condition and the type of transfusion. It usually takes from one to four hours.
Is blood transfusion safe?
Blood transfusions are mostly safe. There are strict tests and matching to reduce risks. But, like any medical procedure, there can be risks and complications.
What are the risks Page associated with blood transfusions?
Risks include transfusion reactions, allergic reactions, and infectious diseases. Close monitoring during the transfusion helps reduce these risks.
What are the signs of a blood transfusion reaction Page?
Page style=”margin-bottom:0″>A: Signs include fever, chills, itching, hives, and trouble breathing. If you notice these, tell the medical staff right away.
Can I receive a blood transfusion Page if I have a rare blood type?
Yes, people with rare blood types can get transfusions. Blood banks keep records of rare types to ensure compatibility.
How is blood matched for transfusions?
Blood is matched through testing like blood typing and cross-matching. This ensures the donor’s blood is compatible with the recipient’s.
Page style=”margin-bottom:0″>Q: What is the role of erythropoiesis-stimulating agents in treating anemia?
These agents help make more red blood cells. They are used for anemia caused by chronic diseases, like chronic kidney disease.
Are there alternatives to blood transfusions?
Yes, there are alternatives. These include treatments for the cause of anemia, like iron supplements and vitamin B12 injections. Erythropoiesis-stimulating agents are also used.
How can I prepare for a blood transfusion?
To prepare, you’ll need pre-transfusion testing and understanding the procedure. Follow your healthcare provider’s instructions.
What should I expect during a blood transfusion?
You’ll be closely watched for any signs of a reaction. The transfusion is done in a controlled medical setting.
What is post-transfusion care?
After the transfusion, you’ll be monitored for complications. Be aware of signs of adverse reactions. Follow your healthcare provider’s post-transfusion care instructions.