Last Updated on December 2, 2025 by Bilal Hasdemir

Anemia is a common problem worldwide, causing tiredness, weakness, and shortness of breath. A study in the Journal of Clinical Medicine showed that blood transfusions save lives for those with severe anemia. Knowing how blood transfusions work is key to helping patients.Detailed procedures and clinical guidelines for when a Blood transfusion for anemia is medically necessary and safe to perform.
We will look into when transfusion is needed, the transfusion threshold, and the hemoglobin levels that call for transfusion. This will help us understand the importance of blood transfusion in treating anemia.
Key Takeaways
- Understanding the guidelines for blood transfusion in anemia patients is key to effective treatment.
- The decision to transfuse depends on how severe the anemia is and the patient’s health.
- Hemoglobin levels are important in deciding if a transfusion is needed.
- Transfusion thresholds change based on the situation and the patient’s needs.
- Following proper transfusion procedures is vital to keep patients safe.
What is Anemia and How It Affects the Body?
Anemia is when your body doesn’t have enough red blood cells or hemoglobin. It makes everyday life harder and can harm your health. It’s a big problem that affects many people around the world.
Definition of Anemia
Anemia means your body has too few red blood cells or they don’t carry enough hemoglobin. Hemoglobin is key for carrying oxygen. Without enough, your body’s tissues and organs don’t get enough oxygen. This can cause many health problems.
Common Causes of Anemia
There are many reasons why someone might get anemia. Some include:
- Iron deficiency: This is the top reason for anemia. It can happen if you don’t eat enough iron, lose blood too much, or need more iron when you’re pregnant.
- Vitamin deficiency: Not having enough vitamins like B12 and folate can also cause anemia.
- Chronic diseases: Diseases like chronic kidney disease, cancer, and HIV/AIDS can lead to anemia.
- Blood loss: Losing a lot of blood from surgery, injuries, or heavy periods can also cause anemia.
Symptoms and Health Risks
The symptoms of anemia can be different for everyone. They often include feeling very tired, weak, and pale. You might also have shortness of breath and feel dizzy. If anemia isn’t treated, it can cause serious problems like heart issues and bad pregnancy outcomes. Knowing the hemoglobin level for transfusion is key for treating severe cases. It helps decide if a low hb blood transfusion is needed.
Anemia is a big health issue that needs careful management. By knowing what causes it, its symptoms, and how treatments like blood transfusions work, we can help people get better.
When is Blood Transfusion Recommended?
Anemia treatment often involves blood transfusion. It’s important to know when to do it. The decision is complex and depends on many factors.
Indications for Blood Transfusion in Anemia
Blood transfusion is recommended for severe anemia or significant blood loss. The main reason is a low hemoglobin level. This can cause organs to not get enough oxygen.
Specific reasons include:
- Severe anemia with hemoglobin levels below 7-8 g/dL
- Significant blood loss due to surgery, trauma, or gastrointestinal bleeding
- Symptomatic anemia causing shortness of breath, chest pain, or dizziness
Factors Influencing Transfusion Decisions
Several factors affect the decision to transfuse blood. These include the patient’s health, any underlying conditions, and how well they can handle anemia.
| Factor | Description |
| Hemoglobin Level | The primary indicator for blood transfusion, with lower levels indicating a greater need for transfusion. |
| Symptoms | The presence and severity of symptoms such as fatigue, shortness of breath, and dizziness influence the decision to transfuse. |
| Underlying Conditions | Patients with heart disease, chronic obstructive pulmonary disease (COPD), or other conditions may require earlier transfusion due to their reduced ability to compensate for anemia. |
Risks of Delaying Transfusion
Delaying blood transfusion can lead to serious problems. These include organ failure and even death. Early transfusion helps ensure tissues get enough oxygen.
Risks associated with delayed transfusion include:
- Organ dysfunction due to prolonged hypoxia
- Increased risk of cardiac complications
- Prolonged hospital stay and recovery time
Understanding when to transfuse blood helps healthcare providers make better choices. This improves patient outcomes.
Types of Blood Transfusions for Anemia
Blood transfusions for anemia come in different forms. Each type is designed for specific patient needs. The choice of transfusion can greatly affect patient outcomes, as the American Association of Blood Banks notes.
Whole Blood Transfusions
Whole blood transfusions include all blood components: red blood cells, plasma, and platelets. They are often used when there’s a lot of blood loss, like during surgery or trauma.
Benefits of whole blood transfusions include replacing many blood components at once. This can be lifesaving in emergency situations.
Red Blood Cell Concentrates
Red blood cell (RBC) concentrates mainly contain red blood cells, with most plasma removed. They are used to increase red blood cell count in anemic patients. This improves oxygen delivery to tissues.
- Red blood cell concentrates are the most common treatment for anemia.
- They are great for patients needing more red blood cells without extra plasma or platelets.
Platelet and Plasma Transfusions
Platelet transfusions help prevent or treat bleeding in patients with low platelet counts or dysfunction. Plasma transfusions replace clotting factors and proteins in patients with deficiencies or bleeding disorders.
| Type of Transfusion | Primary Use | Key Components |
| Whole Blood Transfusions | Significant blood loss, trauma, or surgery | Red blood cells, plasma, platelets |
| Red Blood Cell Concentrates | Anemia, increasing red blood cell mass | Red blood cells |
| Platelet Transfusions | Low platelet count, platelet dysfunction | Platelets |
| Plasma Transfusions | Clotting factor deficiencies, bleeding disorders | Plasma |
Understanding the different blood transfusions helps healthcare providers choose the best treatment for anemic patients.
Blood Transfusion Guidelines in the United States
The United States has set up detailed guidelines for blood transfusions. These rules are key to keeping this important medical action safe and effective. They help manage anemia and other conditions that need blood transfusions.
Overview of National Guidelines
National blood transfusion guidelines are made from the latest research and clinical evidence. These guidelines help healthcare providers make smart decisions about blood transfusions. They ensure patients get the best care possible.
These guidelines cover many areas. They include when to transfuse blood, which blood components to use, and how to handle any problems that might arise.
We use these guidelines to make care more consistent and better for patients. By sticking to these protocols, doctors can reduce risks and make blood transfusions more effective for patients with anemia.
Role of the American Association of Blood Banks (AABB)
The AABB is key in creating and sharing blood transfusion guidelines in the United States. Their guidelines are based on deep reviews of clinical data and expert opinions. They offer clear advice on how to handle transfusions.
We value the AABB’s work in making patient care safer and better. Their guidelines are followed by many healthcare places in the country. This ensures patients get top-notch care when they need a transfusion.
Clinical Pathways for Anemia Management
Clinical pathways for managing anemia involve a team effort. Blood transfusion is just one part of the whole care plan. These pathways aim to improve patient results by making sure care is timely and right.
We stress the need for care plans that fit each patient’s unique situation. By combining blood transfusion guidelines with other treatments, doctors can give patients the best care for managing anemia.
Pre-transfusion Preparation and Testing
Healthcare providers do a lot of work before a blood transfusion. They make sure the blood is safe and works well for patients with anemia.
Importance of Crossmatching
Crossmatching is a test to see if the donor’s blood is safe for the patient. It checks if the donor’s red blood cells and the patient’s plasma are compatible. This is key to avoid serious problems like hemolysis.
During crossmatching, the donor’s red cells are mixed with the patient’s serum. This is to see if there are any signs of agglutination or hemolysis.
- Ensures compatibility between donor and recipient blood
- Reduces the risk of hemolytic reactions
- Is a critical step before issuing blood for transfusion
Blood Typing Procedures
Blood typing is important to find out the patient’s blood group. This is vital for safe transfusions. We look at two main blood group systems: ABO and Rh.
Accurate blood typing makes sure the patient gets the right blood. This lowers the chance of a bad reaction.
- Determine the patient’s ABO blood group (A, B, AB, or O)
- Identify the Rh blood type (Rh positive or Rh negative)
- Perform antibody screening to detect any unexpected red blood cell antibodies
Patient Consent and Education
We need the patient’s consent before a blood transfusion. We explain why it’s needed, the risks, and the benefits. Teaching patients is also key. It helps them understand their treatment and watch for any bad reactions.
We make sure patients know what’s happening. They get to ask questions too.
By getting patients ready for blood transfusions, we lower risks. This includes crossmatching, blood typing, and teaching them. It helps improve how well patients do.
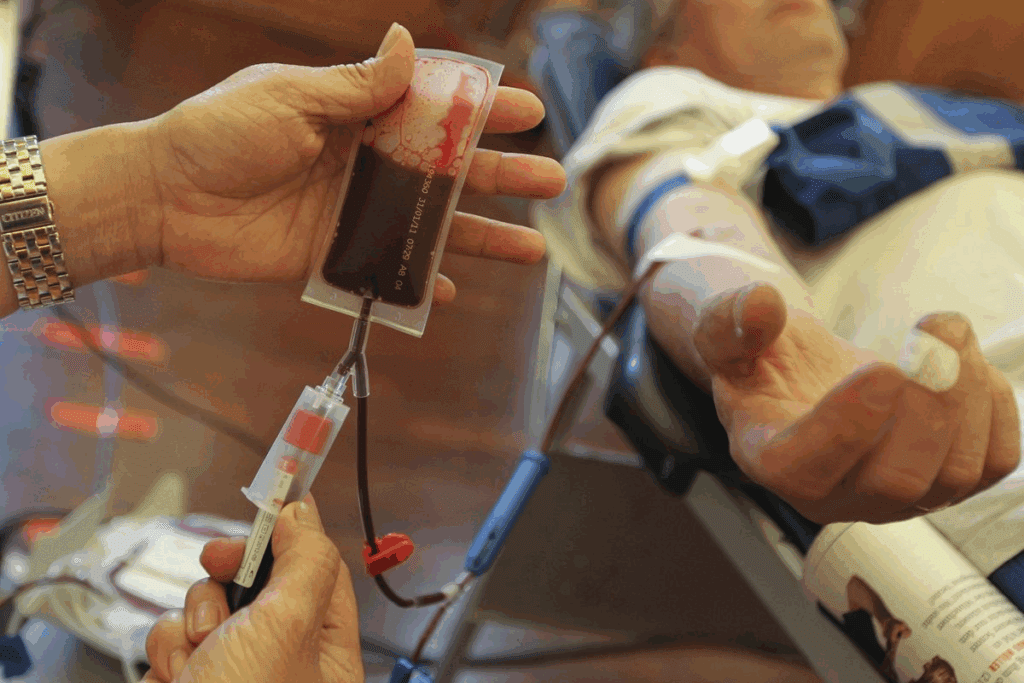
The Blood Transfusion Process
Blood transfusion is a key medical step that requires careful steps. We know it can worry patients. Our aim is to make the process safe and smooth for everyone.
Step-by-Step Procedure
The process starts with careful preparation. We check the patient’s medical history, perform blood tests, and make sure the blood is compatible. After these steps, the transfusion can begin.
The transfusion itself involves several important steps:
- Insertion of an intravenous line to administer the blood product.
- Administration of the blood product at a controlled rate.
- Close monitoring of the patient’s vital signs and overall condition.
Monitoring During Transfusion
During the transfusion, we watch the patient’s vital signs closely, including temperature, blood pressure, and heart rate. This helps us spot any issues quickly and act fast if needed.
The National Heart, Lung, and Blood Institute says it’s key to watch closely during transfusion to catch problems early.
Managing Possible Complications
Even though blood transfusions are usually safe, complications can happen. We know how to quickly spot and handle these issues. Problems like allergic reactions, TRALI, and TACO are common.
If a complication occurs, we act fast to keep the patient safe. This might mean stopping the transfusion, giving medicines, or providing other care as needed.
Post-transfusion Care and Follow-Up
Post-transfusion care is key to a patient’s recovery. It focuses on watching for complications and keeping the patient healthy. After a blood transfusion, patients need close monitoring to make sure they’re doing well.
Symptoms to Watch After Transfusion
Patients and their caregivers should know about possible signs of trouble. These include:
- Fever or chills
- Shortness of breath or trouble breathing
- Rash or itching
- Swelling or pain at the transfusion site
- Dizziness or fainting
If any of these symptoms show up, it’s important to tell the healthcare team right away. A study in the Journal of Patient Safety found that quick action can greatly improve results (8).
Follow-Up Testing and Evaluation
It’s important to do follow-up tests to see how the transfusion worked and how the patient is doing. This might include:
- Complete Blood Count (CBC) to check red blood cell levels
- Blood typing and cross-matching to ensure compatibility
- Monitoring vital signs, such as blood pressure and heart rate
These tests help doctors decide if more transfusions are needed or if other treatments are better. Good follow-up care can really help patients get better and live better lives.
Educating Patients on Self-Care
Teaching patients how to take care of themselves is a big part of post-transfusion care. They should learn about:
- Managing side effects
- Eating a healthy diet full of iron and vitamins
- Not doing too much too soon
- Knowing when to look for signs of trouble
Teaching patients about their care can make them healthier and happier. We make sure to teach patients well as part of our top-notch healthcare.
In short, taking care of patients after a transfusion is very important. By watching for symptoms, doing follow-up tests, and teaching patients about self-care, doctors can help patients get the best results from blood transfusions.
Alternatives to Blood Transfusion for Anemia
Anemia management has evolved a lot. Now, there are many alternatives to blood transfusions. These options are great for those at risk of complications or who don’t want blood transfusions for personal reasons.
First, treating the cause of anemia is key. This might mean changing diets or taking supplements to fix nutritional gaps.
Iron Supplements and Dietary Changes
Iron supplements help with iron-deficiency anemia. Eating iron-rich foods and vitamin C can help your body absorb iron better. A balanced diet with foods like red meat, spinach, and fortified cereals is recommended.
For severe cases, oral iron supplements or intravenous iron therapy might be needed. This depends on how bad the anemia is and how well the patient can take oral iron.
Erythropoietin-Stimulating Agents
Erythropoietin-stimulating agents (ESAs) are another option. These drugs help make more red blood cells. They’re often used for chronic kidney disease or cancer-related anemia.
A study in the Journal of Clinical Oncology shows ESAs work well for cancer patients. They reduce the need for blood transfusions and improve life quality.
Other Medical Interventions
Other treatments depend on the anemia’s cause. For vitamin deficiency anemia, vitamin supplements are needed. Treating the underlying disease helps with chronic disease anemia.
New medications like hypoxia-inducible factor prolyl hydroxylase inhibitors are also used. They’re promising for those not responding to usual treatments or needing extra help.
By exploring these alternatives, doctors can create better treatment plans. This improves patient outcomes and quality of life.
Frequently Asked Questions about Blood Transfusion for Anemia
Patients often wonder about blood transfusion. They ask about its safety, what happens if they refuse, and how long it lasts. We aim to clear up these concerns and offer reassurance.
Safety of Blood Transfusion
Blood transfusion is safe and works well, says the American Association of Blood Banks (AABB). The chance of problems is small. We make sure the blood is safe for everyone.
Refusing a Transfusion
Not getting a blood transfusion can be risky, mainly if anemia is bad. We talk about the risks and benefits with patients. This helps them make the best choice for their health.
Duration of Transfusion
How long a blood transfusion takes varies. It can last from one to four hours. We keep a close eye on patients to make sure they’re comfortable and safe.
FAQ
What is the threshold for blood transfusion in anemia patients?
The need for a blood transfusion in anemia patients depends on their condition. Usually, a hemoglobin level below 7-8 g/dL is when transfusions are considered.
How safe is blood transfusion?
Blood transfusions are safe when done right. This means screening blood well and following guidelines closely.
What happens if I refuse a blood transfusion?
Not getting a blood transfusion can make anemia worse. It can also lead to fatigue and serious health issues. Always talk to your doctor about your concerns.
How long does a blood transfusion take?
How long a blood transfusion lasts depends on the blood type and amount. It usually takes between 1-4 hours.
What are the indications for blood transfusion in anemia?
Doctors usually recommend blood transfusions for severe anemia symptoms. This includes significant blood loss or serious medical conditions.
At what hemoglobin level is a blood transfusion needed?
Deciding on a transfusion depends on the patient. But, a hemoglobin level below 7-8 g/dL is often the threshold.
Can I receive a blood transfusion if I have a low hemoglobin level?
Yes, getting a blood transfusion is common for low hemoglobin. This is true for anemia or significant blood loss.
What are the risks associated with delaying blood transfusion?
Waiting too long for a transfusion can harm your body. It can cause organ damage and even be life-threatening. So, getting a transfusion quickly is key in severe cases.
Are there alternative treatments to blood transfusion for anemia?
Yes, there are other treatments for anemia. These include iron supplements, changing your diet, and erythropoietin-stimulating agents. Your doctor might suggest these based on your anemia’s cause.
How is the decision to transfuse made?
Deciding on a transfusion depends on the patient’s situation. This includes how severe the anemia is, any underlying health issues, and symptoms. Doctors follow guidelines to make this decision.
References
World Health Organization. Evidence-Based Medical Insight. Retrieved from https://www.who.int/publications/i/item/9789241548510