We are always looking to improve pediatric care. A key part of this is knowing when to give blood to kids. Doctors decide to transfuse based on the child’s hemoglobin levels and how they’re feeling, and a blood transfusion for anemia is often considered when levels are too low.
New global guidelines suggest a restrictive approach to blood transfusions. They highlight the importance of weighing the risks of transfusion against the need to treat severe anemia.
Pediatric transfusion is a complex field. It involves children from newborns to young adults. Because there’s not enough research, doctors must tailor care to each child’s needs.
Key Takeaways
- A restrictive approach to blood transfusion is recommended in pediatrics.
- Hemoglobin concentration and clinical assessment guide transfusion decisions.
- Individualized care is key in pediatric transfusion.
- Age, clinical condition, and lab results affect transfusion choices.
- Guidelines vary by clinical scenario and age group.
Understanding Pediatric Blood Transfusion Basics
It’s key for healthcare providers to know about pediatric blood transfusions. These transfusions are vital for kids with anemia, bleeding issues, and cancer. They help save lives.
The Purpose of Blood Transfusions in Children
Blood transfusions in kids do many important things. They help move oxygen to tissues and improve blood flow. They also support the body during sickness or surgery.
Doctors decide to give blood based on how sick the child is and lab tests. They look at the hemoglobin level for transfusion. They must think about the benefits and risks for each child.
Key Differences Between Adult and Pediatric Transfusions
Pediatric transfusions are different from adult ones. Kids have smaller blood volumes and changing blood values as they grow. So, transfusions must fit the child’s age, weight, and health.
The amount of PRBC transfusion (Packed Red Blood Cells) is based on the child’s weight. It’s usually 10 to 20 ml per kg of body weight.
Components of Blood Used in Pediatric Transfusions
Pediatric transfusions use red blood cells, plasma, and platelets. Each part is for a specific need. Red blood cells help with oxygen, and platelets stop bleeding.
Knowing when to use these blood parts is vital. A blood transfusion chart helps doctors make the right choices.
General Guidelines for Blood Transfusion for Anemia in Children
Healthcare providers must carefully consider the benefits and risks of blood transfusions for children with anemia. Recent guidelines suggest a more cautious approach. They recommend transfusions for critically ill, stable children when their hemoglobin is less than 7 g/dL.
Hemoglobin Concentration as a Primary Indicator
Hemoglobin levels are key in deciding if a child needs a blood transfusion. For kids over four months, a transfusion might be needed if they lose more than 15% of their blood or if their hemoglobin is below 70 g/L with anemia symptoms.
We focus on hemoglobin levels because they show how severe anemia is. Monitoring these levels helps us decide if a transfusion is needed and if it’s working.
The Shift Toward Restrictive Transfusion Approaches
Pediatric care is moving toward more careful blood transfusion practices. Now, transfusions are recommended at lower hemoglobin levels than before. This change aims to lower the risks of blood transfusions, such as complications.
- Restrictive transfusion strategies help in reducing unnecessary transfusions.
- They are associated with fewer transfusion-related adverse events.
- Evidence supports that restrictive approaches do not compromise patient outcomes in many cases.
Clinical Assessment Beyond Laboratory Values
Laboratory values like hemoglobin are important, but so is the child’s overall health. We look at signs of anemia, like a fast heart rate, poor blood flow, or trouble exercising.
Clinical judgment is key in deciding if a child needs a blood transfusion. We consider the cause of anemia, other health issues, and how well the child can handle anemia.
By using both lab results and clinical assessment, we make better decisions about blood transfusions for children with anemia. This ensures they get the best care possible.
Hemoglobin Thresholds for Different Clinical Scenarios
In pediatric care, knowing the right hemoglobin levels is key. It helps decide when to give blood transfusions. Healthcare providers use these levels to know when a transfusion is needed.
Critically Ill, Hemodynamically Stable Children
For kids who are very sick but stable, a hemoglobin level of 7 g/dL is the threshold for blood transfusion. This is based on guidelines and studies showing its importance. It helps weigh the benefits and risks of blood transfusions.
We look at each patient’s situation. This includes signs of anemia like extreme tiredness, short breath, or pale skin.
Non-Life-Threatening Bleeding Cases
In non-life-threatening bleeding, blood transfusion is usually for kids with hemoglobin below 5 g/dL. For those with Hb levels between 5“7 g/dL, it depends on the situation and symptoms. We check the bleeding’s severity, the patient’s stability, and lab results.
Chronic Anemia Management
For kids with chronic anemia, we’re more careful with blood transfusions. Transfusion is considered when Hb drops below 7 g/dL (hgb7.0) or when symptoms are severe. We also look at other treatments like iron and erythropoiesis-stimulating agents.
Understanding and using these hemoglobin levels helps healthcare providers make smart decisions. This ensures blood transfusions are safe and effective for kids.
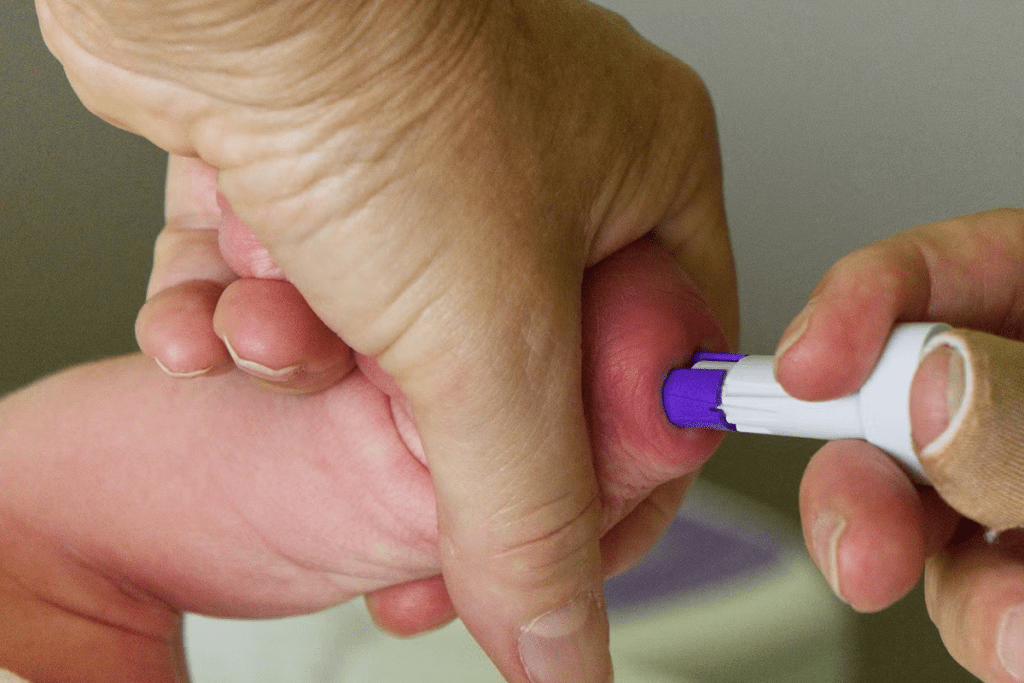
Special Considerations for Neonatal Transfusions
Deciding to give blood to newborns is complex. It involves understanding their special needs. Newborns, including premature or sick ones, often need blood transfusions. We look at their age, health, and need for breathing help to decide the best transfusion plan.
Individualized Approaches Based on Gestational Age
Gestational age is key in deciding if a newborn needs a blood transfusion. Preterm babies, for example, might need more transfusions because their blood-making system is not fully developed. We adjust our transfusion plans based on each baby’s age, weight, and health.
When a newborn has low hemoglobin, we carefully decide if they need a blood transfusion. We consider how severe their anemia is, if they’re having trouble breathing, and if they need oxygen. This helps us figure out when is blood transfusion is needed for low hemoglobin.
Higher Thresholds for Neonates on Respiratory Support
Babies needing breathing help often need more hemoglobin to get enough oxygen. We follow guidelines to keep their hemoglobin levels higher. This helps prevent tissue damage and improves their health.
Using restrictive transfusion strategies is common in neonatal care. But for babies needing breathing support, we might need to transfuse more. We aim to balance the benefits of transfusion against the risks, like complications from the transfusion.
Unique Risks and Benefits in the Neonatal Population
Transfusing blood to newborns has its own set of risks and benefits. Transfusions can help with oxygen delivery and fight anemia, which is important for their growth. But, they also carry risks like infections and immune system problems. We carefully consider these risks and benefits when deciding on transfusions.
In summary, neonatal transfusions need a personalized approach. We consider the baby’s age, health, and breathing needs. This way, we can give the best care to our youngest patients.
Transfusion Guidelines for Children with Cardiac Conditions
Children with heart disease face unique challenges when it comes to blood transfusions. It’s important to manage their care carefully. We must consider their heart condition, overall health, and the situation of the transfusion.
Thresholds for Single-Ventricle Palliation
Children who have had single-ventricle palliation need a hemoglobin level of about 9 g/dL for transfusions. This level is key to ensuring their heart gets enough oxygen. Keeping the hemoglobin level right is essential for their heart’s health.
Key considerations for single-ventricle palliation include:
- Maintaining optimal oxygen delivery
- Ensuring adequate blood flow
- Monitoring for signs of anemia or hypoxia
Monitoring During Transfusion in Cardiac Patients
Watching closely is vital during blood transfusions for children with heart issues. We keep an eye on their heart rate, blood pressure, and oxygen levels. This helps us spot any problems quickly. We also watch for signs of complications like fluid overload or allergic reactions.
Effective monitoring strategies include:
- Continuous vital sign monitoring
- Regular assessment of the child’s clinical status
- Prompt intervention in case of adverse reactions
By managing blood transfusions carefully and following guidelines, we can reduce risks. This helps ensure the best outcomes for children with heart conditions.
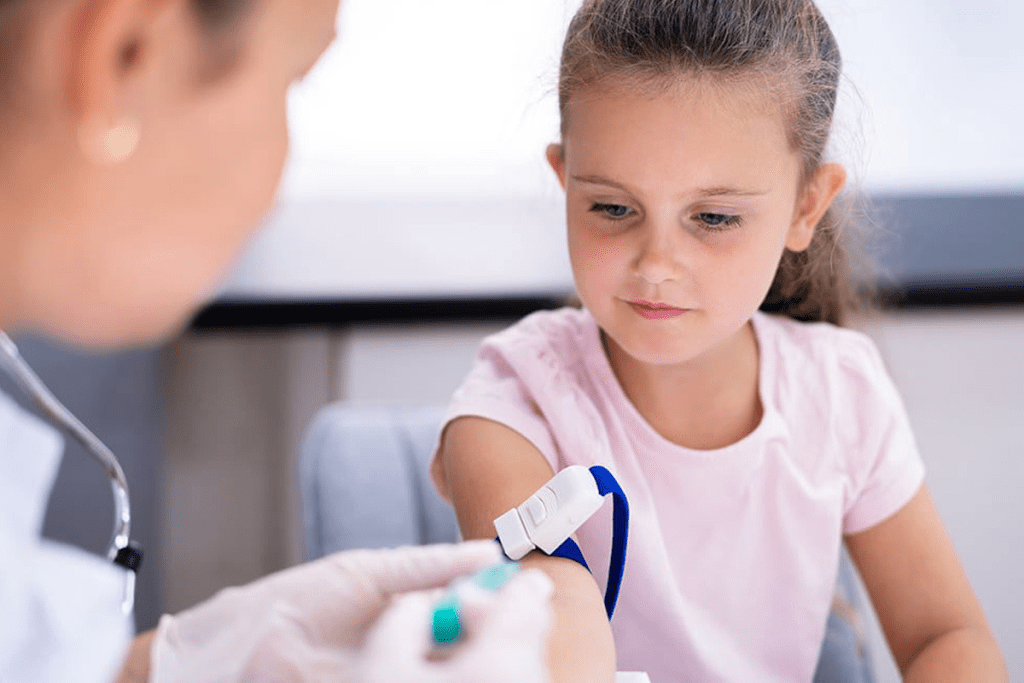
Practical Aspects of Pediatric Blood Transfusion
Ensuring the safety and success of pediatric blood transfusions is key. When giving blood to kids, we must think about several things. These include how much blood to give and the chance of bad reactions.
Standard Transfusion Volumes
For kids, the usual amount of blood given is between 10 and 20 ml/kg of body weight. This is for red blood cell transfusions, which help with anemia or blood loss. It’s important not to give too much, to avoid problems.
A 20 kg child would get 200-400 ml of blood. But the exact amount depends on the child’s health, blood levels, and other factors.
Key Considerations for Transfusion Volume:
- Patient weight in kilograms
- Severity of anemia or blood loss
- Hemoglobin levels before and after transfusion
- Clinical symptoms and overall health status
Managing Possible Transfusion Reactions
It’s important to watch for and manage any bad reactions from blood transfusions. While rare, these can range from mild to severe. Common issues include allergic reactions, febrile non-hemolytic reactions, and very rarely, hemolytic reactions.
To keep risks low, we closely watch the patient during and after the transfusion. We check their vital signs often. If a reaction happens, we act fast. A blood transfusion chart helps track the transfusion and spot any problems.
“Monitoring patients closely during blood transfusions is critical for early detection and management of any adverse reactions.”
In summary, the practical sides of pediatric blood transfusions are very important. This includes knowing how much blood to give and how to handle any bad reactions. By sticking to guidelines and using tools like a blood transfusion chart, we can make sure kids get the best care.
When to Consider Alternatives to Blood Transfusion
When looking at treatment options for kids with anemia, it’s key to think about other choices instead of blood transfusions. There are many ways to handle anemia, which can cut down on the need for blood transfusions in kids.
Iron Supplementation Strategies
Iron supplements are a common alternative to blood transfusions for kids with iron-deficiency anemia. Oral iron supplements are usually the first choice, with ferrous sulfate being a common pick. The amount and length of iron treatment depend on how bad the anemia is and how well the child responds.
The National Institutes of Health says iron supplements can help manage iron-deficiency anemia well, making blood transfusions less necessary.
- Oral iron supplements are the first choice for treatment.
- Parenteral iron therapy might be used if oral iron doesn’t work or if the anemia is severe.
- It’s important to keep an eye on iron levels and hemoglobin during treatment.
Erythropoiesis-Stimulating Agents
Erythropoiesis-stimulating agents (ESAs) are another option instead of blood transfusions. ESAs help make more red blood cells, which is good for kids with chronic diseases like chronic kidney disease.
ESAs can help lower the need for blood transfusions in kids with ongoing anemia. But it’s important to weigh the risks and benefits carefully.
“The use of ESAs has been shown to reduce the need for blood transfusions in patients with chronic kidney disease.”
– Source: National Kidney Foundation
Blood Conservation Techniques
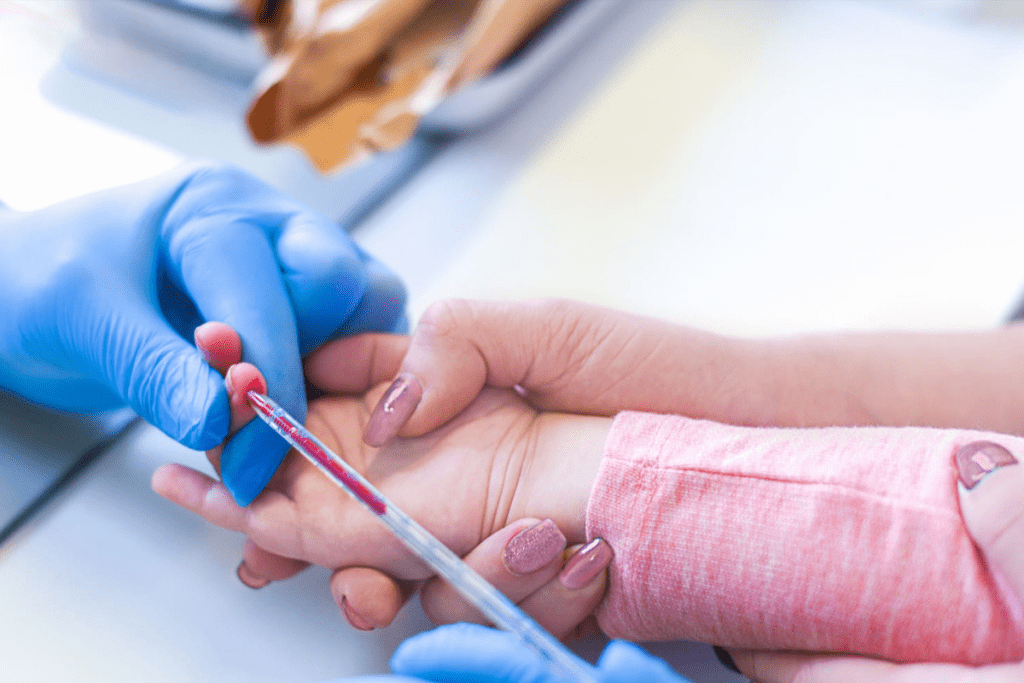
Using techniques to save blood is also key to reducing blood transfusions. This includes taking fewer blood samples for tests, using smaller tubes for blood draws, and using point-of-care testing.
- Try to take fewer blood samples by doing tests together.
- Use smaller tubes for blood draws to take less blood.
- Use point-of-care testing to avoid needing to take blood multiple times.
By using these blood-saving techniques, doctors can greatly reduce the need for blood transfusions in kids.
Conclusion: Balancing Benefits and Risks in Pediatric Transfusion Practice
We’ve looked at the key points for blood transfusions in kids, focusing on the balance between good and bad. Deciding to give blood for anemia or other issues needs careful thought. This includes checking the hemoglobin levels and what each child needs.
When it comes to blood transfusions in kids, we must think about the good and the bad. Knowing the guidelines helps doctors make smart choices. This ensures kids get the care they need safely and effectively.
Managing blood transfusions for anemia and other issues in kids requires a careful approach. We need to consider hemoglobin levels, the situation, and what each child needs. We must keep learning to make transfusions better for kids.
FAQ
What are the key considerations for deciding when to transfuse blood in pediatric patients?
The decision to transfuse blood in kids depends on several factors. These include the child’s age, their health condition, and lab results like hemoglobin levels.
What is the primary indicator for blood transfusion in children with anemia?
Hemoglobin levels are key to deciding on blood transfusions in kids with anemia. Guidelines suggest different levels based on the child’s situation.
What are the hemoglobin thresholds for blood transfusion in critically ill, hemodynamically stable children?
For kids who are very sick but stable, a hemoglobin level of 7 g/dL is often recommended. But this can change based on the child’s specific situation.
How do transfusion guidelines differ for neonates, particularly those on respiratory support?
Neonates and those on breathing support might need higher hemoglobin levels for transfusions. Decisions are made based on their age and health.
What are the standard transfusion volumes for pediatric blood transfusions?
For kids, blood transfusions usually range from 10 to 20 ml/kg. This amount is based on the child’s weight.
What alternatives to blood transfusion are available for managing anemia in pediatric patients?
Instead of blood transfusions, kids can get iron supplements, erythropoiesis-stimulating agents, or blood-saving techniques. These can help manage anemia and reduce the need for transfusions.
When is a blood transfusion needed for low hemoglobin levels in children?
Blood transfusions are considered when a child’s hemoglobin is below a certain threshold. For example, critically ill kids might need transfusions at a level of 7 g/dL.
What are the signs that a child may need a blood transfusion for anemia?
Signs a child might need a blood transfusion include severe tiredness, shortness of breath, and other symptoms of not getting enough oxygen. But the decision to transfuse is based on a full clinical evaluation.
How are transfusion decisions made for children with cardiac conditions?
Decisions on blood transfusions for kids with heart conditions follow specific guidelines. These include rules for single-ventricle palliation. Transfusions are closely monitored to ensure they are safe and effective.
What are the unique risks and benefits associated with blood transfusions in neonates?
Blood transfusions in newborns have both risks and benefits. Risks include complications, while benefits include better oxygen delivery. These need careful thought and individualized decisions.
References
- U.S. National Library of Medicine. (2022). Transfusion Practices in Pediatric Cardiac Surgery. Frontiers in Pediatrics, 10, 900693. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9349887/









