Last Updated on December 3, 2025 by mcelik

When a bone fracture happens, the body starts a complex healing process. Did you know that about 6.8 million people in the United States get fractures every year? Many need surgery to heal. Knowing how a bone fracture heals is key for patients to recover well.
We’ll take you through the four main stages of bone fracture healing. You’ll learn about the biological steps and what to expect in each stage. Understanding these stages helps patients get their treatment plans and make smart care choices.
Key Takeaways
- The fracture healing process involves four distinct stages.
- Understanding these stages is key for effective recovery.
- The body’s natural response to a fracture starts the healing process.
- Each stage is important for getting bone strength and function back.
- Knowing the healing stages helps patients make informed treatment choices.
Understanding Bone Fractures
The human skeleton is strong but can break. These breaks, called fractures, happen from trauma or osteoporosis. They can really change someone’s life, so it’s key to know about them and how our body fixes them.
Definition and Basic Anatomy of Bones
Bones are hard, calcified parts that make up our skeleton. They support us, protect us, and help us move. A bone fracture is when a bone breaks, from a small crack to a full break.
The parts of a bone include the periosteum (outer layer), cortex (compact bone layer), and endosteum (inner layer). Knowing about these parts helps us understand how bones heal.
| Layer | Description | Function |
| Periosteum | Outer layer covering the bone | Provides blood supply and aids in bone repair |
| Cortex | Compact bone layer | Provides structural support and protection |
| Endosteum | Inner layer lining the bone cavity | Involved in bone resorption and formation |
Common Causes of Bone Fractures
Fractures can come from trauma, osteoporosis, or too much stress. Traumatic fractures happen from big impacts, like falls or car crashes. Osteoporotic fractures occur when bones weakened by osteoporosis break easily.
Stress fractures come from too much stress or overuse. Pathological fractures happen when a bone is weakened by disease, like cancer.
| Cause | Description | Common Examples |
| Trauma | High-force impact or stress | Falls, car accidents, sports injuries |
| Osteoporosis | Bones weakened by disease | Hip fractures in the elderly |
| Repetitive Stress | Overuse or repetitive strain | Stress fractures in athletes |
Types of Bone Fractures
Bone fractures come in different types, each with its own healing process. Knowing these types is key for proper diagnosis and treatment.
Simple vs. Compound Fractures
Fractures are mainly split into simple and compound types. Simple fractures happen when the bone breaks but doesn’t go through the skin. On the other hand, compound fractures occur when the bone does break through the skin, raising the chance of infection.
Simple fractures are usually less complicated and have a lower risk of getting infected. But, both types need quick medical care to heal right.
Complete vs. Incomplete Fractures
Fractures can also be classified by how complete they are. Complete fractures are breaks that go all the way through the bone, splitting it. Incomplete fractures are cracks that don’t fully go through the bone.
Complete fractures can be either displaced or non-displaced, depending on if the bone pieces are out of place. Incomplete fractures, often found in kids, can be harder to spot because they’re only partial breaks.
Other Classification Methods
Fractures can also be sorted by their pattern and where they happen. For example, transverse fractures are at a right angle to the bone’s axis. Oblique fractures, on the other hand, have an angled pattern.
Comminuted fractures are when the bone breaks into many pieces. Segmental fractures have two or more breaks in the same bone. Knowing these patterns helps doctors figure out the best treatment.
| Fracture Type | Description | Characteristics |
| Simple (Closed) | Break does not pierce the skin | Less risk of infection |
| Compound (Open) | Break pierces the skin | Higher risk of infection |
| Complete | Break goes entirely through the bone | May be displaced or non-displaced |
| Incomplete | Crack does not completely traverse the bone | Often seen in children |
The Importance of Proper Bone Healing
Proper bone healing is key to getting back to normal after a fracture. The body starts healing when a bone breaks, but results can vary. This depends on the fracture’s severity, treatment, and the patient’s health.
Long-term Consequences of Improper Healing
Bad healing can cause lasting problems like malunion, non-union, and chronic pain. Malunion means the bone heals wrong, leading to deformity and limited movement. Non-union means the bone doesn’t heal, causing ongoing pain and instability.
These issues can greatly affect a person’s life and ability to do everyday things. It’s vital to manage bone fractures well to avoid these problems and ensure a good recovery.
| Complication | Description | Potential Impact |
| Malunion | Bone heals in an incorrect position | Deformity, limited mobility |
| Non-union | Bone fails to heal | Persistent pain, instability |
| Chronic Pain | Ongoing pain due to improper healing | Reduced quality of life, decreased mobility |
The Body’s Natural Healing Mechanism
The body’s healing process is complex, involving inflammation, soft callus, hard callus, and bone remodeling. Knowing this helps us see why proper healing is so important. It also shows the role of medical help in supporting the osteogenic healing process.
First, a hematoma forms at the break, then a soft callus. This callus turns into a hard one through mineralization. Eventually, the bone heals fully.
The time it takes for a bone to heal can differ a lot. It depends on age, health, and fracture severity. Healing can take weeks to months. It’s important to follow a doctor’s advice during this time.
Understanding bone healing and the body’s process helps patients see why proper care is essential. It ensures the best possible outcome.
Bone Fracture Healing Stages: An Overview
Knowing the stages of bone fracture healing is key. It shows how our bodies fix themselves. The healing is a series of complex steps that work together.
Timeline of the Complete Healing Process
The healing of a bone fracture goes through four stages. These are inflammation, soft callus, hard callus, and bone remodeling. How long each stage lasts depends on the fracture’s severity, the person’s health, and treatment.
- Inflammation Stage: This first stage lasts a few days to a week. It’s the body’s quick response to injury.
- Soft Callus Formation: About 2-3 weeks after the fracture, a soft callus forms. It gives the bone some stability.
- Hard Callus Formation: This stage can last weeks to months. It replaces the soft callus with a harder one.
- Bone Remodeling: The last stage can take months to a year or more. It shapes and strengthens the new bone.
Cellular and Molecular Players in Fracture Repair
Healing a bone fracture is a complex process. It involves many cells and molecules. Key players are:
- Osteoblasts: These cells make and mineralize bone matrix.
- Osteoclasts: These cells are important in bone resorption during remodeling.
- Cytokines and Growth Factors: These molecules help with inflammation and cell growth.
- Stem Cells: These cells can turn into different cell types, helping in healing.
The healing of a bone fracture shows our body’s amazing repair skills. By knowing the stages and the cells and molecules involved, we can see the complex biology at work.
Stage1: Hematoma Formation Phase

Hematoma formation is the first step in healing a bone fracture. It involves inflammation and clotting. When a bone breaks, the body quickly starts to heal it, beginning with a hematoma.
Initial Inflammatory Response
The initial inflammatory response is key in the hematoma formation phase. When a bone fractures, it and the surrounding tissue get damaged. This damage leads to bleeding into the fracture site, forming a hematoma.
This hematoma is made of blood cells, platelets, and biochemical signals. These signals start the healing process. The inflammatory response is important for clearing debris and preparing for healing.
Blood Clot Formation at the Fracture Site
Blood clot formation is vital in the hematoma. The clot acts as a temporary matrix for healing cells. It’s made by platelets and the coagulation cascade, creating a stable hematoma.
This hematoma provides a scaffold for the initial stages of fracture repair. It supports the influx of cells needed for healing.
Cellular Activity During Hematoma Formation
During hematoma formation, many cellular activities start. The hematoma is not just blood; it’s an active environment. It recruits and activates various cell types.
These include inflammatory cells, mesenchymal stem cells, and endothelial cells. They proliferate and differentiate, preparing for bone healing.
| Cell Type | Role in Hematoma Formation |
| Inflammatory Cells | Clear debris, release cytokines |
| Mesenchymal Stem Cells | Differentiate into osteoblasts and chondrocytes |
| Endothelial Cells | Initiate angiogenesis, supporting tissue regeneration |
The hematoma formation phase is complex and essential for bone fracture healing. Understanding this phase helps us see how the body heals itself. It shows the importance of inflammation and hematoma formation for healing.
The Inflammatory Response in Fracture Healing
Inflammation is key to healing bone fractures. When a bone breaks, the body sends more blood to the area. This leads to inflammation.
This response is not just a reaction. It’s a detailed process involving cells and proteins. It’s essential for starting the healing, clearing debris, and preparing for repair.
Role of Cytokines and Growth Factors

Cytokines and growth factors are vital in the inflammatory response. Cytokines are proteins that help cells talk to each other. They make sure the healing process starts and keeps going.
Growth factors, like BMPs, PDGF, and VEGF, help new tissue and bone grow. They are important for fixing the bone.
| Growth Factor | Function in Fracture Healing |
| BMPs | Induce bone formation and differentiation of mesenchymal cells into osteoblasts and chondrocytes. |
| PDGF | Promotes cell proliferation and chemotaxis, enhances the healing process. |
| VEGF | Stimulates angiogenesis, improving blood supply to the healing fracture. |
Vascular Changes During Inflammation
During inflammation, blood flow to the fracture site increases. This brings cells and nutrients needed for repair. New blood vessels form, ensuring oxygen and nutrients reach the healing bone.
The inflammatory response is complex but essential for healing. Understanding it can help find new ways to improve bone repair.
Stage2: Soft Callus Formation
Soft callus formation is the second stage in bone fracture healing. It involves the growth of fibrocartilage and collagen matrix. This stage is key because it gives the bone the stability it needs to heal further.
Fibrocartilage Development
In the soft callus stage, fibrocartilage starts to form at the fracture site. This cartilage is full of collagen, which helps in bone formation. It’s a vital step as it fills the gap in the bone, giving it initial strength.
Collagen Matrix Formation in Fracture Healing
The collagen matrix is another important part of this stage. It acts as a base for new bone to grow on. The matrix is made of different collagen types, mainly Type I and Type II. It supports the bone’s mineralization and remodeling.
Cellular Changes During Soft Callus Phase
During the soft callus phase, many cellular changes happen. The area around the fracture is filled with cells like chondrocytes, osteoblasts, and fibroblasts. These cells work together to create the matrix needed for the soft callus. Their activity is controlled by growth factors and cytokines.
As the soft callus stage goes on, the soft callus turns into a harder, more stable one. This marks the start of the next healing stage. Understanding this stage is key to seeing how bones heal after a fracture.
The Role of Osteoblasts in the Fracture Healing Process
Osteoblasts play a key role in healing bone fractures. They are cells that help form new bone tissue. Their work is vital for fixing broken bones.
Osteoblast Activation and Proliferation
The healing starts with activating and growing osteoblasts. This step brings these cells to the broken bone area. After being activated, they multiply, helping the bone to heal.
Many things can trigger osteoblasts to start working. Growth factors and cytokines are among them. These signals help osteoblasts do their job in healing the bone.
Bone Matrix Production
Osteoblasts make bone matrix, which are mostly collagen and proteins. This matrix is the base for bone hardening. Minerals like calcium and phosphate are added to make it strong.
This bone matrix is key for healing. It gives the new bone a structure and helps it connect with the old bone.
| Osteoblast Function | Description | Importance in Fracture Healing |
| Osteoblast Activation | Recruitment and activation of osteoblasts to the fracture site | Critical for initiating the bone healing process |
| Proliferation | Increase in osteoblast numbers to support healing | Ensures sufficient osteoblasts for effective bone formation |
| Bone Matrix Production | Production of collagen and other proteins to form bone matrix | Provides the structural framework for new bone formation and mineralization |
We’ve looked at how osteoblasts help heal fractures. They start by getting activated and growing. Then, they make the bone matrix. Understanding their role helps us see the amazing biology behind fixing broken bones.
Stage3: Hard Callus Formation
Hard callus formation is the third stage in bone fracture healing. It’s a big step towards fixing the break. At this point, the body turns the soft callus from the last stage into a harder, more stable form.
Bone Mineralization Process
The bone mineralization process is key in hard callus formation. It adds minerals like calcium and phosphate to the bone, making it stronger. Osteoblasts, special cells, help by adding proteins and minerals.
As minerals are added, the callus gets stronger. This is important for the bone to handle normal stresses and loads.
Conversion of Soft Callus to Woven Bone
During hard callus formation, the soft callus turns into woven bone. This change involves many cells working together. Woven bone is a temporary structure that will later become more organized.
The process starts with a collagen matrix, which then gets mineralized. This creates a hard callus that adds a lot of stability to the fracture site.
Mechanical Stability During Hard Callus Phase
Mechanical stability is a big deal in the hard callus stage. As the soft callus turns into woven bone, the fracture site gets stronger. This strength is vital for supporting the bone while it heals.
This stability comes from bone mineralization and the change from soft callus to woven bone. It’s important to keep the fracture site stable to avoid complications.
| Characteristics | Soft Callus | Hard Callus |
| Composition | Fibrocartilage | Woven Bone |
| Mechanical Stability | Low | High |
| Mineralization | Minimal | Significant |
Vascular Tissue Growth in Skeletal Repair
Vascular tissue growth is key in healing bone fractures. It helps bring oxygen and nutrients to the damaged area. This growth is vital for bone repair.
Angiogenesis During Bone Repair
Angiogenesis, or making new blood vessels, is important in bone repair. This complex process involves many cell types, growth factors, and signals. We’ll look into how angiogenesis starts and is controlled during bone healing.
Angiogenesis starts with specific growth factors and cytokines at the fracture site. These signals help endothelial cells grow and form new blood vessels. This network is key for delivering oxygen and nutrients to the healing bone.
Oxygen and Nutrient Supply to Healing Bone
New blood vessels are essential for delivering oxygen and nutrients to the healing bone. Adequate oxygen is needed for osteoblasts to work well. We’ll talk about how blood supply affects healing and what can influence this balance.
- Oxygen supply is key for osteoblast function and bone matrix production.
- Nutrient delivery supports the energy needs of healing.
- The vascular network also removes waste, keeping the repair area healthy.
Understanding vascular tissue growth in bone repair shows the complex healing process. This knowledge helps us find ways to improve healing and better patient outcomes.
Stage4: Bone Remodeling Phase
The final stage in bone fracture healing is the bone remodeling phase. It’s a key time when the new bone is reshaped and gets stronger.
In this phase, osteoclasts are very important for breaking down bone tissue. These cells are in charge of removing damaged or old bone. This makes room for new bone to grow.
Osteoclast Resorption Process
This step is vital for the bone to heal right. It prepares the bone for new tissue to form. This way, the bone gets back its strength.
Reshaping and Strengthening of New Bone
After the bone is broken down, osteoblasts start making new bone. They replace the first bone with stronger, more organized bone. This makes the bone not only look right but also be strong.
Timeline for Complete Remodeling
How long it takes to fully remodel the bone varies. It depends on age, diet, and health. It can take months to years.
During this time, osteoclasts and osteoblasts work together. They make sure the new bone is not just reshaped but also gets stronger. This helps the bone get back to its original shape and function.
Factors Affecting the Fracture Recovery Timeline
Many things can change how long it takes to heal from a bone fracture. Knowing these factors is key for the best healing. The speed of recovery depends on many things.
Age and Overall Health
Age is a big factor in healing from a fracture. Older people heal slower because their bones are less dense. They might also have other health issues.
Being healthy is very important for healing. This means managing health problems and living a healthy life.
Nutrition and Dietary Factors
Nutrition is very important for healing bones. Foods with calcium, vitamin D, and protein help a lot. Eating foods with these nutrients can help healing.
Eating well is a big part of healing from a fracture. We suggest eating foods full of calcium, vitamin D, and protein. This helps keep bones strong.
Medications and Medical Conditions
Some medications and health issues can slow down healing. For example, steroids can slow healing. Osteoporosis might need extra treatment.
Telling your doctor about any medicines or health issues is important. We help manage these to help you heal faster.
Mechanical Factors and Fracture Stabilization
Mechanical factors like how stable the fracture is are very important. The fracture needs to be stable to heal right.
We focus on making sure the fracture is stable. This can be done with casts or surgery, depending on the case.
Medical Interventions to Support the Osteogenic Healing Process
Medical interventions are key in helping bones heal. We use many strategies, like immobilization and surgery, to aid in bone repair. These methods help bones mend better.
Immobilization Techniques
Immobilization is vital for bone healing. Methods like casting and bracing keep the bone in place. This helps the bone heal right.
Depending on the fracture, we choose the right immobilization method. For stable fractures, casts work well. Bracing is better for fractures needing extra support.
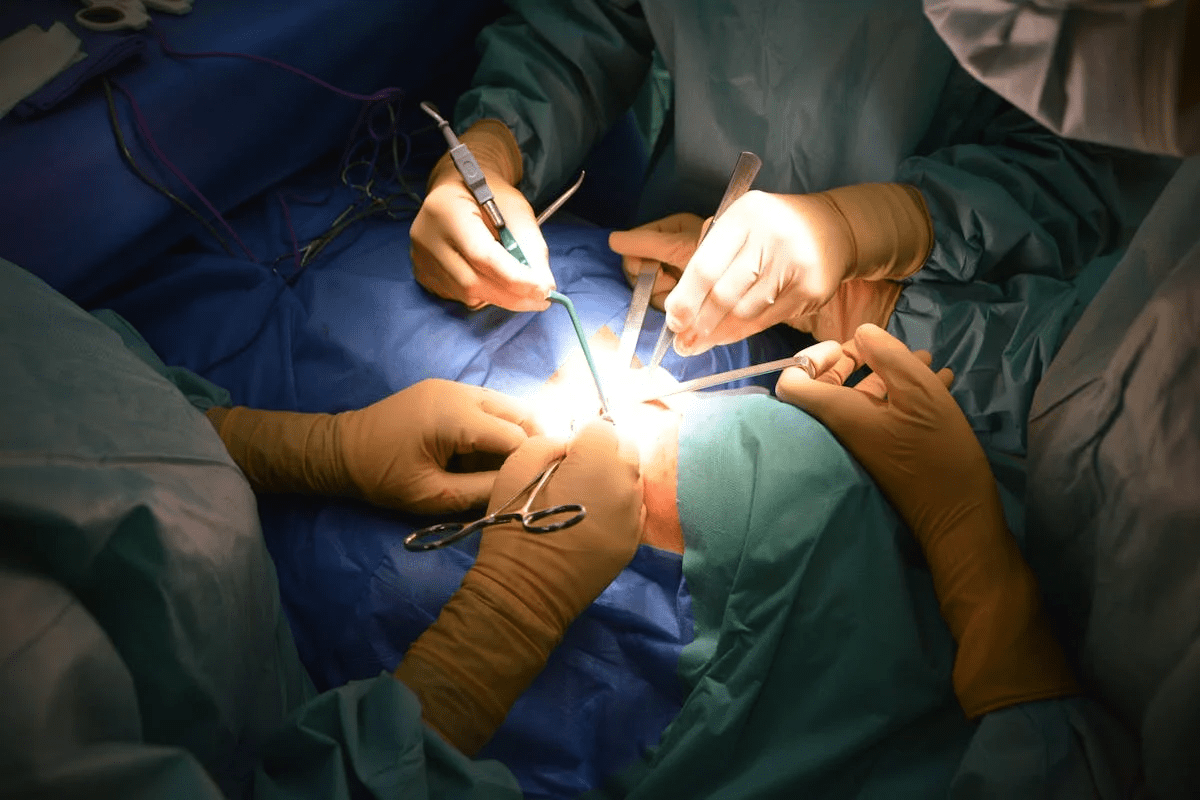
Surgical Approaches for Complex Fractures
For complex fractures, surgery is often needed. Surgical approaches like ORIF or intramedullary nailing help align bones for healing.
We pick the best surgery based on the fracture and patient health. This choice helps avoid complications and improves healing.
Emerging Therapies for Enhanced Healing
New therapies are changing bone healing. Emerging therapies like BMPs and PRP therapy are promising. They help bones heal faster and better.
We keep up with these new treatments. By using the latest research, we offer our patients the best care. This approach improves healing outcomes.
Complications in the Fracture Site Strengthening
Complications during fracture healing can greatly affect patient outcomes. Understanding the possible issues that can happen during fracture site strengthening is key.
Delayed Union and Non-union
Delayed union and non-union are serious issues. Delayed union means healing takes longer than expected. Non-union means the fracture doesn’t heal at all.
Many things can cause these problems. These include not keeping the bone in place long enough, not enough blood flow, and infection. Spotting these early helps us take the right steps.
Malunion and Improper Alignment
Malunion happens when the bone heals wrong, causing deformity and pain. This can happen if the bone isn’t set right or held in place well.
To avoid malunion, setting the bone correctly and keeping it stable is vital. We use surgery and other methods to help the bone heal right and avoid malunion.
Infection and Other Complications
Infection is a big problem that can slow healing. Bacterial colonization at the fracture site can cause infection. This can lead to delayed or non-union, or even more surgery.
Other issues like nerve damage, blood vessel problems, or device failure can also happen. We manage these risks with good wound care, antibiotics, and watching the patient closely.
Knowing about these complications helps us prevent them. This way, we can ensure the best results for patients getting fracture site strengthening.
Rehabilitation and Physical Therapy During the Fracture Healing Process
Recovering from a bone fracture is more than just healing the bone. It also involves rehabilitation and physical therapy to get back to normal. These steps are key to restoring function and aiding in the healing process. A well-planned rehabilitation program is essential as we move through the healing stages.
Early Mobilization Strategies
Early mobilization is vital in the recovery process. It helps prevent stiffness and promotes healing. Gentle exercises and movements are started early to:
- Maintain range of motion
- Reduce muscle atrophy
- Enhance circulation
Early mobilization strategies include passive and active exercises. Passive exercises involve a healthcare provider or physical therapist moving the limb. Active exercises are when the patient moves their limb on their own.
Progressive Strengthening Exercises
As the fracture heals, strengthening exercises become more important. These exercises aim to:
- Improve muscle strength around the fracture site
- Enhance bone density
- Support the return to normal activities
A physical therapist will create a personalized exercise plan. This plan starts with low-intensity exercises and gradually gets more challenging. It’s tailored to the patient’s needs and recovery stage.
Return to Normal Activities
The main goal of rehabilitation and physical therapy is to safely return patients to their normal activities. This means regaining strength, mobility, and ensuring the bone is fully healed. The bone must be strong enough to handle normal stresses and loads.
| Activity Level | Timeline | Guidelines |
| Low-Impact Activities | 6-8 weeks | Start with low-impact activities like walking or swimming |
| Moderate Activities | 8-12 weeks | Progress to moderate activities, including cycling or light jogging |
| High-Impact Activities | 12+ weeks | Gradually return to high-impact activities, such as running or jumping, under the guidance of a healthcare provider |
Following a structured rehabilitation and physical therapy program helps patients recover better. It minimizes complications and leads to the best outcomes after a bone fracture.
Conclusion
We’ve looked at the four stages of healing a bone fracture. Each stage is key to getting the bone strong again. These stages are hematoma formation, soft callus formation, hard callus formation, and bone remodeling.
The healing of a bone fracture is complex. It depends on age, nutrition, and how stable the bone is. Rehabilitation helps a lot by making sure the bone heals right and the patient can move well again.
Healthcare providers can make better treatment plans by knowing about bone healing stages and what affects it. Rehabilitation is very important. It helps patients get back their strength, mobility, and function.
FAQ
What are the four stages of bone fracture healing?
The healing of a bone fracture goes through four stages. First, a hematoma forms. Then, a soft callus is created. Next, a hard callus is formed. Lastly, the bone is remodeled.
How long does the bone fracture healing process take?
Healing a bone fracture can take weeks to months. It depends on your age, diet, and how severe the break is.
What is the role of osteoblasts in bone healing?
Osteoblasts are key in bone healing. They make bone matrix and help mineralize it.
What are the possible complications of bone fracture healing?
Complications can include delayed or non-union, malunion, and infection. These can slow down or stop healing.
How can I optimize my nutrition for better bone healing?
For better bone healing, eat enough calcium, vitamin D, and protein. Also, keep your diet balanced.
What is the importance of immobilization in bone fracture healing?
Immobilization is key. It keeps the fracture stable, helping the bone heal right.
Can certain medications affect bone fracture healing?
Yes, some meds like corticosteroids and NSAIDs can slow healing. They can delay or hinder the process.
What is the role of physical therapy in bone fracture rehabilitation?
Physical therapy is vital. It helps with early movement, strengthening, and getting back to normal life.
How does age affect bone fracture healing?
Age impacts healing. Older people heal slower because of less bone density and cell activity.
What is bone remodeling, and how long does it take?
Bone remodeling is the final healing stage. It reshapes and strengthens the bone. This can take months to years.
References
- Egermann, M., et al. (2023). Fracture healing research: Recent insights. Bone Reports, 17, 101289. https://www.sciencedirect.com/science/article/pii/S2352187223000347