Last Updated on November 17, 2025 by Ugurkan Demir
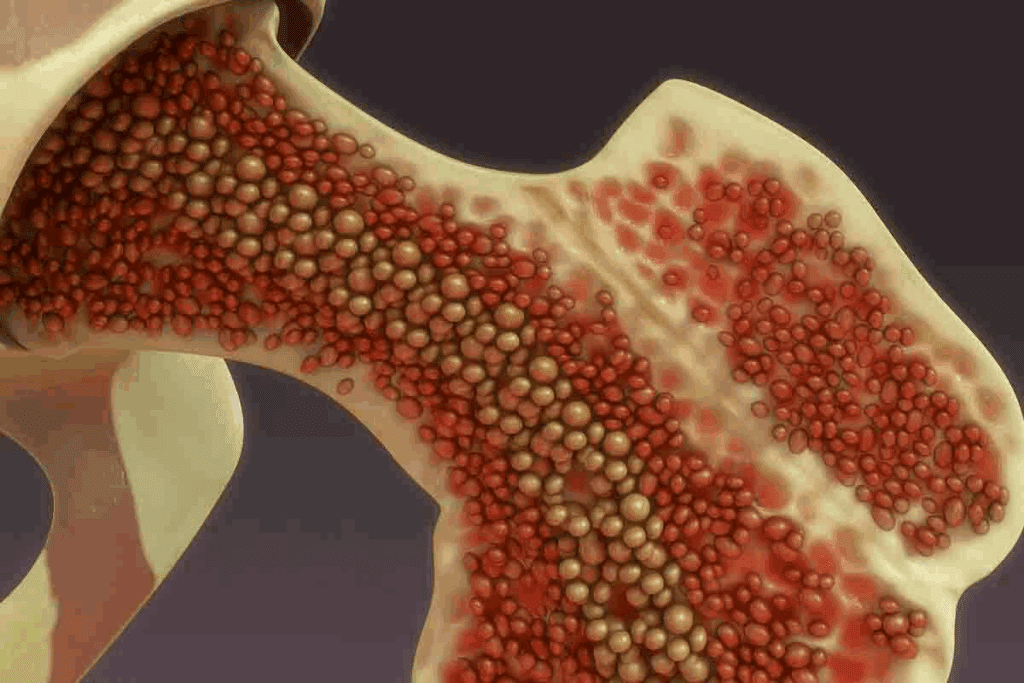
At LivHospital, we understand the complexities of bone marrow disorders and their significant impact on health. Bone marrow is a soft, gelatinous tissue that fills the hollow spaces within our bones. It is the primary site of haematopoiesis, the process of blood cell formation.
Disorders affecting the bone marrow can disrupt the production or function of blood cells, leading to various health issues. We guide you through the essential facts, types, and latest insights on major bone marrow conditions. This empowers you to make informed decisions about your health.
Key Takeaways
- Understanding bone marrow disorders is key for overall health.
- Bone marrow is responsible for blood cell formation.
- Disorders can disrupt blood cell production or function.
- LivHospital provides expert care for bone marrow-related diseases.
- Staying informed is key to managing bone marrow health.
Understanding Bone Marrow and Its Function

Bone marrow makes blood cells, which are key for carrying oxygen, fighting germs, and stopping bleeding. Knowing how bone marrow works helps us spot problems.
The Structure and Components of Bone Marrow
Bone marrow is a soft, spongy tissue inside bones. It has a network of blood vessels, like sinusoids, for exchanging nutrients and waste. It also has cells that make blood and others that support them.
How Bone Marrow Produces Blood Cells
The making of blood cells, or hematopoiesis, is complex. It starts with stem cells that turn into different blood cells. This process is controlled by growth factors and cytokines.
Signs of Healthy vs. Abnormal Bone Marrow
A healthy bone marrow makes the right amount of blood cells. But, problems can show up as anemia, infections, or bleeding issues. These signs mean the bone marrow isn’t working right.
What Are Bone Marrow Disorders?
Bone marrow disorders can cause too few or too many cells, affecting health. These conditions impact the marrow’s ability to make blood cells.
Definition and Classification Systems
Bone marrow disorders affect the marrow’s blood cell production. They are classified by cause and cell type. This helps in diagnosing and treating them.
The World Health Organization (WHO) classification is one system. It groups myeloid neoplasms and acute leukemia by features.
| Classification System | Description |
| WHO Classification | Categorizes myeloid neoplasms and acute leukemia based on morphological, immunophenotypic, genetic, and clinical features. |
| FAB Classification | An older system that categorizes acute myeloid leukemia (AML) based on the type of cell affected. |
Common Causes of Bone Marrow Abnormalities
Many factors can cause bone marrow problems. These include genetic mutations, toxin exposure, and infections. Knowing these causes helps in finding treatments.
- Genetic Mutations: Inherited or acquired genetic mutations can lead to bone marrow failure or proliferation disorders.
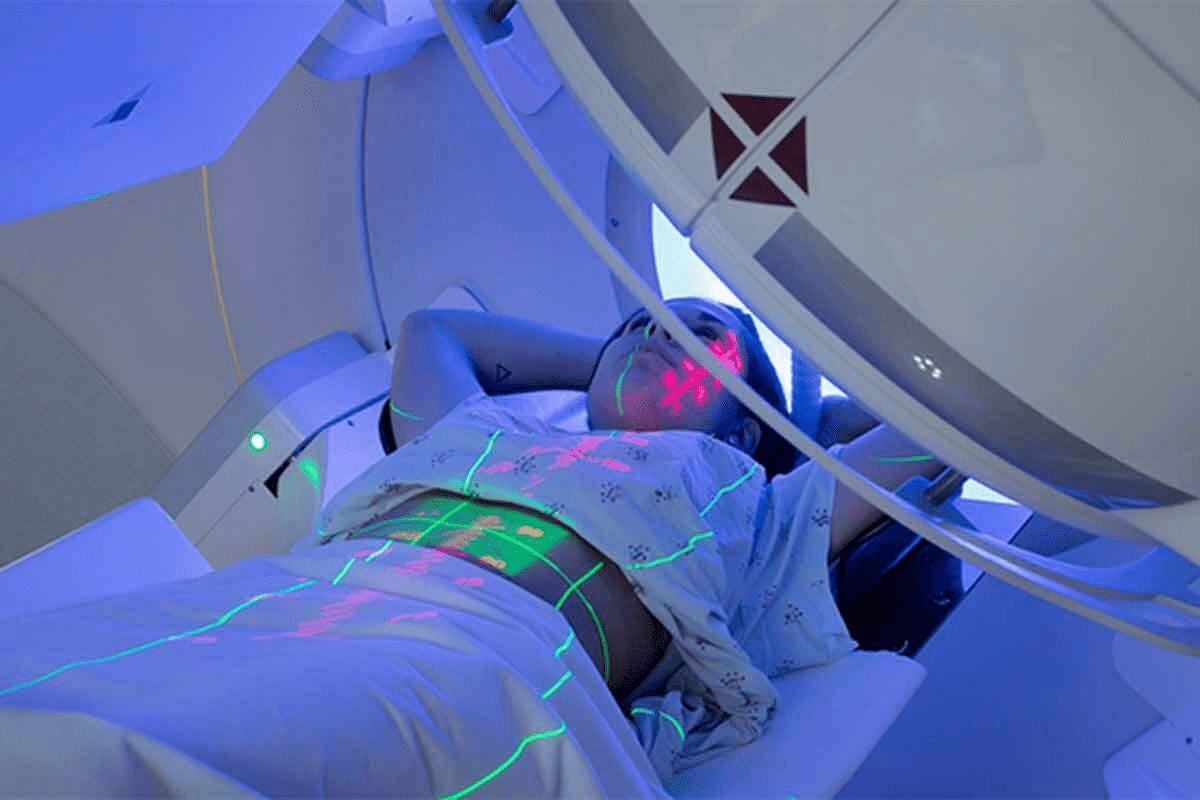
- Exposure to Toxins: Exposure to certain chemicals and radiation can damage the bone marrow, leading to abnormalities.
- Infections: Certain infections can affect the bone marrow, impairing its function.
Risk Factors and Genetic Predispositions
Some risk factors and genetic predispositions increase the chance of bone marrow disorders. Knowing these helps in early detection and prevention.
Genetic predispositions are key in some disorders. For example, inherited conditions like Fanconi anemia and Dyskeratosis congenita can cause bone marrow failure.
| Risk Factor | Description |
| Family History | A family history of bone marrow disorders can increase the risk. |
| Genetic Mutations | Inherited or acquired genetic mutations can predispose individuals to bone marrow disorders. |
| Exposure to Toxins | Prolonged exposure to certain chemicals and radiation can increase the risk. |
Aplastic Anemia: When Bone Marrow Fails
Aplastic anemia is a rare condition where the bone marrow doesn’t make enough blood cells. This can cause fatigue, infections, and severe bleeding. It’s a serious issue that can be life-threatening.
Mechanisms and Causes of Bone Marrow Failure
Bone marrow failure in aplastic anemia can happen for many reasons. These include toxins, some medicines, viral infections, and autoimmune disorders. Sometimes, the exact cause is not known, and it’s called idiopathic aplastic anemia.
Common causes include:
- Exposure to chemicals like pesticides and benzene
- Certain medications, such as antibiotics and anti-inflammatory drugs
- Viral infections, including hepatitis and HIV
- Autoimmune disorders, where the immune system attacks the bone marrow
Symptoms, Diagnosis, and Staging
Symptoms of aplastic anemia can vary. They include fatigue, shortness of breath, frequent infections, and easy bruising or bleeding. These symptoms depend on how severe the bone marrow failure is.
To diagnose, doctors do blood tests and a bone marrow biopsy. This helps figure out how severe the condition is. This information guides treatment choices.
“Early diagnosis is critical for effective management of aplastic anemia,” says why quick medical action is important.
Treatment Options and Long-term Outlook
Treatment for aplastic anemia depends on the severity and cause. It can range from blood transfusions to immunosuppressive therapy and bone marrow transplantation.
Treatment approaches include:
- Immunosuppressive therapy to stop the immune system from attacking the bone marrow
- Bone marrow transplantation to replace damaged marrow with healthy cells
- Supportive care, like blood transfusions and antibiotics, to manage symptoms and prevent complications
Thanks to new treatments, the outlook for aplastic anemia patients has improved. But, the outcome depends on how well the treatment works and any other health issues.
Acute Myeloid Leukemia (AML)
Acute Myeloid Leukemia (AML) is a serious blood cancer that starts in the bone marrow. It’s a type of bone marrow disorder that causes abnormal white blood cells. These cells grow fast and fill the bone marrow, stopping normal blood cell production.
Subtypes and Classification
AML is not just one disease but a group of disorders with different traits. The World Health Organization (WHO) classification is widely used. It sorts AML by genetic and molecular features, and by how cells look.
The French-American-British (FAB) classification also groups AML into subtypes. It looks at the cell type involved. Though the WHO system is now more common, FAB is useful for understanding AML’s variety.
Key Subtypes of AML:
- M0: Undifferentiated acute myeloid leukemia
- M1: Acute myeloblastic leukemia without maturation
- M2: Acute myeloblastic leukemia with maturation
- M3: Acute promyelocytic leukemia
- M4: Acute myelomonocytic leukemia
- M5: Acute monocytic leukemia
- M6: Acute erythroid leukemia
- M7: Acute megakaryoblastic leukemia
Clinical Presentation and Diagnostic Approach
AML symptoms vary by subtype, age, and health. Symptoms include tiredness, weight loss, infections, and easy bleeding or bruising. Doctors use blood tests, bone marrow biopsies, and imaging to diagnose.
Diagnosis often comes from a bone marrow exam. This shows the AML subtype and genetic details. Tests like cytogenetic analysis and molecular testing help plan treatment.
Treatment Strategies and Survival Rates
AML treatment is tough and often combines chemotherapy, targeted therapy, and bone marrow transplants. Treatment choices depend on age, health, and leukemia type.
Survival rates for AML have gotten better, thanks to new treatments and care. But, AML is hard to beat, mainly in older adults or those with certain genetic traits.
“The treatment of AML requires a multidisciplinary approach, involving hematologists, oncologists, and other healthcare professionals to provide the best possible outcomes for patients.” –
leading hematologist
Research keeps improving AML treatment. Knowing the disease, its subtypes, and best treatments is key to managing AML and boosting survival chances.
Acute Lymphoblastic Leukemia (ALL)
ALL is a serious disease that affects both kids and adults around the world. It happens when lymphoblasts grow too much in the bone marrow. This stops normal blood cells from being made.
Childhood vs. Adult ALL
ALL shows up differently in kids and adults. Childhood ALL is a common cancer in kids, hitting them between 2 and 5 years old. On the other hand, adult ALL is rarer but more aggressive and has a worse outlook.
Symptoms and Diagnostic Workup
Symptoms of ALL can be vague, like feeling tired, losing weight, and getting sick often. Doctors use blood tests, bone marrow samples, and special tests to find out if it’s ALL and what type.
This process is key to figuring out the leukemia’s details. It helps doctors decide the best treatment.
Modern Treatment Protocols and Outcomes
ALL treatments have changed a lot, with pediatric-inspired regimens now used for teens and young adults too. These include strong chemotherapy, targeted treatments, and sometimes bone marrow transplants.
Thanks to these advances, more people are getting better. Kids have a 90% chance of being cured, and adults have a 50% chance, depending on the type and other factors.
Chronic Myeloid Leukemia (CML)
The Philadelphia chromosome is a key sign of CML. It comes from a swap between chromosomes 9 and 22. This swap is key to understanding CML and finding new treatments.
The Philadelphia Chromosome and Disease Mechanism
CML is marked by the Philadelphia chromosome. This happens when chromosomes 9 and 22 swap places. This swap creates the BCR-ABL1 gene, which makes cells grow too much.
The BCR-ABL1 gene is a major cause of CML. It’s a target for treatments. The disease starts with cells that have this gene growing more than normal cells.
Phases of CML and Clinical Features
CML goes through three phases: chronic, accelerated, and blast. The chronic phase has few symptoms. But, the disease gets worse in the accelerated and blast phases, causing more symptoms.
Symptoms of CML vary by phase. Common ones include anemia, low platelets, and more infections. Watching the disease closely and acting fast is key to managing it.
Tyrosine Kinase Inhibitors and Treatment Response
Tyrosine kinase inhibitors (TKIs) have changed CML treatment. TKIs like imatinib, dasatinib, and nilotinib block the BCR-ABL1 gene. This stops cancer cells from growing. Many patients now live longer and have fewer symptoms.
Doctors check how well treatment is working by looking at BCR-ABL1 levels. A major molecular response is a big win, showing the disease is under control. The right TKI and treatment plan depend on each patient’s situation.
Myelodysplastic Syndromes (MDS)
Myelodysplastic syndromes (MDS) are complex disorders where the bone marrow fails to make healthy blood cells. This failure leads to various blood cell shortages.
Classification and Risk Stratification
MDS is classified by the World Health Organization (WHO) criteria. These criteria look at the bone marrow’s blast count, genetic abnormalities, and affected cell lines.
The International Prognostic Scoring System (IPSS) helps predict patient outcomes. It guides treatment choices.
Clinical Manifestations and Diagnostic Criteria
Patients with MDS often have symptoms like anemia, infections, and bleeding. These symptoms come from blood cell shortages.
Diagnosis involves clinical findings, blood counts, bone marrow biopsy, and cytogenetic analysis. These steps help confirm the diagnosis.
Treatment Approaches Based on Risk Category
Treatment for MDS depends on the patient’s risk category. Lower-risk patients get supportive care. Higher-risk patients may need more aggressive treatments like stem cell transplantation.
Supportive care includes blood transfusions and growth factors. These help manage blood cell shortages. Higher-risk patients get treatments aimed at changing the disease’s course.
Bone Marrow Conditions Types: Myeloproliferative Neoplasms
Myeloproliferative neoplasms are rare blood cancers. They cause too many blood cells to be made. This can lead to serious problems. We’ll look at three main types: polycythemia vera, essential thrombocythemia, and primary myelofibrosis.
Polycythemia Vera: Causes and Management
Polycythemia vera makes too many red blood cells. This raises the risk of blood clots and heart problems. It’s linked to a JAK2 gene mutation. To manage it, doctors take blood to lower red cell counts and use medicines to stop clots.
Essential Thrombocythemia: Diagnosis and Treatment
Essential thrombocythemia makes too many platelets. This can cause bleeding or clotting. Doctors use blood tests and bone marrow biopsies to diagnose it. Treatment includes medicines to lower platelet counts and prevent clots, along with regular check-ups.
Primary Myelofibrosis: Progression and Therapy
Primary myelofibrosis scars the bone marrow. This can cause anemia, fatigue, and other issues. Its progression varies, and treatments range from symptom management to stem cell transplants in severe cases.
In summary, myeloproliferative neoplasms are complex disorders needing careful management. Understanding polycythemia vera, essential thrombocythemia, and primary myelofibrosis helps support those affected.
Multiple Myeloma: Cancer of Plasma Cells
The bone marrow is affected by multiple myeloma, a cancer that starts in plasma cells. This cancer makes the bone marrow fill up with bad plasma cells. This causes many problems.
Pathophysiology and Disease Manifestations
Multiple myeloma is a complex disease. It involves bad plasma cells and the bone marrow. These cells can damage bones, cause anemia, and make infections more likely.
We will look at how the disease shows up. Symptoms include bone pain, tiredness, and infections that keep coming back. Knowing how it works helps us find better treatments.
Diagnostic Criteria and Staging Systems
To diagnose multiple myeloma, doctors use tests and scans. They look for certain proteins in the blood or urine, check the bone marrow, and see if organs are damaged.
There are different ways to stage multiple myeloma, like the International Staging System (ISS). Staging helps doctors know how serious the disease is and what treatment to use.
| Stage | Characteristics | Median Survival |
| I | Low levels of beta-2 microglobulin and albumin | 62 months |
| II | Intermediate levels of beta-2 microglobulin and albumin | 44 months |
| III | High levels of beta-2 microglobulin | 29 months |
Current Treatment Paradigms and Novel Therapies
Treatment for multiple myeloma has changed a lot. New drugs like proteasome inhibitors and monoclonal antibodies are being used. We will talk about these new treatments.
New treatments give hope to those with multiple myeloma. We’re seeing progress with CAR-T cell therapy and other immunotherapies in trials.
Inherited Bone Marrow Failure Syndromes
Inherited bone marrow failure syndromes are a group of genetic conditions. They affect the bone marrow’s ability to make blood cells. This leads to various health problems.
Genetics and Clinical Features of Fanconi Anemia
Fanconi anemia is a rare genetic disorder. It makes it hard for the body to make new blood cells. This results in bone marrow failure.
Key Features of Fanconi Anemia:
- Congenital abnormalities
- Increased risk of cancer
- Bone marrow failure
Pathogenesis and Management of Diamond-Blackfan Anemia
Diamond-Blackfan anemia affects the production of red blood cells. It is often found in infants or young children.
Management Strategies:
- Corticosteroid therapy
- Blood transfusions
- Bone marrow transplantation
Shwachman-Diamond Syndrome and Dyskeratosis Congenita
Shwachman-Diamond syndrome is a rare disorder. It affects the pancreas, bone marrow, and bones. Dyskeratosis congenita has a unique set of symptoms.
Both conditions show how complex and varied inherited bone marrow failure syndromes can be.
It’s important to understand these syndromes. This helps in creating effective treatment plans.
| Syndrome | Key Characteristics | Management Approaches |
| Fanconi Anemia | Congenital abnormalities, cancer susceptibility, bone marrow failure | Bone marrow transplantation, supportive care |
| Diamond-Blackfan Anemia | Red blood cell production failure | Corticosteroids, blood transfusions, bone marrow transplantation |
| Shwachman-Diamond Syndrome | Pancreatic insufficiency, bone marrow dysfunction, skeletal abnormalities | Pancreatic enzyme replacement, supportive care for bone marrow failure |
Bone Marrow Infiltrative and Rare Disorders
Rare bone marrow disorders are tough to diagnose and treat. They can mess up the bone marrow’s job of making blood cells. This leads to serious health issues. We’ll look at what these disorders are, how to find them, and how to manage them.
Metastatic Cancer to Bone Marrow
When cancer spreads to the bone marrow, it’s called metastatic cancer. This can cause the marrow to fail, leading to anemia, infections, and bleeding problems. Cancers like breast, prostate, and lung often spread to the bone marrow. Doctors use bone marrow biopsies to diagnose it. Treatment aims to control the cancer.
Myelofibrosis: Primary and Secondary Forms
Myelofibrosis scars the bone marrow, causing anemia and spleen growth. It can start on its own or after other blood diseases. Primary myelofibrosis is rare. Doctors try to ease symptoms and improve life quality.
Hemophagocytic Lymphohistiocytosis (HLH)
HLH is a rare, serious condition with too much inflammation and histiocytes in organs like the bone marrow. It can be genetic or caused by infections, cancers, or autoimmune diseases. Quick diagnosis and treatment are key.
Mastocytosis and Other Rare Conditions
Mastocytosis is when mast cells build up in tissues, including the bone marrow. It can cause mild to severe symptoms. Other rare bone marrow issues include histiocytic disorders and storage diseases.
Conclusion: Advances in Bone Marrow Disease Treatment
Understanding bone marrow conditions is key to better treatments. This article has covered different bone marrow disorders and their effects on patients. Thanks to new diagnosis and treatment methods, patients are seeing better results.
Recently, there have been big steps forward in treating bone marrow diseases. New therapies and better ways to diagnose have helped. For example, treatments for acute myeloid leukemia and multiple myeloma are now more effective. This has improved survival rates and the quality of life for patients.
It’s important to keep researching and investing in bone marrow disease treatment. New technologies and treatments will help tackle the challenges of these diseases. By staying updated, we can offer the best care to those affected by these conditions.
FAQ
What are bone marrow disorders?
Bone marrow disorders are conditions that affect the bone marrow’s ability to make healthy blood cells. These issues can cause anemia, infections, and bleeding problems.
What is the difference between healthy and abnormal bone marrow?
Healthy bone marrow makes a balanced mix of blood cells. Abnormal bone marrow might make too few or too many cells. Or, it might make cells that don’t work right.
What are the symptoms of bone marrow disorders?
Symptoms vary by condition but often include fatigue, weakness, and pale skin. You might also get infections easily or bruise or bleed a lot.
What is aplastic anemia?
Aplastic anemia is when the bone marrow can’t make enough blood cells. This leads to anemia, infections, and bleeding issues.
What is acute myeloid leukemia (AML)?
AML is a cancer that stops the bone marrow from making healthy blood cells. It’s marked by fast-growing, abnormal white blood cells in the bone marrow.
What is the difference between acute lymphoblastic leukemia (ALL) in children and adults?
ALL symptoms and tests are similar for kids and adults. But, treatment and outcomes differ. Kids usually have a better chance of recovery than adults.
What is chronic myeloid leukemia (CML)?
CML is a cancer that affects the bone marrow’s blood cell production. It’s marked by the Philadelphia chromosome, causing too many white blood cells.
What are myelodysplastic syndromes (MDS)?
MDS are conditions where the bone marrow can’t make healthy blood cells. They can turn into AML in some cases.
What are myeloproliferative neoplasms?
Myeloproliferative neoplasms are conditions where the bone marrow makes too many blood cells. Examples include polycythemia vera and essential thrombocythemia.
What is multiple myeloma?
Multiple myeloma is a cancer that affects plasma cells in the bone marrow. It can cause anemia, bone pain, and increase infection risk.
What are inherited bone marrow failure syndromes?
Inherited bone marrow failure syndromes are rare genetic disorders. They affect the bone marrow’s ability to make healthy blood cells. Examples include Fanconi anemia and Diamond-Blackfan anemia.
What is bone marrow infiltrative disease?
Bone marrow infiltrative disease is when abnormal cells or tissues invade the bone marrow. This disrupts its ability to make healthy blood cells. Examples include metastatic cancer and myelofibrosis.
What are the treatment options for bone marrow disorders?
Treatment for bone marrow disorders depends on the condition. It may include medications, blood transfusions, bone marrow transplants, or other therapies.
References
- DeZern, A. E., & Churpek, J. E. (2021). Approach to the diagnosis of aplastic anemia. Blood Advances, *5*(12), 2660–2671. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8233215/