Last Updated on November 17, 2025 by Ugurkan Demir

At LivHospital, we know that bone marrow disorders can really affect your health. They can mess with how your body makes blood cells, leading to serious problems.
Bone marrow disease is a group of conditions that harm the spongy tissue inside bones. This tissue is key for making blood cells. If not treated right away, these diseases can be very dangerous.
We get how complex bone marrow abnormalities can be. That’s why we offer top-notch, team-based care. Our goal is to give you the best treatment possible, based on the latest research, to help you get better.
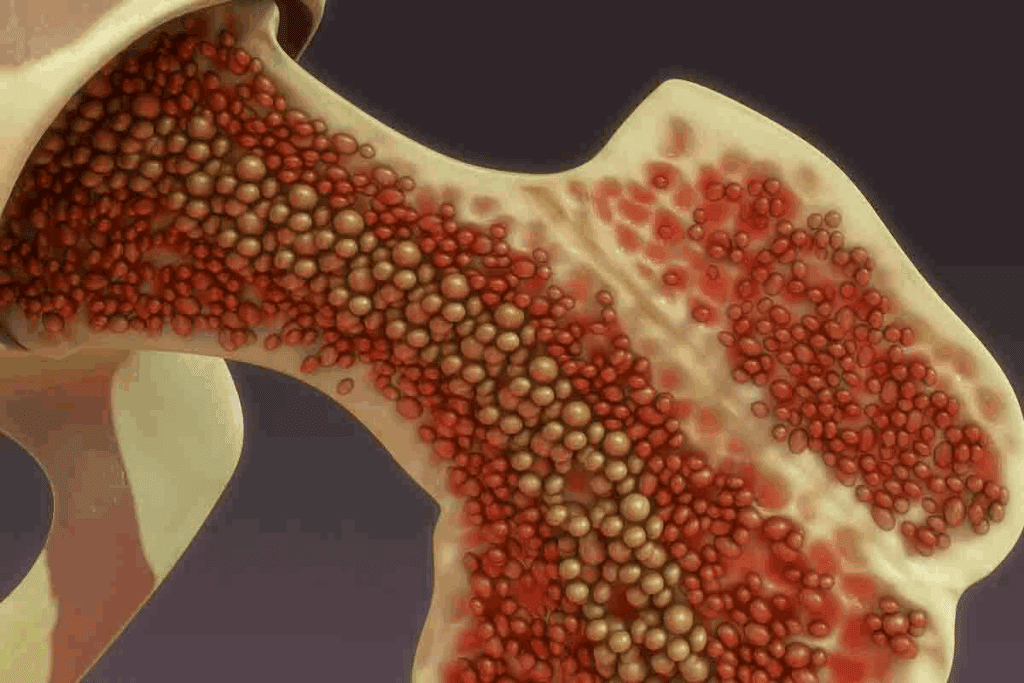
Bone marrow is a key part of our body, found inside our bones. It makes red blood cells, white blood cells, and platelets. These cells are vital for our health.
Bone marrow is more than just tissue; it’s a vital organ. It has blood vessels that bring nutrients and oxygen. The health of our bone marrow is linked to our overall well-being. It produces cells that carry oxygen, fight infections, and stop bleeding.
In a healthy person, bone marrow makes the right amount of blood cells. It works with stem cells, progenitor cells, and mature blood cells. This ensures the body has the right balance of cells. This balance is key to staying healthy and avoiding disease.
Stem cells are the base of blood cell production in bone marrow. They can turn into different cell types, like red and white blood cells, and platelets. Understanding stem cells helps us see how bone marrow problems can affect our health.
Knowing how bone marrow works helps us understand bone marrow diseases better. It shows the importance of stem cells in making blood cells. This knowledge highlights the health impact of bone marrow conditions.

Bone marrow disease refers to conditions that harm the bone marrow’s ability to make healthy blood cells. These diseases can be caused by genetics or acquired, leading to serious health issues.
Bone marrow disease happens when the bone marrow can’t work right. It affects its ability to make blood cells. There are many types, including:
Knowing these types is key to finding and treating bone marrow diseases well.
The symptoms of bone marrow disease vary by condition. But, some common ones are:
Spotting these symptoms early can help get a diagnosis and treatment sooner.
Some things can make you more likely to get bone marrow disorders. These include:
| Risk Factor | Description |
| Genetic predisposition | Family history of bone marrow disorders |
| Exposure to toxins | Chemicals, pesticides, and heavy metals |
| Previous chemotherapy or radiation | Treatment for cancer or other conditions |
Knowing these risk factors can help catch and prevent bone marrow diseases early.
Leukemia is a term for several cancers affecting the blood and bone marrow. It’s caused by abnormal white blood cells growing out of control. These cells are key for fighting off infections. Leukemia is divided based on how fast it grows and the type of blood cells it affects.
Leukemia is mainly split into acute and chronic types. Acute leukemia grows fast and needs quick treatment. Chronic leukemia grows slower, sometimes allowing for a watchful waiting period before treatment starts.
“The difference between acute and chronic leukemia is key for picking the right treatment,” doctors say. Acute leukemia has more immature cells, while chronic leukemia has more mature cells.
Leukemia is also classified by the blood cells it affects: myeloid or lymphocytic. Myeloid leukemia impacts cells that make red blood cells, platelets, and some white blood cells. Lymphocytic leukemia affects lymphocytes, which are important for the immune system.
Leukemia symptoms can vary but often include tiredness, weight loss, frequent infections, and easy bruising or bleeding. Doctors use blood tests and bone marrow biopsies to find and identify abnormal cells and the leukemia type.
Treatment for leukemia depends on the type and the patient’s health. Options include chemotherapy, targeted therapy, radiation, or bone marrow transplantation. “New treatments have greatly improved care for leukemia patients, making it more personalized and effective,” research shows.
Myelodysplastic syndromes (MDS) are complex disorders where the bone marrow fails to make healthy blood cells. This failure leads to anemia, neutropenia, and thrombocytopenia. It affects how well the body can make blood.
MDS is divided into subtypes based on certain features and genetic changes. The World Health Organization (WHO) system is used to classify MDS. This helps doctors understand the disease better.
Knowing the subtype is key to figuring out the prognosis and treatment plan.
Several factors can lead to MDS, like chemicals, radiation, and chemotherapy. Genetics also play a role. The disease can progress slowly or quickly, sometimes turning into AML.
A study in the Journal of Clinical Oncology found that MDS can turn into AML. This is a major concern for patients.
“The International Prognostic Scoring System (IPSS) is a widely used tool to predict the risk of disease progression and AML transformation in MDS patients.”
To diagnose MDS, doctors use bone marrow biopsies, genetic tests, and blood counts. Treatment depends on the subtype, risk level, and patient’s health.
| Treatment Approach | Description | Applicability |
| Supportive Care | Includes blood transfusions and growth factors to manage symptoms | All MDS patients |
| Immunosuppressive Therapy | Targets the immune system to improve blood counts | Selected patients with specific HLA types |
| Hypomethylating Agents | Medications that can help improve blood counts and delay disease progression | Higher-risk MDS patients |
Emerging treatments like new hypomethylating agents and targeted therapies offer hope for better outcomes in MDS patients.
Aplastic anemia happens when the bone marrow stops working right. This leads to a big drop in blood cell production. This includes red blood cells, white blood cells, and platelets. It can come from either getting it or being born with it, affecting people differently.
Aplastic anemia falls into two types: acquired and inherited. Acquired aplastic anemia is more common. It can be caused by toxins, some medicines, viruses, or autoimmune diseases. Inherited aplastic anemia, on the other hand, is linked to genetic mutations, like in Fanconi anemia.
The main signs of aplastic anemia are due to a lack of blood cells. People might feel tired, get sick easily, and bleed a lot. These problems can be very serious and even life-threatening.
Treatment for aplastic anemia depends on how bad it is and why it happened. Doctors might use medicines to calm down the immune system, bone marrow transplants, or just give blood transfusions. How well someone does varies; some get better, while others need ongoing care.
Immunosuppressive therapy can help by stopping the immune system from attacking the bone marrow.
Thanks to new treatments, the outlook for aplastic anemia is better. Catching it early and treating it right is key to managing it well.
Myeloproliferative neoplasms are a group of blood disorders. They cause too many blood cells to be made. This happens because a blood cell stem cell mutates, leading to more blood cells than needed.
We’ll look at three main types: polycythemia vera, essential thrombocythemia, and primary myelofibrosis. Each has its own signs and health effects.
Polycythemia vera makes too many red and white blood cells and platelets. This raises the risk of blood clots and other problems.
Symptoms include headaches, dizziness, and itching after bathing. To manage it, doctors might use phlebotomy or medicine to lower blood cell counts.
Key Features of Polycythemia Vera:
Essential thrombocythemia is when platelets are made too much. It can cause blood clots and bleeding.
People might not show symptoms or have headaches, fatigue, or bleeding. Doctors use medicine to lower platelet counts and prevent blood clots.
“The management of essential thrombocythemia focuses on preventing thrombotic complications while minimizing the risk of bleeding.” – Hematology Expert
Primary myelofibrosis is a serious condition. The bone marrow gets fibrotic, making blood cell production poor. This leads to anemia, big spleens, and other issues.
| Disease Characteristics | Polycythemia Vera | Essential Thrombocythemia | Primary Myelofibrosis |
| Primary Feature | Too many red blood cells | Too many platelets | Bone marrow fibrosis |
| Common Complications | Blood clots | Blood clots, bleeding | Anemia, big spleen |
Knowing the differences and complications of these diseases is key to good care. We’re always working to improve diagnosis and treatment, aiming for better patient outcomes.
Plasma cell cancer, also known as multiple myeloma, is a blood cancer. It affects the bone marrow. This happens when plasma cells, which make antibodies, turn cancerous.
Multiple myeloma makes the bone marrow fill with cancerous plasma cells. This pushes out healthy cells. It can damage bones, cause anemia, and make infections more likely.
The disease grows at different rates for everyone. Some may see it grow slowly, while others may face a fast-moving disease. Knowing how multiple myeloma works is key to finding good treatments.
Symptoms of multiple myeloma include bone pain, tiredness, and frequent infections. As it gets worse, it can lead to high calcium levels, kidney damage, and anemia.
Common problems with multiple myeloma include:
Treatment for multiple myeloma has improved a lot. Now, there are targeted therapies, immunotherapies, and stem cell transplants.
New treatments target specific parts of the cancer. These include proteasome inhibitors, immunomodulatory drugs, and monoclonal antibodies. They have made treatments better for patients.
Doctors create treatment plans that fit each person. They consider the disease stage, the patient’s health, and the cancer’s genetics.
Inherited bone marrow disorders are rare but serious. They affect the marrow’s ability to make healthy blood cells. This leads to various health problems.
We will look at several inherited bone marrow disorders. These include Fanconi anemia, Diamond-Blackfan anemia, Shwachman-Diamond syndrome, and dyskeratosis congenita. We will discuss their causes, symptoms, and how to manage them.
Fanconi anemia is a rare genetic disorder. It causes bone marrow failure, birth defects, and a higher risk of cancer. It happens because of DNA repair gene mutations.
Clinical Features: People with Fanconi anemia often have aplastic anemia, birth defects, and are more likely to get infections and cancers.
Management: Treatment includes bone marrow transplants, supportive care, and watching for cancer.
Diamond-Blackfan anemia is a rare disorder that affects red blood cell production. It is linked to physical anomalies and a higher risk of cancer.
Causes: It is caused by mutations in genes that make ribosomal proteins.
Clinical Features: Symptoms include anemia, low reticulocyte count, and sometimes physical malformations.
Management: Treatment includes steroids, blood transfusions, and sometimes bone marrow transplants.
Shwachman-Diamond syndrome is a rare genetic disorder. It affects the pancreas, bone marrow, and bones.
Clinical Features: Symptoms include low white blood cell count, anemia, and infections. It also affects the pancreas.
Management: Treatment includes pancreatic enzyme replacement, antibiotics, and sometimes bone marrow transplants.
Dyskeratosis congenita is a rare genetic disorder. It causes skin, nail, and mouth changes, bone marrow failure, and a higher risk of cancer.
Causes: It is caused by mutations in genes that affect telomere maintenance.
Clinical Features: Symptoms include aplastic anemia, skin, nail, and mouth changes, and other systemic issues.
Management: Treatment includes bone marrow transplants, supportive care, and cancer monitoring.
| Disorder | Primary Features | Management Strategies |
| Fanconi Anemia | Bone marrow failure, congenital anomalies, cancer risk | Hematopoietic stem cell transplantation, supportive care |
| Diamond-Blackfan Anemia | Red cell aplasia, physical anomalies | Corticosteroids, red blood cell transfusions, hematopoietic stem cell transplantation |
| Shwachman-Diamond Syndrome | Pancreatic insufficiency, bone marrow dysfunction, skeletal abnormalities | Pancreatic enzyme replacement, antibiotics, hematopoietic stem cell transplantation |
| Dyskeratosis Congenita | Mucocutaneous features, bone marrow failure, cancer risk | Hematopoietic stem cell transplantation, supportive care |
Understanding how to diagnose and treat bone marrow issues is key. Accurate diagnosis is the first step to effective treatment. It combines clinical checks, lab tests, and sometimes, imaging.
Bone marrow aspiration and biopsy are key tests for diagnosing issues. Bone marrow aspiration takes a sample of the liquid part. Bone marrow biopsy takes a sample of bone and marrow. These tests help find problems like leukemia and lymphoma.
First, the patient gets local anesthesia. Then, a needle is inserted into the bone marrow, usually in the hip. The sample is checked for abnormal cells or disease signs.
Genetic and molecular tests are vital for diagnosing bone marrow disorders. They find specific genetic mutations or abnormalities. This helps diagnose conditions like myeloproliferative neoplasms.
Common tests include:
Bone marrow transplantation is a treatment for many disorders, like leukemia. It replaces the diseased bone marrow with healthy stem cells. These can be from the patient or a donor.
The goal is to restore bone marrow function. But, it comes with risks like graft-versus-host disease (GVHD).
New treatments and clinical trials offer hope for bone marrow disorder patients. These include targeted therapies, immunotherapies, and gene therapies. They aim to attack cancer cells or correct genetic defects.
Joining clinical trials can give patients access to new treatments. It’s important to talk about the benefits and risks with a healthcare provider.
Living with bone marrow disorders can be tough. It needs a full plan to manage it well. This plan includes medical care, lifestyle changes, and ongoing support.
People with bone marrow illnesses must team up with their doctors. Together, they create a care plan that fits the patient’s needs. This plan includes regular check-ups, treatments, and support services.
Good management of bone marrow diseases helps patients live active lives. We stress the need for a team of doctors to support patients fully. This team helps a lot.
We aim to help patients manage their condition better. Our goal is to improve their life quality. We offer top-notch healthcare to those dealing with bone marrow disorders.
Bone marrow disease is a group of conditions that affect the bone marrow. This part of the body is key for making healthy blood cells. Problems here can cause anemia, infections, and bleeding issues.
There are many types of bone marrow diseases. These include leukemia, myelodysplastic syndromes, aplastic anemia, myeloproliferative neoplasms, and multiple myeloma. Each type affects the body differently.
Symptoms vary by disease. Common signs are fatigue, weakness, and pale skin. You might also feel short of breath or get infections easily. Some diseases cause bone pain, weight loss, or night sweats.
Doctors use tests to diagnose bone marrow disease. These include bone marrow aspiration and biopsy, blood tests, and genetic testing. These help find the right treatment.
Stem cells in the bone marrow are vital. They help make red blood cells, white blood cells, and platelets. These cells keep blood counts healthy and prevent anemia and infections.
Myelodysplastic syndromes (MDS) are disorders of the bone marrow. They lead to poor blood cell production. MDS can turn into more serious conditions like leukemia.
Aplastic anemia is when the bone marrow can’t make enough blood cells. This causes anemia, infections, and bleeding problems. It’s important to get medical help quickly.
Myeloproliferative neoplasms are conditions where the bone marrow makes too many blood cells. These include polycythemia vera, essential thrombocythemia, and primary myelofibrosis.
Multiple myeloma is a cancer that affects plasma cells in the bone marrow. It leads to too much of an abnormal protein, causing bone damage, anemia, and kidney issues.
Treatments vary by disease. They can include medicines, blood transfusions, bone marrow transplants, and other therapies. New treatments and clinical trials are also being explored.
Yes, some bone marrow diseases can be inherited. Conditions like Fanconi anemia and Diamond-Blackfan anemia are caused by genetic mutations. They can be passed down from parents to children.
The outlook varies by disease and treatment. With proper care, many people with bone marrow diseases can live active and fulfilling lives.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!