Last Updated on November 17, 2025 by Ugurkan Demir
At LivHospital, we understand the complexities of bone marrow disorders and their impact on patients’ lives. These bone marrow issues affect blood cell production and bone marrow function. This leads to various health problems that require specialized diagnosis and treatment approaches to improve patient outcomes and quality of life.
Bone marrow disorders can be inherited or acquired. They include both benign and malignant diseases. It’s important to know about these conditions for early detection and treatment. This way, patients can get the care they need.
We offer a detailed guide to 12 key bone marrow diseases. It covers their symptoms and treatment options. Our patient-centered approach ensures patients get the best care and latest therapies for these tough conditions.
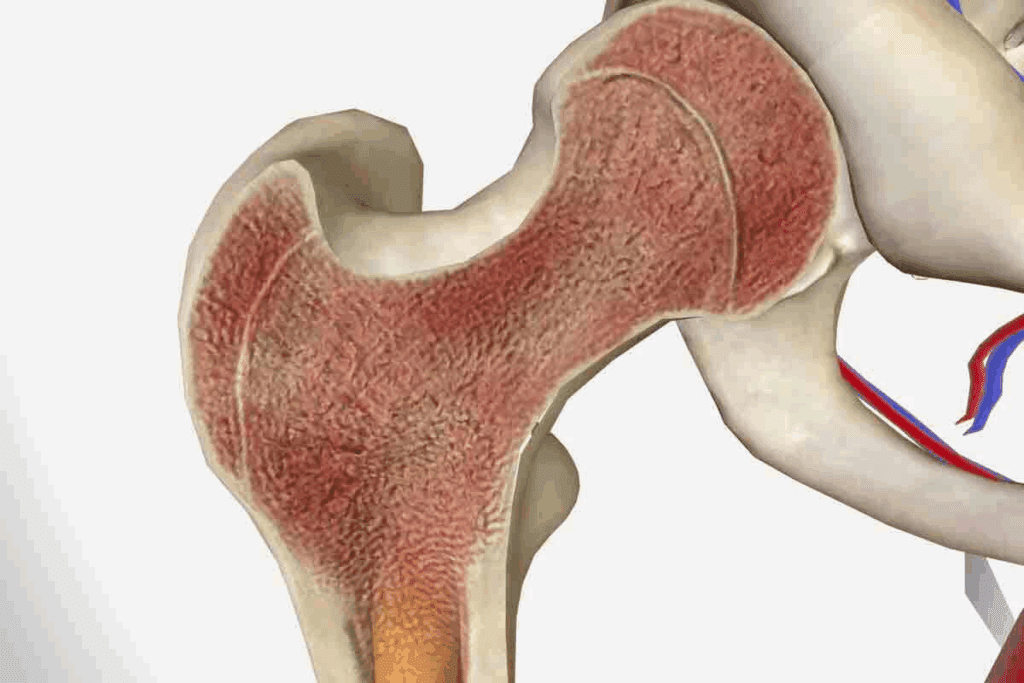
Deep inside our bones, there’s a soft, fatty tissue called bone marrow. It’s key to our survival. Bone marrow makes blood cells, which carry oxygen, fight infections, and stop bleeding.
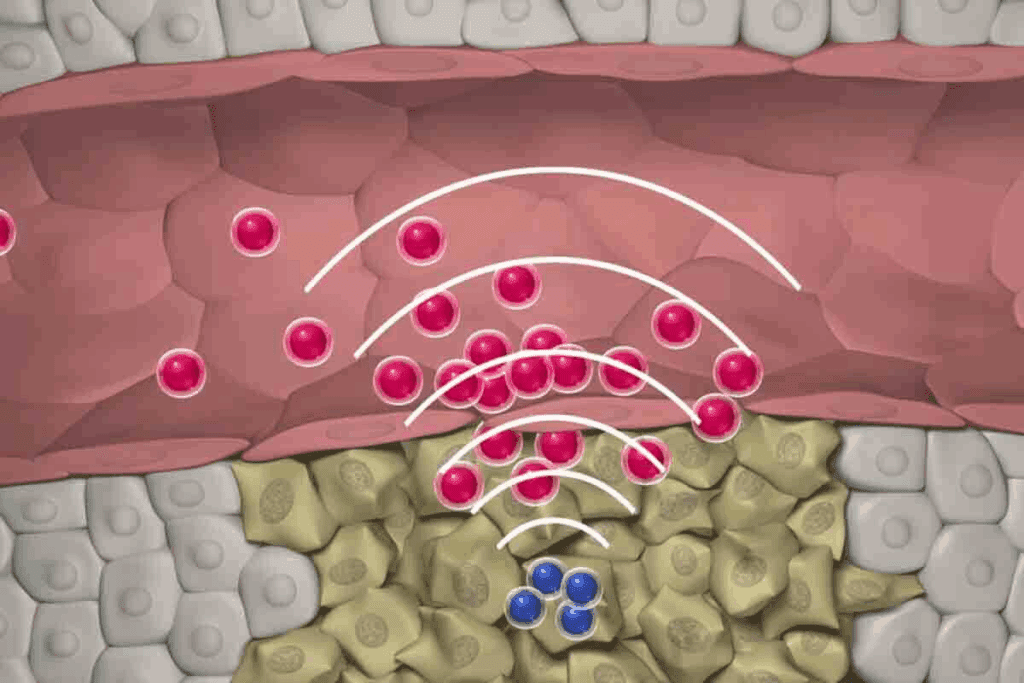
Bone marrow makes blood cells through a process called hematopoiesis. It turns stem cells into different blood cells. Understanding bone marrow’s role in blood production is vital for our health.
Every day, bone marrow produces millions of blood cells. This keeps our blood healthy and prevents problems like anemia and bleeding disorders.
Bone marrow makes three main blood cell types: red blood cells, white blood cells, and platelets. Each type is essential for our health.
| Type of Blood Cell | Function |
| Red Blood Cells | Carry oxygen to the body’s tissues and organs |
| White Blood Cells | Fight infections and diseases |
| Platelets | Help to stop bleeding by forming blood clots |
Bone marrow is vital for making the cells that keep us alive. Its role is too important to ignore. Knowing how it works helps us understand the effects of bone marrow disorders.

Bone marrow problems can come from many sources, affecting our health. Disorders in the bone marrow can lead to serious issues if not treated quickly.
Bone marrow disorders can start from genetic changes, environmental factors, or other diseases. Exposure to harmful chemicals or radiation can harm the bone marrow. Genetic factors also play a big role.
These disorders are complex, caused by both genetics and environment. Knowing this helps us create better treatment plans.
The symptoms of bone marrow disorders vary but often include fatigue, frequent infections, and easy bruising. Spotting these signs early is key to managing the condition.
Common symptoms include:
Being aware of these symptoms is important. Seeking medical help early can greatly improve treatment results for bone marrow disorders.
| Symptom | Description |
| Fatigue | Persistent feeling of tiredness or weakness |
| Frequent Infections | Recurring infections due to a weakened immune system |
| Easy Bruising | Bruising or bleeding easily due to low platelet count |
Bone marrow failure syndromes are conditions where the bone marrow can’t make enough blood cells. This can cause serious health problems like anemia, infections, and bleeding disorders.
We will look at two main bone marrow failure syndromes: aplastic anemia and Fanconi anemia. Both show how complex and challenging bone marrow issues can be.
Aplastic anemia is when the bone marrow can’t make new blood cells. This leads to fatigue, infections, and uncontrolled bleeding. It can be caused by toxins, certain medicines, and viral infections.
The symptoms of aplastic anemia are severe. They include:
Treatment for aplastic anemia aims to fix the cause. It may involve immunosuppressive therapy or bone marrow transplantation.
Fanconi anemia is a rare genetic disorder that affects blood cell production. It’s marked by congenital abnormalities and a higher cancer risk. Symptoms are similar to aplastic anemia, like anemia, infections, and bleeding.
Diagnosing Fanconi anemia involves genetic tests to find specific gene mutations. Treatment is mostly about managing symptoms and complications.
Key aspects of Fanconi anemia include:
Managing bone marrow failure syndromes like aplastic anemia and Fanconi anemia needs a detailed approach. This includes early diagnosis, proper treatment, and ongoing care.
Leukemia is a cancer that affects the bone marrow. It causes too many immature white blood cells to be made. These cells can’t fight infections well. We’ll look at the different types of leukemia, like Acute Myeloid Leukemia (AML), Acute Lymphoblastic Leukemia (ALL), Chronic Myeloid Leukemia (CML), and Chronic Lymphocytic Leukemia (CLL).
Acute Myeloid Leukemia (AML) is a fast-growing cancer. It starts in the bone marrow and quickly spreads to the blood. It can also go to other parts of the body, like the lymph nodes and liver.
AML makes too many abnormal cells. These cells fill the bone marrow and stop normal blood cells from being made.
Acute Lymphoblastic Leukemia (ALL) grows fast if not treated. It makes too many immature lymphocytes, a type of white blood cell. ALL is most common in kids but can also happen in adults.
The symptoms and treatment for ALL depend on the patient’s age and other factors.
Chronic Myeloid Leukemia (CML) starts in the bone marrow. It grows slowly, making it easier to treat than acute leukemia.
Chronic Lymphocytic Leukemia (CLL) is a slow-growing cancer. It affects the blood and bone marrow. CLL makes too many mature lymphocytes.
It’s more common in older adults. Treatment depends on the stage and symptoms.
| Type of Leukemia | Characteristics | Commonly Affected Population |
| Acute Myeloid Leukemia (AML) | Rapidly progressing, abnormal myeloid cells | Adults, can occur in children |
| Acute Lymphoblastic Leukemia (ALL) | Rapid progression, immature lymphocytes | Children, can occur in adults |
| Chronic Myeloid Leukemia (CML) | Slow progression, mature myeloid cells | Mainly adults |
| Chronic Lymphocytic Leukemia (CLL) | Slow progression, mature lymphocytes | Older adults |
Myelodysplastic syndromes (MDS) are a group of disorders that affect the bone marrow. They make it hard for the bone marrow to produce healthy blood cells. The severity of MDS can vary a lot, affecting patients differently.
These conditions cause the bone marrow to make abnormal blood cells. This can lead to problems like anemia, infections, and bleeding disorders. Knowing about MDS is key to managing and treating it effectively.
MDS has several subtypes, each with its own characteristics. The World Health Organization (WHO) classification system helps categorize MDS. It looks at factors like the number of cell lines affected and the presence of ring sideroblasts.
Several factors can increase the risk of getting MDS. These include exposure to chemicals like benzene, radiation, and previous chemotherapy or radiation therapy. Genetic mutations also play a big role in MDS development.
The prognosis for MDS patients varies a lot. It depends on the subtype of MDS, the number of blasts in the bone marrow, and genetic mutations. The Revised International Prognostic Scoring System (IPSS-R) helps predict prognosis and guide treatment.
“The prognosis and treatment of MDS have evolved significantly, giving new hope to patients with these complex disorders.”
Expert Opinion
Understanding risk factors and prognostic indicators is vital. It helps healthcare providers create effective treatment plans for each patient.
Myeloproliferative neoplasms are blood disorders where the bone marrow makes too many blood cells. This can cause serious health problems, like blood clots and leukemia.
There are different types of these disorders, each with its own signs and effects on health. The main ones are polycythemia vera, essential thrombocythemia, primary myelofibrosis, and chronic neutrophilic leukemia.
Polycythemia vera makes too many red blood cells. This makes blood thick, raising the risk of blood clots. Symptoms include headaches, dizziness, and itching, often after hot showers. Doctors treat it with blood removal and medicines to prevent clots.
Essential thrombocythemia makes too many platelets, raising the risk of blood clots. Symptoms include headaches, dizziness, or a burning feeling in the hands and feet. Treatment aims to lower platelet counts and prevent clots with medicines.
Primary myelofibrosis replaces bone marrow with fibrous tissue. This causes anemia, spleen enlargement, and other issues. Symptoms include fatigue, night sweats, and bone pain. Treatment may include medicines and, in some cases, bone marrow transplant.
Chronic neutrophilic leukemia is a rare disorder with high neutrophil counts. Diagnosis rules out other causes of high neutrophils, and treatment aims to control counts with medicines.
It’s important to understand these conditions to manage them well. Early diagnosis and the right treatment can greatly improve outcomes. Ongoing research helps us find better treatments for these complex diseases.
Multiple myeloma is a blood cancer that starts in the bone marrow. It causes the growth of bad plasma cells. This can lead to anemia, bone pain, and more infections.
We will look at how multiple myeloma affects the bone marrow and the treatments available. Knowing about this condition is key for both patients and doctors to manage it well.
Multiple myeloma fills the bone marrow with bad cells. This can cause anemia, thrombocytopenia, and leukopenia. Patients then face more infections and bleeding.
The disease also damages bones by making osteoclasts work too much. This can cause bone pain, fractures, and high calcium levels.
Treatment for multiple myeloma is made just for each patient. It might include different therapies. The main treatments are:
| Treatment Approach | Description | Benefits |
| Targeted Therapy | Drugs targeting specific molecules in myeloma cells | Improved response rates, fewer side effects |
| Chemotherapy | Conventional drugs killing rapidly dividing cells | Effective in reducing myeloma cell burden |
| Stem Cell Transplantation | High-dose chemotherapy followed by stem cell infusion | Potential for prolonged remission |
By understanding how multiple myeloma affects the bone marrow and the treatments available, patients and doctors can create a good plan together.
It’s key to understand rare genetic bone marrow disorders for better patient care. These conditions, often passed down, make it hard for the bone marrow to make healthy blood cells. This leads to different health problems.
We’ll look at three rare inherited bone marrow disorders: Diamond-Blackfan anemia, Shwachman-Diamond syndrome, and GATA2 deficiency. Each one brings its own challenges in finding and treating the condition.
Diamond-Blackfan anemia is a rare genetic disorder. It makes it hard to produce red blood cells. It usually starts in infancy or early childhood.
A leading hematologist says, “Diamond-Blackfan anemia needs a detailed treatment plan. It often involves a team of healthcare professionals.”
“Managing Diamond-Blackfan anemia is complex. It requires careful thought about the patient’s health and needs.”
Shwachman-Diamond syndrome is a genetic disorder that affects many parts of the body. It impacts the bone marrow, pancreas, and skeleton. It also raises the risk of infections, leukemia, and other issues.
Managing Shwachman-Diamond syndrome involves supportive care like pancreatic enzyme replacement. It also means watching for possible complications.
GATA2 deficiency is caused by mutations in the GATA2 gene. It leads to a lack of blood cells and makes people more prone to infections and immune disorders.
GATA2 deficiency shows how vital genetic testing is. It helps diagnose rare bone marrow disorders and guides treatment.
The link between lymphoma and bone marrow involvement is complex and key to effective treatment. Lymphoma, a cancer of the lymphatic system, can harm the bone marrow. This can lead to health issues. We’ll look at how lymphoma impacts the bone marrow and how to diagnose it.
Lymphomas can invade the bone marrow, disrupting its blood cell production. This can cause anemia, infections, and bleeding problems. The extent of bone marrow involvement often correlates with the stage and prognosis of lymphoma. A leading oncologist notes, “The bone marrow’s role in lymphoma is not just a passive bystander; it’s an active participant in the disease’s progression.”
“Understanding the complex relationship between lymphoma and bone marrow is vital for developing targeted therapies.”
Diagnosing bone marrow infiltration in lymphoma requires several tests. Bone marrow aspiration and biopsy are key. These procedures allow for the examination of bone marrow cells to detect lymphoma cells. Imaging studies, like PET scans, may also be used to check the extent of lymphoma in the bone marrow. Accurate diagnosis is essential for staging and treatment planning.
To find bone marrow problems, we use many tests and procedures. These tools help us understand the causes and plan treatments.
Bone marrow aspiration and biopsy are key tests. They let us see what’s inside the bone marrow. A biopsy takes a small bone piece with marrow.
These tests tell us about the bone marrow’s cells. They help us spot issues like leukemia and lymphoma.
Blood tests check how well the bone marrow works. A complete blood count (CBC) shows if there are problems with blood cells.
Imaging studies like X-rays and CT scans show how far the disease has spread. They also find any other issues.
| Imaging Study | Use in Bone Marrow Disorders |
| X-ray | Assesses bone structure and detects bone lesions |
| CT Scan | Provides detailed images of bones and soft tissues, helping identify disease extent |
| MRI Scan | Offers high-resolution images of bone marrow, useful for detecting infiltration or fibrosis |
| PET Scan | Evaluates metabolic activity in the bone marrow, aiding in the assessment of disease activity |
Genetic testing is key in finding bone marrow problems. It finds specific genetic changes. This helps us diagnose conditions like myeloproliferative neoplasms.
It also helps us figure out the risk and plan treatments for patients.
Medical research and technology have made big strides in treating bone marrow disorders. We’ve seen new targeted therapies and better stem cell transplants. These changes have greatly improved life for those with these conditions.
We’ve talked about different bone marrow disorders and how to catch them early. We’ve also looked at the many ways to treat them. Knowing more about these disorders and their treatments helps us support patients better.
The future for treating bone marrow disorders is bright. Ongoing research is leading to new treatments. As we learn more, we’ll see even better results for patients. Our goal is to provide top-notch care and support to everyone.
Bone marrow disorders happen when the bone marrow can’t make healthy blood cells. These issues can be passed down or happen later in life. They can be mild or serious.
Bone marrow is the soft tissue inside some bones. It’s key for making blood cells. This includes red blood cells, white blood cells, and platelets.
Symptoms vary but often include tiredness, frequent infections, and easy bruising or bleeding.
Aplastic anemia is when the bone marrow can’t make new blood cells. This leads to anemia, infections, and bleeding.
Leukemia is cancer in the bone marrow and blood. It’s caused by abnormal white blood cells.
Myelodysplastic syndromes (MDS) are conditions where the bone marrow makes bad blood cells. They can lead to leukemia.
Myeloproliferative neoplasms are when the bone marrow makes too many blood cells. This includes polycythemia vera and others.
Multiple myeloma is a cancer of plasma cells in the bone marrow. It causes anemia, bone damage, and infections.
Doctors use bone marrow tests, blood tests, and imaging to diagnose these disorders.
Genetic testing finds specific mutations in bone marrow disorders. It helps in diagnosis and treatment planning.
Treatments vary by condition. They include targeted therapies, stem cell transplants, and supportive care.
Rare disorders like Diamond-Blackfan anemia and Shwachman-Diamond syndrome affect blood cell production. They are genetic.
Lymphoma can damage the bone marrow. Diagnosing bone marrow involvement is key for treatment planning.
Bone marrow failure means the marrow can’t make enough blood cells. It’s serious and can cause health problems.
Diseases include leukemia, myelodysplastic syndromes, and multiple myeloma. There are many types.
Complications include anemia, infections, bleeding, and organ damage. They depend on the disorder and its severity.
References
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!