Last Updated on November 17, 2025 by Ugurkan Demir
Are you or a loved one feeling unexplained fatigue, infection risk, or bleeding? It’s important to find out why. At LivHospital, we focus on you to find the cause of anemia, low white blood cells, and platelets. We offer top-notch care and answers you can rely on.
Aplastic anemia is a rare but serious disease. It happens when the bone marrow doesn’t make enough blood cells. This leads to pancytopenia, causing serious health problems. It’s key to spot the signs early for the best treatment.
We’ll look at the 7 main signs that show bone marrow isn’t working right. Knowing these signs helps patients get the care they need quickly.

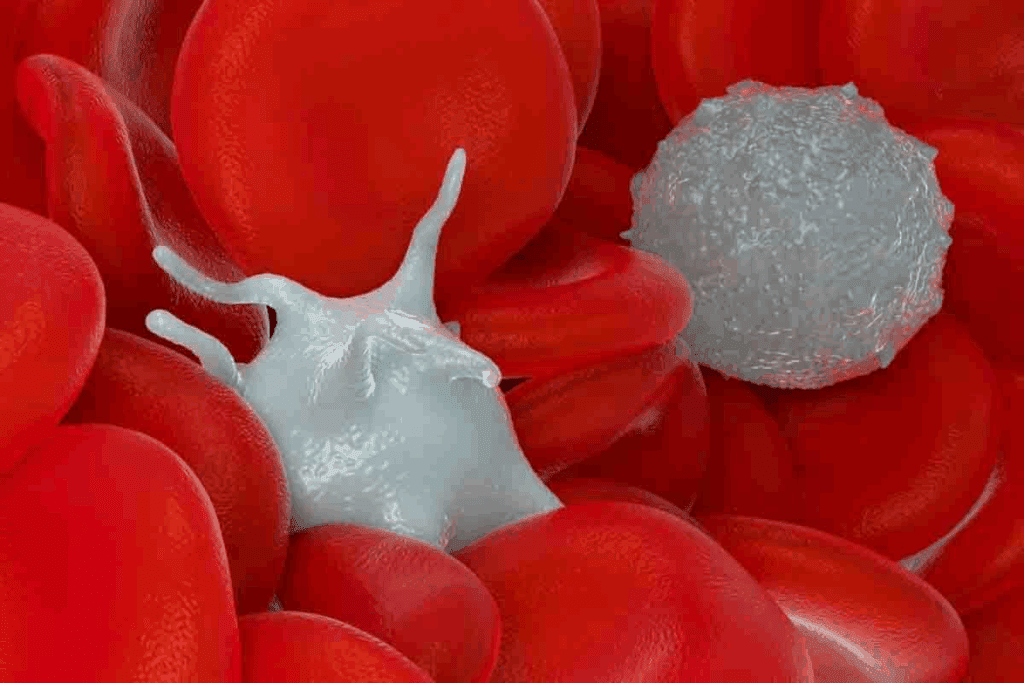
The production of blood cells starts in the bone marrow. Here, stem cells turn into different types of blood cells. This is key to keeping the right balance of blood cells in our bodies.
Bone marrow is the spongy tissue inside bones like the hips and thighbones. It makes blood cells. Stem cells in the marrow grow into red blood cells, white blood cells, and platelets. The marrow helps these cells grow and then they enter the bloodstream.
Red blood cells are made through erythropoiesis. This is when stem cells turn into red blood cells and enter the bloodstream. Red blood cells carry oxygen to our body’s tissues. A healthy adult makes about 2 million red blood cells every second.
White blood cells help fight infections and are made through leukopoiesis. Platelets, which help blood clot, are made through thrombopoiesis. Both happen in the bone marrow and are important for our health.
The production of blood cells is carefully controlled. This balance is vital for our health. An imbalance can cause problems like anemia, infections, or bleeding disorders. The bone marrow adjusts production to meet the body’s needs, ensuring we have enough of each type of blood cell.
| Blood Cell Type | Production Process | Function |
| Red Blood Cells | Erythropoiesis | Carry oxygen from lungs to tissues |
| White Blood Cells | Leukopoiesis | Fight infections |
| Platelets | Thrombopoiesis | Enable blood clotting |

Bone marrow failure to produce red blood cells can happen for many reasons. Knowing these causes is key to finding and treating bone marrow problems.
Aplastic anemia is when the bone marrow fails to make blood cells. This leads to a lack of red blood cells, white blood cells, and platelets. It can be caused by toxins, some medicines, or viruses that harm the bone marrow.
We will look into how aplastic anemia affects blood cell production. Diagnosing it involves blood tests and a bone marrow biopsy.
| Cause | Description | Impact on Blood Cells |
| Toxins and Chemicals | Exposure to certain chemicals can damage bone marrow | Reduction in red blood cells, white blood cells, and platelets |
| Medications | Certain drugs can suppress bone marrow activity | Pancytopenia or specific cytopenias |
| Viral Infections | Viruses like hepatitis can affect bone marrow function | Variable impact on blood cell counts |
Myelodysplastic syndromes are when the bone marrow doesn’t make blood cells right. They can turn into acute myeloid leukemia (AML) in some cases. Doctors check the bone marrow for changes in blood cells to diagnose MDS.
“Myelodysplastic syndromes are a group of disorders caused by poorly formed or dysfunctional blood cells, typically leading to anemia, infection, and bleeding complications.”
Fanconi anemia is a rare genetic disorder that causes bone marrow failure and raises cancer risk. Other genetic disorders can also harm bone marrow, leading to a lack of red blood cells.
We will talk about the genetics behind these disorders and their effects. Genetic tests are important for diagnosing them.
Secondary causes of bone marrow failure include certain medicines, toxins, and infections. These can damage the bone marrow, reducing blood cell production.
It’s important to understand secondary causes of bone marrow failure for effective treatments. We will look at the different secondary causes and how they affect bone marrow.
Fatigue and weakness that don’t go away with rest might mean a serious problem. This could be because the bone marrow isn’t making enough red blood cells. This is a common sign of anemia, where the bone marrow can’t make enough red blood cells.
Anemia makes you tired because there are fewer red blood cells. This means tissues don’t get enough oxygen. Without enough oxygen, tissues can’t make energy, leading to weakness and exhaustion.
Fatigue has many causes, but anemia-related fatigue is different. It doesn’t get better with rest. Unlike tiredness from not sleeping or working too hard, anemia-related fatigue lasts and affects daily life. Knowing why you’re tired is key to feeling better.
Fatigue from bone marrow failure gets worse over time. As the bone marrow can’t make red blood cells, anemia and its symptoms get worse. This makes everyday tasks harder.
Anemia’s fatigue and weakness deeply affect daily life and quality of life. Simple tasks become hard, and enjoying activities you once loved is lost. Finding and treating the cause of anemia is vital to feeling better and living a better life.
A decrease in red blood cell production can show in different ways, like changes in skin color. When our bone marrow doesn’t make enough red blood cells, it leads to anemia. This is when there’s less hemoglobin in the blood.
Hemoglobin is key for carrying oxygen to our body’s parts. Its lack causes paleness because less oxygen reaches tissues. This paleness is not just in the skin but also in mucous membranes.
Hemoglobin is vital for our skin’s color. Normal hemoglobin levels give us a healthy, rosy look. But, low levels make the skin pale.
With less hemoglobin, the skin gets less oxygen. This makes it paler. At first, the change is small but gets clearer as anemia gets worse.
Pallor shows up differently on our body. The face, lips, inner eyelids, and nail beds are key areas. These spots are more telling of anemia than others.
Looking at these areas can tell us a lot about anemia. For example, pale inner eyelids are a big sign.
Nail bed pallor is when the nail beds look pale or white. Normally, they’re pink because of good blood flow. But in anemia, they’re not.
Conjunctival paleness is another sign. The conjunctiva, the eye’s white part and eyelid inside, loses its pink color in anemia.
Pallor can be an early sign of anemia. But how severe it is can show how bad the condition is. Severe pallor, with symptoms like tiredness and short breath, means a big drop in red blood cells.
Seeing a doctor quickly is key when pallor is severe. Untreated severe anemia can cause serious health issues, like heart problems and poor oxygen to vital organs.
Shortness of breath and heart palpitations are signs the body isn’t making enough red blood cells. This often happens when the bone marrow fails. Without enough red blood cells, the body’s tissues and organs don’t get enough oxygen. This leads to various body responses.
The heart tries to fix the low oxygen problem by beating faster and pumping more. This is a key effort to keep vital organs oxygenated. But, it can cause symptoms like heart palpitations and a fast heart rate.
People with anemia from bone marrow failure often can’t handle simple tasks. This is because their body can’t meet the oxygen demand during activity. It really affects their quality of life.
“Patients with severe anemia may experience shortness of breath even at rest, highlighting the severity of their condition and the need for prompt medical evaluation.”
In severe anemia, the heart works harder to pump more blood. This can cause a fast heart rate and heart murmurs. These signs show the heart’s effort to meet the body’s oxygen needs.
| Symptom | Description | Clinical Significance |
| Tachycardia | Rapid heart rate | Compensatory mechanism for low oxygen delivery |
| Heart Murmurs | Abnormal heart sounds | Potential indication of severe anemia and increased cardiac workload |
| Exertional Dyspnea | Shortness of breath during activity | Indicator of inadequate oxygen supply during increased demand |
Some heart symptoms can be managed with care, but others need immediate help. Severe chest pain, trouble breathing at rest, or palpitations with dizziness or fainting are urgent signs.
It’s key to understand how anemia and bone marrow failure affect the heart. If you have symptoms like shortness of breath or heart palpitations, see a doctor right away.
Frequent infections can signal a problem with the bone marrow. It’s not making enough white blood cells to fight off germs. This makes it hard for the body to fight off infections.
Anemia and low white blood cell count often happen together in bone marrow failure. The bone marrow makes both red and white blood cells. Research shows that bone marrow problems can lower both types of blood cells.
It’s important to understand how anemia and low white blood cell count are linked. Anemia means not enough red blood cells, while low white blood cells make infections more likely.
Neutropenia is when you don’t have enough neutrophils, a key white blood cell. This makes you more likely to get infections, like those from bacteria and fungi.
Key facts about neutropenia:
Those with bone marrow failure often get infections because their immune system is weak. Common infections include:
Fever is a key warning sign of infection in those with bone marrow failure. It’s important for them to watch their temperature and seek help if it gets too high.
When to seek medical help:
Getting medical help quickly is key for managing infections in those with bone marrow failure. Early treatment can greatly improve their chances of recovery.
When the bone marrow doesn’t make enough platelets, you might see unusual bleeding and bruising. This is a sign of a health problem. It’s called thrombocytopenia and can cause mild to severe issues.
Having low platelets and hemoglobin is very worrying. Low hemoglobin means you have anemia, leading to tiredness, weakness, and shortness of breath. With low platelets, the risk of bleeding goes up a lot. This is because the bone marrow can’t make enough blood cells.
Spontaneous bleeding is a big worry. It’s when you bleed without any reason, like nosebleeds, gum bleeding, or easy bruising. If you bleed a lot and it doesn’t stop, you need to see a doctor fast. Prolonged bleeding can cause a lot of blood loss, making anemia worse and could be life-threatening.
Petechiae and purpura are signs of low platelet counts. Petechiae are small spots on the skin from minor bleeding. Purpura are bigger bruises from blood leaking into the skin. These signs often show up in people with thrombocytopenia and mean the bone marrow might not be working right.
Mucosal bleeding happens in the mucous membranes, like the nose, mouth, and stomach. Symptoms include nosebleeds, gum bleeding, and stomach bleeding. These are big problems for people with low platelets because they can lose a lot of blood if not treated right.
Dizziness, headaches, and changes in thinking can mean you might have anemia. This happens when your bone marrow doesn’t make enough red blood cells. Without enough red blood cells, your body’s tissues and organs don’t get enough oxygen. This leads to a condition called cerebral hypoxia.
Cerebral hypoxia is when your brain doesn’t get enough oxygen. This can happen if you have severe anemia. Symptoms include dizziness, feeling lightheaded, and even fainting. The brain is very sensitive to oxygen levels. Any drop can really affect how it works.
Neurological symptoms like dizziness, headaches, and changes in thinking are important warning signs. They can show that you might have anemia or a problem with your bone marrow. It’s key to notice these signs and see a doctor if they keep happening or get worse.
In severe cases of anemia, you might faint because your brain doesn’t get enough oxygen. Near-syncope is when you feel like you’re going to faint but don’t. Both are serious and need quick medical help.
Anemia can make it hard to focus and think clearly. You might have trouble concentrating, forget things, or feel mentally foggy. These problems can really affect your daily life. It’s important to find and fix the cause of anemia to get better.
Dizziness, headaches, and changes in thinking are big signs of anemia caused by bone marrow problems. Spotting these symptoms early and knowing what they mean can help you get the right treatment. This can make a big difference in how you feel and do.
Laboratory abnormalities are key signs of bone marrow failure. They give vital clues for diagnosis and treatment. The main signs include low hemoglobin and hematocrit, a low white blood cell count, and fewer platelets.
Low hemoglobin and hematocrit mean you might have anemia. Anemia is when you don’t have enough red blood cells or hemoglobin. Hemoglobin carries oxygen, and hematocrit is the red blood cell percentage in your blood.
When these values drop, you might feel tired, weak, or have trouble breathing.
Here’s a summary of what low hemoglobin and hematocrit values mean:
| Parameter | Normal Range | Low Value Indication |
| Hemoglobin (g/dL) | 13.8-17.2 (men), 12.1-15.1 (women) | Anemia, possible bone marrow failure |
| Hematocrit (%) | 40.7-50.3 (men), 36.1-44.3 (women) | Anemia, possible bone marrow failure |
A low white blood cell count, or leukopenia, shows bone marrow issues. White blood cells fight infections. A differential count shows the types of white blood cells, helping pinpoint the problem.
White Blood Cell Differential Count:
| Type of White Blood Cell | Normal Range (%) |
| Neutrophils | 45-75 |
| Lymphocytes | 20-40 |
| Monocytes | 5-10 |
| Eosinophils | 1-4 |
| Basophils | <1 |
A low platelet count, or thrombocytopenia, raises bleeding risks. Platelets help blood clot. Low counts can cause easy bruising and nosebleeds.
A bone marrow biopsy removes a sample for examination. It shows the cause of bone marrow failure, like abnormal cells or fibrosis.
Biopsy results help diagnose aplastic anemia, myelodysplastic syndromes, and other disorders. Knowing these findings is key for the right treatment.
Bone marrow failure diagnosis and treatment have seen big improvements. This gives new hope to those facing this serious condition. Finding out if you have bone marrow failure involves many tests and checks.
The first step in diagnosing bone marrow failure is a complete blood count (CBC). This test looks at the levels of different blood cells. If the CBC shows problems, more tests are done.
These tests help doctors figure out why you have bone marrow failure. They then decide the best treatment for you.
Genetic testing is key in diagnosing bone marrow failure, like in Fanconi anemia. Tests like cytogenetic analysis and molecular testing give important info. They help doctors choose the right treatment.
Treatment for bone marrow failure depends on the cause and how severe it is. Options include:
We create a treatment plan that fits each patient’s needs and situation.
Supportive care is a big part of treating bone marrow failure. It focuses on managing symptoms and improving life quality. Blood transfusions help with anemia and prevent bleeding.
We offer full care and support. This helps patients with bone marrow failure deal with their condition and get the best results.
Understanding bone marrow disorders is key to managing them. We’ve talked about the 7 main signs that show bone marrow isn’t making enough red blood cells. Early diagnosis and treatment are very important.
Living with bone marrow failure means constant medical care and checks. Knowing the signs helps people manage their condition better. If you notice any of these signs, get medical help right away.
Getting medical help on time is critical for bone marrow disorders. This way, people can get the right treatment and support. It helps improve their overall health and well-being.
Signs include persistent fatigue and weakness. You might also notice pale skin and mucous membranes. Shortness of breath and heart palpitations are common.
Frequent infections and poor immune response are also signs. Unusual bleeding and bruising can occur. Dizziness, headaches, and cognitive changes are other symptoms. Laboratory abnormalities can also indicate this issue.
Anemia means your body doesn’t make enough red blood cells. This reduces oxygen delivery to tissues and organs. As a result, you feel tired and weak.
Hemoglobin gives blood its red color. Low hemoglobin levels make skin and mucous membranes pale. This is known as pallor.
Yes, anemia and low white blood cell count can happen together. This makes you more prone to infections.
Neutropenia is when you have too few neutrophils. Neutrophils fight infections. So, having low neutrophils means you’re at higher risk for infections.
Low platelets and hemoglobin are dangerous together. They can cause bleeding disorders and anemia. This makes the situation more complex.
Diagnosis starts with blood tests to check for low hemoglobin, white blood cells, and platelets. A bone marrow biopsy is then done to confirm the diagnosis.
Treatment depends on the cause and severity. It may include immunosuppressive therapy, bone marrow transplantation, or supportive care. This includes blood product transfusions.
Genetic testing is key in finding the cause of bone marrow failure. It helps identify genetic disorders like Fanconi anemia.
It can greatly affect daily life and quality of life. Symptoms like persistent fatigue, frequent infections, and bleeding disorders are common. These symptoms make everyday activities challenging.
References
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!