
Bone marrow suppression, also known as myelotoxicity, is a serious condition. It happens when the bone marrow can’t make enough blood cells.
At Liv Hospital, we know how tough bone marrow suppression is for patients. We’re dedicated to giving top-notch care to help manage its effects.
We follow the latest research and care plans to help those with bone marrow toxicity. We make sure they get all the help they need during their treatment.
We aim to teach and support our patients. We want to give them the tools to handle their care well.
Key Takeaways
- Understanding bone marrow suppression is key to good patient care.
- Myelotoxicity affects blood cell production, causing health issues.
- Liv Hospital is dedicated to top healthcare and international patient support.
- We use the latest research to lessen bone marrow toxicity.
- Teaching and supporting patients is vital for effective treatment.
The Science Behind Bone Marrow Function

The bone marrow is key in making blood cells needed for our body’s functions. It’s a spongy tissue in bones like the hips and thighbones. It produces red blood cells, white blood cells, and platelets that keep us healthy.
Normal Bone Marrow Activity and Blood Cell Production
Bone marrow works hard to make blood cells. Red blood cells carry oxygen, white blood cells fight infections, and platelets help blood clot. Every day, it makes billions of these cells.
The making of blood cells, called hematopoiesis, is a complex process. It turns stem cells into different blood cell types. This process is controlled by growth factors and cytokines. Knowing how bone marrow works helps us understand myelotoxicity.
How Blood Cells Support Overall Health
Blood cells are vital for our health. Red blood cells carry oxygen to our tissues and organs. White blood cells protect us from infections, and platelets stop bleeding by forming clots.
- Red blood cells support oxygen delivery.
- White blood cells fight infections.
- Platelets are critical for blood clotting.
If bone marrow is not working properly, we can get sick. This includes anemia, infections, and bleeding problems. Knowing how blood cells help us stay healthy shows how important bone marrow is.
Bone Marrow Suppression: Definition and Mechanisms
Bone marrow suppression, or myelotoxicity, happens when the bone marrow can’t make enough blood cells. This can be caused by chemotherapy, some medicines, infections, or not getting enough nutrients.
What Happens During Myelotoxicity
When myelotoxicity occurs, the bone marrow makes fewer blood cells. This affects red blood cells, white blood cells, and platelets. These cells are key to carrying oxygen, fighting infections, and stopping bleeding.
People with myelotoxicity might feel very tired, get sick more often, and have trouble stopping bleeding.
The Difference Between Acute and Chronic Suppression
It’s important to know the difference between acute and chronic bone marrow suppression. Acute suppression is short-term, often from chemotherapy or other temporary problems. Chronic suppression lasts longer and needs ongoing care.
Understanding myelotoxicity and its types helps manage bone marrow health. Knowing the causes and effects helps doctors find better treatments.
Common Causes of Myelotoxicity
Myelotoxicity can come from many sources. This includes chemotherapy, some medications, and certain health issues. Knowing these causes helps us manage and lessen the harm to bone marrow.
Chemotherapy Agents and Their Effects
Chemotherapy is a major cause of myelotoxicity. It targets fast-growing cancer cells but also affects bone marrow cells. This can lead to suppression.
The impact of chemotherapy on bone marrow depends on the agent, dosage, and treatment length. Some agents are more likely to cause myelotoxicity than others.
Non-Cancer Medications That Cause Bone Marrow Suppression
Some non-cancer medications can also harm bone marrow. This includes antibiotics, anti-inflammatory drugs, and treatments for chronic conditions. Knowing these side effects helps us care for patients better.
The table below shows common non-cancer medications that can suppress bone marrow:
| Medication Category | Examples | Potential Effect on Bone Marrow |
| Antibiotics | Trimethoprim-sulfamethoxazole | Can cause a decrease in white blood cell production |
| Anti-inflammatory | Nonsteroidal anti-inflammatory drugs (NSAIDs) | May affect platelet production and function |
| Anticonvulsants | Carbamazepine | Can lead to a reduction in blood cell counts |
Disease-Related Causes: Infections and Blood Disorders
Diseases like infections and blood disorders can also cause myelotoxicity. Viral infections can directly harm bone marrow. Blood disorders can also affect the bone marrow’s ability to produce blood cells.
It’s important to understand these disease-related causes. This helps us create effective treatments that address both the disease and its impact on bone marrow.
How Myelotoxicity Affects Different Blood Cells
Myelotoxicity, or bone marrow suppression, impacts blood cells in many ways. It can lower the production of different blood cells. Each type of cell has its own health risks.
Red Blood Cell Reduction and Anemia
Myelotoxicity often leads to fewer red blood cells, causing anemia. Red blood cells carry oxygen. Without enough, you might feel tired, weak, and have trouble breathing. Anemia makes daily tasks harder.
White Blood Cell Depletion and Immune Compromise
It also lowers white blood cells, which fight infections. With fewer white blood cells, you’re more likely to get sick. You might get sick more often, take longer to get better, and have a weaker immune system.
Platelet Deficiency and Bleeding Risks
Myelotoxicity can also reduce platelets, which help blood clot. Fewer platelets mean a higher risk of bleeding and bruising. Even small injuries can be serious because your body can’t clot as well.
In summary, myelotoxicity affects blood cells in different ways. It can cause anemia, increase infection risk, and lead to bleeding problems. Knowing these effects helps manage bone marrow suppression better.
Recognizing Symptoms of Bone Marrow Depression
The signs of bone marrow depression can be hard to spot early. But catching them early is vital to avoid serious problems. Bone marrow depression happens when the bone marrow can’t make enough blood cells. This can be due to chemotherapy, some medicines, or health issues.
Early Warning Signs
Fatigue, frequent infections, and easy bruising or bleeding are early signs. These happen because the bone marrow isn’t making enough blood cells. Fatigue comes from not having enough red blood cells.
Frequent infections are due to a lack of white blood cells, which fight off germs. Easy bruising or bleeding means there aren’t enough platelets, which help blood clot.
It’s important for patients to watch for these signs and tell their doctor. Catching it early can help prevent it from getting worse.
Severe Symptoms Requiring Immediate Medical Attention
In serious cases, bone marrow depression can cause life-threatening conditions. These include severe anemia, overwhelming infections, or major bleeding. If not treated, these can be deadly.
Severe anemia makes you very tired, short of breath, and can cause chest pain. Overwhelming infections can lead to sepsis, a serious infection response. Major bleeding can cause shock or organ failure.
If you have a high fever, severe bleeding, or extreme weakness, get help right away. Quick treatment can help manage these severe symptoms and improve your chances of getting better.
Diagnostic Approaches for Myeloid Suppression
Diagnosing myeloid suppression needs a detailed approach with different tests. Finding the right cause is key to treating it well.
Blood Tests and Complete Blood Count Analysis
Blood tests are vital in finding myeloid suppression. A Complete Blood Count (CBC) is the first step. It counts red, white blood cells, and platelets. If these counts are off, it might mean bone marrow issues.
“A CBC is key to spotting low blood cell counts,” says a leading hematologist. “It shows how bad the bone marrow problem is and what might be causing it.”
Advanced Diagnostic Procedures
Even with blood tests, more tests might be needed to find the cause. These include:
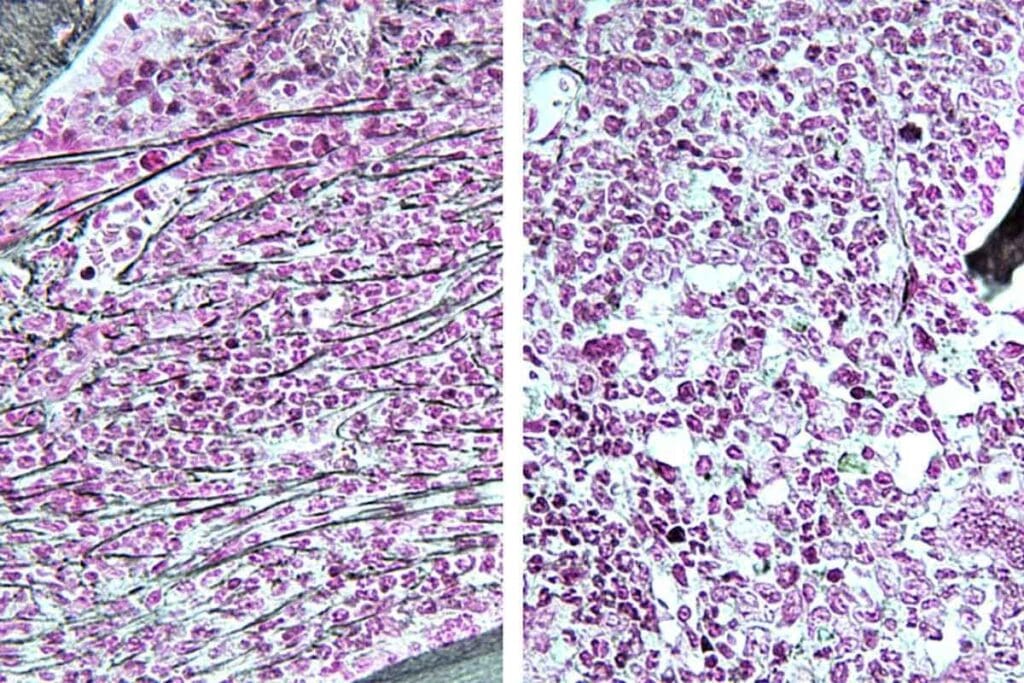
- Bone marrow biopsy: This takes a bone marrow sample for study.
- Imaging studies: Like CT scans or MRI, to check the bone marrow and nearby areas.
- Genetic testing: To find genetic problems that might be causing bone marrow issues.
These tests help doctors understand the patient’s condition better. This lets them make a good treatment plan.
Treatment Strategies for Bone Marrow Toxicity
Managing bone marrow toxicity needs a detailed plan. We’ll look at the ways to lessen its effects and help patients stay healthy.
Medication Management and Dose Adjustments
Medication management and dose adjustments are key. We watch blood cell counts closely when treating with myelotoxic agents. Sometimes, we need to change the dose or stop the treatment to let the bone marrow heal.
We also look for other medicines or doses that might be safer. This tailored approach helps lower the risk of bone marrow problems while treating the condition.
Growth Factor Therapies and Colony Stimulating Factors
Growth factor therapies are vital for making more blood cells. Colony-stimulating factors (CSFs) help grow and develop blood cells. This speeds up the recovery of blood counts, lowering the chance of infections and other issues.
For example, G-CSF boosts neutrophil production, a key white blood cell. Erythropoietin-stimulating agents also increase red blood cells, cutting down on the need for transfusions.
Blood Component Transfusions
When bone marrow toxicity causes severe blood cell shortages, blood component transfusions might be needed. These transfusions can raise red, white blood cells, or platelets. This helps avoid anemia, infections, or bleeding problems.
We decide on transfusions based on the patient’s health, how severe their condition is, and how they react to other treatments.
Using these strategies, we can manage bone marrow toxicity well. This includes medication management, growth factor therapies, and blood transfusions. It helps us reduce the harm caused by myelotoxicity and improve patient results.
Living with Suppressed Bone Marrow
For those with suppressed bone marrow, managing daily life is key. It’s about preventing infections, eating right, and staying active. These steps help keep you healthy and feeling good.
Daily Infection Prevention Strategies
Stopping infections is vital. Stay away from crowded places and wash your hands often. Wear masks when you need to.
Also, watch who you’re around. Try to avoid people who are sick. These steps can really help keep you safe.
Nutritional Support and Dietary Considerations
Eating well is important for making blood cells. Eat foods full of essential vitamins and minerals like iron and vitamin B12. Folate is also key.
Drink lots of water, too. Your doctor might suggest special foods based on your needs.
Physical Activity Guidelines and Energy Conservation
Doing the right kind of exercise is important. But don’t push yourself too hard. Start with easy things like short walks.
Save your energy by taking breaks and focusing on what’s important. Listen to your body and adjust your activities to avoid getting too tired.
Conclusion: Advances in Managing Bone Marrow Suppression
Managing bone marrow suppression is key for those getting treatments that might harm their marrow. At Liv Hospital, we follow the latest research and care plans. This helps us reduce and manage marrow suppression, aiming for the best results for our patients.
Thanks to new ways of handling bone marrow suppression, people with myelotoxicity live better lives. Knowing what causes it, its signs, and how to treat it helps patients. They can work with their doctors to lessen risks and handle side effects.
We’re dedicated to top-notch care, using the newest methods for managing myelotoxicity. By keeping up with the latest in bone marrow suppression, we help people face their treatments with hope and support.
FAQ
What is bone marrow suppression?
Bone marrow suppression, or myelotoxicity, happens when the bone marrow can’t make enough blood cells. This leads to fewer red blood cells, white blood cells, and platelets.
What causes myelotoxicity?
Myelotoxicity can be caused by many things. These include chemotherapy, some medications, infections, and blood disorders.
How does bone marrow suppression affect the body?
It can cause anemia, make you more likely to get infections, and increase bleeding risks. This is because there are fewer red blood cells, white blood cells, and platelets.
What are the symptoms of bone marrow depression?
Symptoms include feeling very tired, getting sick often, and bleeding or bruising easily. In severe cases, it can lead to serious anemia or bleeding.
How is myeloid suppression diagnosed?
Doctors use blood tests, like a complete blood count (CBC), to diagnose myeloid suppression. They also use other tests to check blood cell levels and find the cause.
What are the treatment strategies for bone marrow toxicity?
Treatment includes managing medications, using growth factors, and giving blood transfusions. These help counteract myelotoxicity and support blood cell production.
How can individuals live with suppressed bone marrow?
To live with suppressed bone marrow, you need to manage it carefully. This means preventing infections, eating well, and staying active. It helps keep you healthy and reduces complications.
What is myelosuppression?
Myelosuppression is another name for bone marrow suppression. It means the bone marrow can’t make enough blood cells.
What is the difference between acute and chronic bone marrow suppression?
Acute bone marrow suppression is short-term. Chronic bone marrow suppression lasts longer and needs ongoing care.
References
- Kurtin, S. (2012). Myeloid toxicity of cancer treatment. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC4093344/



































