Last Updated on December 2, 2025 by Bilal Hasdemir
A bone marrow transplant can save lives for many. But, not everyone can get this treatment. Experts say doctors look at patients over 65. They check their overall health to decide.
There are reasons why some can’t get a transplant. Poor health status and organ dysfunction are big ones. These rules help make sure the treatment works best for the patient.
Key Takeaways
- Age can be a consideration for transplant eligibility.
- Overall physical health plays a critical role in deciding if someone can get a transplant.
- Poor health status can make someone not eligible for a transplant.
- Organ dysfunction also affects if someone can get a transplant.
- Doctors look at each patient carefully to see if they’re a good match for a transplant.
Understanding Bone Marrow Transplants
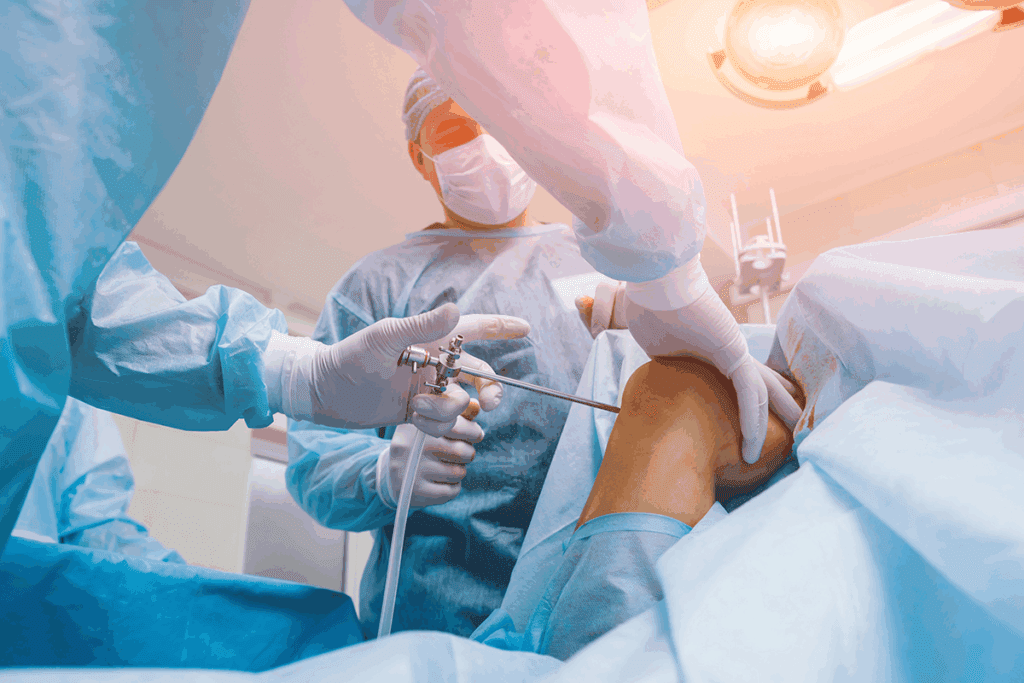
Bone marrow transplants are a complex medical procedure. They are used to treat life-threatening conditions. This treatment replaces unhealthy bone marrow with healthy stem cells, which can cure some diseases.
The Purpose and Types of Bone Marrow Transplants
Bone marrow transplants are key in treating blood disorders and cancers. There are mainly two types: autologous and allogeneic.
The Life-Saving and Risks
Bone marrow transplants can save lives by replacing damaged marrow. But, they also come with risks like graft-versus-host disease and infections.
Autologous vs. Allogeneic Transplants
Autologous transplants use the patient’s own stem cells. This lowers the risk of graft-versus-host disease. Allogeneic transplants use donor cells. They can fight tumors but also have more risks.
Common Conditions Treated with Transplantation
Bone marrow transplants treat several serious conditions, including:
- Leukemia
- Lymphoma
- Aplastic anemia
- Multiple myeloma
These conditions can be deadly if not treated right. Bone marrow transplantation offers a chance for a cure for many patients.
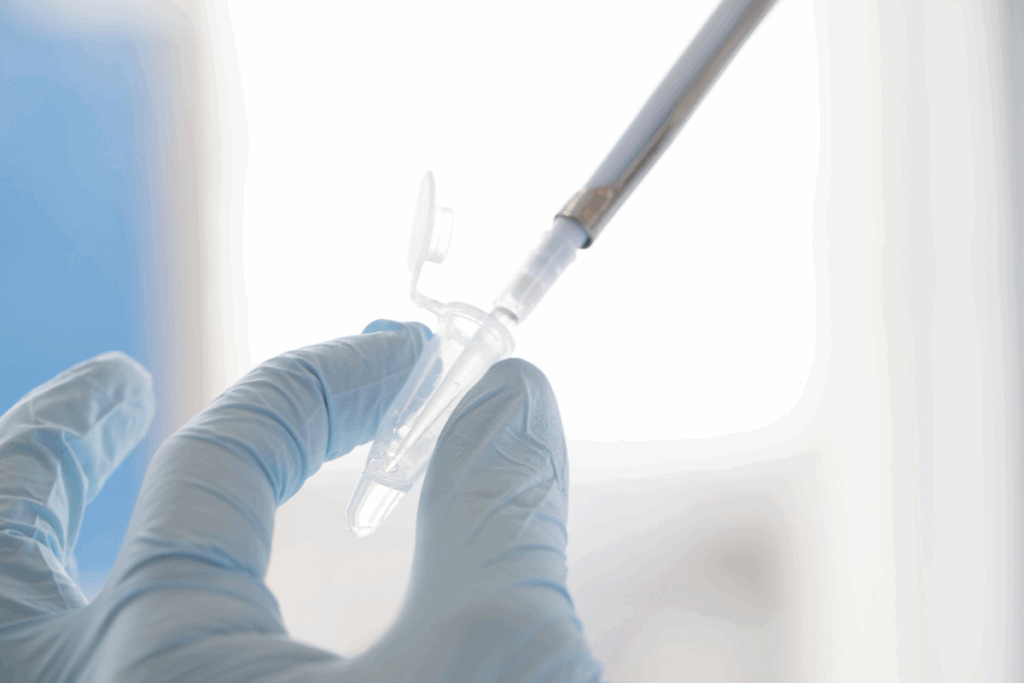
Medical Evaluation Process for Transplant Candidates
A thorough medical evaluation is key to see if a patient can get a bone marrow transplant. This step checks if the patient is healthy enough for the transplant. It also makes sure the benefits of the transplant are worth the risks.
Standard Pre-Transplant Testing
Standard pre-transplant testing is a big part of the evaluation. It includes many checks to see how well the patient is doing.
Physical Examinations
Physical examinations are done to check the patient’s health. They look for any signs of infection or health problems. This helps make sure the transplant will go well.
Laboratory and Imaging Studies
Laboratory studies, like blood tests, check the patient’s blood and organs. Imaging studies
The Multidisciplinary Transplant Team Approach
The transplant team approach brings together many healthcare experts. They work together to decide if a patient can get a bone marrow transplant.
Role of Transplant Physicians
Transplant physicians are very important in the evaluation. They take care of the patient and decide if they can get the transplant.
Input from Specialists and Support Staff
The team also includes nurses, social workers, and nutritionists. They offer their expertise and help with the patient’s physical and emotional needs.
Bone Marrow Transplant Disqualification: General Overview
Figuring out if someone can get a bone marrow transplant involves looking at several things. Some health issues can stop someone from getting this treatment. Doctors make this choice by weighing the risks and benefits, looking at things like organ health and infections.
Absolute vs. Relative Contraindications
There are two kinds of reasons someone might not get a bone marrow transplant. Absolute contraindications are things that make the transplant too risky or not possible, like severe organ failure or infections that can’t be stopped. Relative contraindications, on the other hand, are things that might raise the risks but don’t always mean no transplant.
For example, someone with past infections or organ problems might be looked at differently. The transplant team will decide if the benefits of the transplant are worth the risks for that person.
Risk-Benefit Assessment in Borderline Cases
When someone has a relative contraindication, a detailed risk-benefit check is done. A team of doctors looks at the patient’s health, how bad their condition is, and how likely they are to do well with the transplant.
“The decision to proceed with a bone marrow transplant in borderline cases requires careful consideration of the possible risks and benefits, as well as talking openly with the patient about their chances and other options.”
Transplant Center-Specific Criteria
Each transplant center has its own rules for who can get a transplant. These rules might include the patient’s age, health, and any medical conditions they have. Knowing these rules is important for patients and their families as they go through the transplant process.
Evolution of Eligibility Standards Over Time
Rules for who can get a bone marrow transplant have changed over time. New medical tech and treatments have made some things that used to be a no-go now okay. It’s important for both patients and doctors to keep up with these changes.
Age and Physical Condition Limitations
Age and physical health are key factors in deciding if a patient can get a bone marrow transplant. The transplant process is tough. Both age and physical condition are important in seeing if a patient can handle it.
Age Considerations for Different Transplant Types
There are different bone marrow transplants, each with its own age limits. For example, traditional allogeneic transplants were mainly for younger patients. This was because the risks were higher.
Traditional Age Cutoffs and Modern Approaches
Before, age limits were strict, often stopping transplants at 55. But now, some places are more open. They might consider patients over 65.
Performance Status and Frailty Assessment
A patient’s performance status and frailty are key in deciding if they can get a transplant. There are scales to check these factors.
Karnofsky and ECOG Performance Scales
The Karnofsky Performance Status (KPS) and the Eastern Cooperative Oncology Group (ECOG) scales are used to check a patient’s health. A higher KPS score or a lower ECOG score means better health.
| Karnofsky Performance Status | ECOG Performance Status | Description |
| 80-100% | 0-1 | Able to carry on normal activity |
| 50-70% | 2 | Requires some assistance |
| Below 50% | 3-4 | Disabled, requires significant assistance |
Impact of Obesity and Malnutrition
Obesity and malnutrition can hurt a patient’s chances after a transplant. Malnutrition can increase infection risks and slow recovery. Obesity can lead to more transplant problems.
Organ Function Requirements
The health of vital organs is key when deciding if a patient can get a bone marrow transplant. Problems with organs can raise the risks of the transplant and affect the patient’s chances of recovery.
Heart and Cardiovascular Health
When thinking about bone marrow transplants, the heart’s health is very important. Doctors check the heart’s strength through different tests.
Ejection Fraction Thresholds
The left ventricular ejection fraction (LVEF) shows how well the heart pumps blood. A certain LVEF level is needed for a patient to be eligible for a transplant.
Arrhythmias and Coronary Disease
Heart problems like arrhythmias or coronary artery disease can make the transplant harder. Patients with serious heart issues are seen as high-risk.
Lung Function Parameters
Lungs need to be strong enough to handle the transplant. Pulmonary function tests (PFTs) check how well the lungs work.
Pulmonary Function Test Requirements
PFTs look at lung function, like forced expiratory volume (FEV1) and diffusing capacity of the lungs for carbon monoxide (DLCO). These tests help find patients at risk for lung problems.
Liver Function Tests and Thresholds
The liver’s health is also very important for transplant eligibility. If the liver isn’t working right, it can lead to more complications.
Bilirubin and Enzyme Levels
Tests for liver function include checking bilirubin and liver enzymes. High levels mean the liver might not be working well.
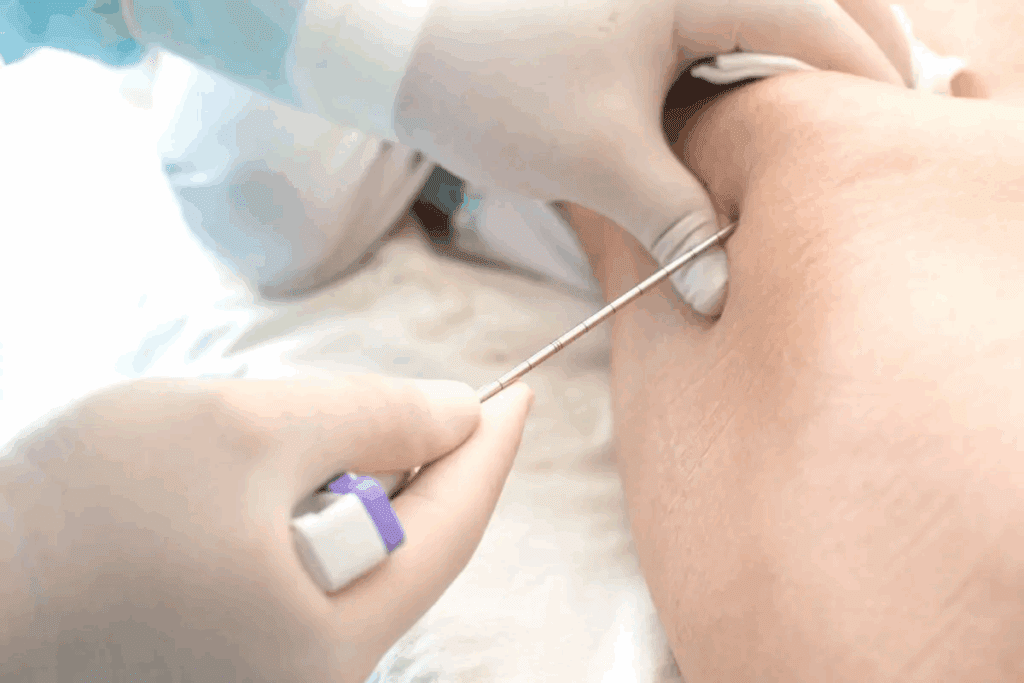
Kidney Function and Dialysis Considerations
Doctors check how well the kidneys work to see if they can handle the transplant’s stress.
Creatinine Clearance and GFR Cutoffs
Tests like creatinine clearance and glomerular filtration rate (GFR) check kidney function. Patients with very bad kidney problems might not be eligible or need extra care.
Active Infections and Immune System Issues
Checking for active infections and immune system problems is key in bone marrow transplant checks. An active infection can make it hard for a patient to get a transplant. It might risk the transplant’s success.
Bacterial, Viral, and Fungal Infections
Infections come from bacteria, viruses, or fungi. Each needs its own way to be treated. Quick and strong treatment is key to fight the infection before the transplant.
Acute vs. Chronic Infection Management
Acute infections need fast and strong treatment. Chronic infections might need ongoing care. “Handling infections in transplant hopefuls is complex,” say doctors.
HIV and Hepatitis Status
A patient’s HIV and hepatitis status is very important for transplant suitability. New treatments for HIV have made transplants possible for more people.
Current Protocols for Viral Infections
Today, we treat viral infections like HIV and hepatitis with medicines and watchful care. Customizing treatment for each patient is key for the best results.
Recent Vaccination Considerations
Recent vaccines can also affect transplant eligibility. Live vaccines are risky for those with weak immune systems.
Live Vaccine Timing Restrictions
There are rules for live vaccines to keep patients safe. Usually, live vaccines should be given at least 4 weeks before starting treatments that weaken the immune system.
In summary, infections and immune system problems are big factors in getting a bone marrow transplant. It’s vital to carefully check and manage these issues for the best results for patients.
Cancer Status and Relapse Risk
Cancer status and the chance of relapse are key in deciding on a bone marrow transplant. The choice to go ahead with a transplant depends on the patient’s current health and the risk of cancer coming back.
Disease Status Requirements
The health of a patient’s disease is very important for transplant eligibility. Patients are sorted based on how well they’ve responded to past treatments.
Complete vs. Partial Remission
Patients in complete remission have no cancer left. Those in partial remission have less cancer but some is left. Most patients in either of these states can get a bone marrow transplant.
Previous Treatment Response
How well a patient has responded to past treatments is also key. Those who have done well with treatments are seen as better candidates.
Refractory Disease Considerations
Patients with refractory disease face a tougher decision. Their cancer hasn’t responded to treatments. The choice to transplant depends on the disease’s severity and other treatment options.
Minimal Residual Disease Considerations
Having minimal residual disease (MRD) means some cancer is left after treatment. Modern tests can find MRD even in small amounts.
Modern Detection Methods and Thresholds
Tests like next-generation sequencing and flow cytometry find MRD. The amount of MRD that’s considered significant varies by cancer type and test.
Important things to think about include:
- The sensitivity of the detection method
- The level of MRD and its implications for relapse risk
- The possibility of further treatment to lower MRD
Donor-Related Disqualifying Factors
Finding the right donor is key in bone marrow transplants. The right donor can make a big difference for a patient’s chance to get the transplant.
HLA Matching Requirements
Human Leukocyte Antigen (HLA) matching is very important in bone marrow transplants. A good match between donor and recipient lowers the risk of graft-versus-host disease (GVHD). It also makes the transplant more likely to succeed.
Full Match vs. Haploidentical Options
Having a full HLA match is the best, but haploidentical donors (half-matched family members) are also considered. Haploidentical transplants are a good option when a full match is not found. They help more patients find a donor.
Donor Availability Issues
Finding a donor can be hard. Even if a donor is found, they must pass a detailed screening to make sure they are a good match.
Registry Searches and Family Testing
Looking through registries and testing family members are important steps to find a donor. National and international registries help find donors. Family testing can find related donors.
Graft Quality Concerns
The quality of the graft is very important. The graft needs enough healthy cells to work well and avoid problems.
Cell Count and Viability Standards
There are strict cell count and viability standards for graft quality. A graft with more cells and higher viability is likely to work better.
HLA matching, donor availability, and graft quality all play a part in choosing a donor for bone marrow transplants. Knowing these factors is important for both patients and doctors in the transplant process.
Psychosocial and Compliance Factors
Psychosocial factors are key in deciding if a patient can get a bone marrow transplant. The process checks if the patient is both medically and mentally ready for the transplant.
Mental Health Considerations
A patient’s mental health is very important for transplant suitability. Mental health issues can make it hard for a patient to handle transplant stress.
Depression, Anxiety, and Coping Capacity
Patients with depression or anxiety might need more support. A detailed check can spot those needing extra care.
Substance Abuse History
Substance abuse history is a big concern. Patients with such a history might need to show they’ve been sober before the transplant.
Sobriety Requirements and Monitoring
Centers have different rules for sobriety before a transplant. But, after the transplant, regular checks help keep the patient sober.
Support System Requirements
A strong support system is vital for transplant patients. Having a caregiver can greatly help in recovery.
Caregiver Availability and Training
Caregivers are key in supporting patients during recovery. They often get training to meet the patient’s needs.
Medication Adherence History
A patient’s history of following medication is also important. Not following medication can cause problems and affect transplant success.
Compliance Assessment Methods
There are many ways to check if a patient follows their medication. These methods help find and fix any issues with following medication.
| Psychosocial Factor | Assessment Criteria | Importance in Transplant Decision |
| Mental Health | History of depression, anxiety, coping mechanisms | High |
| Substance Abuse | Sobriety period, monitoring requirements | High |
| Support System | Caregiver availability, training | Critical |
| Medication Adherence | History of adherence, compliance assessment | Critical |
“A thorough psychosocial evaluation is key to spotting barriers to a successful transplant.”
— Expert in Bone Marrow Transplantation
Alternative Options for Disqualified Patients
Patients who can’t get a bone marrow transplant have other options. Being turned down for a transplant can happen for many reasons. This doesn’t mean they have no hope.
Clinical Trials and Experimental Protocols
Clinical trials offer new treatments being tested. These might include new drugs or ways to treat diseases like gene therapy.
Expanded Access Programs
Expanded access programs help those who can’t join clinical trials. They’re for people with serious diseases who’ve tried everything else.
Reduced-Intensity Conditioning Regimens
Reduced-intensity conditioning (RIC) is a gentler transplant method. It uses less chemotherapy and radiation. This is for older patients or those with health issues.
Candidates for Modified Approaches
RIC is good for older or sicker patients. It tries to lower the bad effects of traditional transplants while fighting cancer.
Non-Transplant Treatment Strategies
Some patients might do better without a transplant. They can get treatments made just for their disease.
Disease-Specific Alternatives
| Disease | Alternative Treatments |
| Leukemia | Targeted therapies, chemotherapy regimens |
| Lymphoma | Immunotherapy, CAR-T cell therapy |
| Myeloma | Proteasome inhibitors, immunomodulatory drugs |
Conclusion
Figuring out if you can get a bone marrow transplant is complex. It looks at many things that could affect how well the transplant works. Knowing what makes someone not eligible is key for both patients and doctors.
The process to check if you can get a transplant looks at your health, body, and mind. Things like your age, how well your organs work, if you have infections, your cancer status, and if there’s a donor available are important. These all help decide if you’re a good candidate for a transplant.
Doing a full check to see if you’re eligible for a transplant is very important. It helps doctors understand the risks and benefits of the transplant. This helps them decide if the transplant is right for you and how to handle any problems that might come up.
If you can’t get a bone marrow transplant, there are other ways to treat your condition. You might look into clinical trials or other treatments that don’t involve a transplant. Knowing about bone marrow transplant eligibility is important for making the best choices about your health care.
FAQ
What are the main factors that can disqualify someone from a bone marrow transplant?
Several factors can prevent someone from getting a bone marrow transplant. These include poor health, organ problems, and active infections. Heart and lung diseases, liver and kidney issues, and uncontrolled cancer are also concerns. Age, weight, and psychosocial barriers can also play a role.
How is a patient’s overall health evaluated for bone marrow transplant eligibility?
Evaluating a patient’s health for a transplant involves many tests. These include checks on heart and lung function, liver and kidney health, and infection screenings.
Can age be a barrier to bone marrow transplant eligibility?
Yes, age can be a factor. Older patients might face more risks with a transplant. But, each case is judged based on the patient’s health and how well they can handle the transplant.
What are the requirements for organ function in bone marrow transplant candidates?
Candidates need their organs to function well. This includes the heart, lungs, liver, and kidneys. Specific tests and standards are used to check this.
How do active infections affect bone marrow transplant eligibility?
Active infections can make it harder to get a transplant. The type and severity of the infection matter. So does the patient’s overall health.
What is the importance of cancer status and relapse risk in bone marrow transplant eligibility?
Cancer status and the risk of relapse are key. The transplant aims to treat the cancer. The disease’s current state, past treatments, and any remaining cancer cells are considered.
Can a lack of a suitable donor disqualify someone from a bone marrow transplant?
Yes, not having a suitable donor can prevent a transplant. A compatible donor is needed for an allogeneic transplant.
What alternative options are available to patients who are disqualified from bone marrow transplant?
Patients who can’t get a transplant have other options. These include clinical trials, less intense transplant regimens, and non-transplant treatments.
How do psychosocial factors affect bone marrow transplant eligibility?
Psychosocial factors, like mental health and support, matter. They can affect a patient’s ability to follow post-transplant care.
References
Gebel HM, Bray RA, “Major histocompatibility complex class II gene matching in unrelated donor bone marrow transplantation,” Bone Marrow Transplantation





