Stem cell therapy is an exciting new treatment that can repair damaged tissues and organs..
To find out if you can get stem cell therapy, you need to know the basics. This treatment uses stem cells to fix or replace damaged cells. It can help with many diseases and injuries. To qualify, you need to have the right condition and be in good health.
Key Takeaways
- Stem cell therapy has the power to fix damaged tissues and organs.
- Qualifying for stem cell therapy involves several factors, including the type of condition and overall health.
- Understanding the basics of stem cell therapy is key to knowing if you qualify.
- Stem cell therapy is a promising treatment for many medical conditions.
What is a Bone Marrow Transplant?
Stem cell therapy, also known as bone marrow transplant, is a complex treatment. It replaces damaged stem cells with healthy ones. The National Cancer Institute says it’s key for treating serious diseases.
The Science Behind Stem Cell Therapy
Stem cell therapy uses the body’s healing power. It uses stem cells to fix or replace damaged tissues. Stem cells can turn into different cell types, helping treat many health issues.
Types of Stem Cell Transplants: Autologous vs. Allogeneic
There are two main types of stem cell transplants. Autologous transplants use the patient’s own stem cells. Allogeneic transplants use stem cells from a donor. The choice depends on the patient’s health and condition.
How Stem Cells are Collected and Processed
Stem cells can come from bone marrow, blood, or umbilical cord blood. After collection, they are processed and tested. This makes sure they are healthy for transplant.
The bone marrow transplant procedure is a detailed treatment. Knowing the stem cell transplant process is important for those considering it.
Medical Conditions That Qualify for Stem Cell Therapy
Blood Cancers (Leukemia, Lymphoma, Myeloma)
Blood cancers like leukemia, lymphoma, and myeloma are common. They affect blood cells and bone marrow. Stem cell therapy can replace unhealthy cells with healthy ones.
Bone Marrow Failure Syndromes
Bone marrow failure, like aplastic anemia, happens when marrow can’t make enough blood cells. Stem cell therapy can fix this by regrowing the marrow. This improves blood cell production.
Immune Deficiency Disorders
Conditions like severe combined immunodeficiency (SCID) can be treated with stem cells. This therapy boosts the immune system. It helps patients fight off infections better.
Genetic and Metabolic Disorders
Stem cell therapy also helps with genetic and metabolic disorders. It can ease symptoms and improve life quality for those with these conditions.
Stem cell therapy offers new hope for many. It opens up new treatment options for patients with few choices before.
The Initial Screening Process
The journey to stem cell therapy starts with a detailed initial screening. This step is key to see if you’re a good candidate for the treatment.
Getting a Referral from Your Specialist
First, you need a referral from your specialist. This referral is important. It gives the transplant team basic info about your health and past treatments. It’s a critical step that ensures you’re directed to the right team for further evaluation.
First Consultation with the Transplant Team
In your first meeting with the transplant team, you’ll get a full check-up. They’ll look at your health, talk about the risks and benefits of stem cell therapy, and explain what to expect. This meeting is also an opportunity for you to ask questions and understand the procedure in detail.
Required Medical Documentation
You’ll also need to give detailed medical records. This includes your health history, past treatments, and test results. Accurate and complete documentation is vital for the transplant team to assess your eligibility accurately.
Medical Eligibility Requirements for Bone Marrow Transplant
To see if someone can get a bone marrow transplant, doctors look at many things. They check to see who will likely do well and who might face risks.
Age Considerations and Limitations
Age is a big deal when it comes to bone marrow transplants. There’s no age limit, but older people might have more problems. Doctors look at each patient’s health, not just their age.
Overall Health Assessment Criteria
Doctors do a deep check of a patient’s health to see if they can handle the transplant. They look for things like heart disease or diabetes. These can affect how well the transplant works.
Organ Function Requirements
For a bone marrow transplant, organs need to work well. This means the heart, lungs, liver, and kidneys must be okay. Doctors test these organs to make sure the transplant is safe.
Previous Treatment History Evaluation
What treatments a patient has had before is also important. Doctors look at how well those treatments worked and if there were any problems.
“A thorough evaluation of the patient’s treatment history helps in assessing their suitability for a bone marrow transplant.”
By looking at all these things, doctors can decide if someone is a good candidate for a bone marrow transplant. This helps make sure the transplant goes well for the patient.
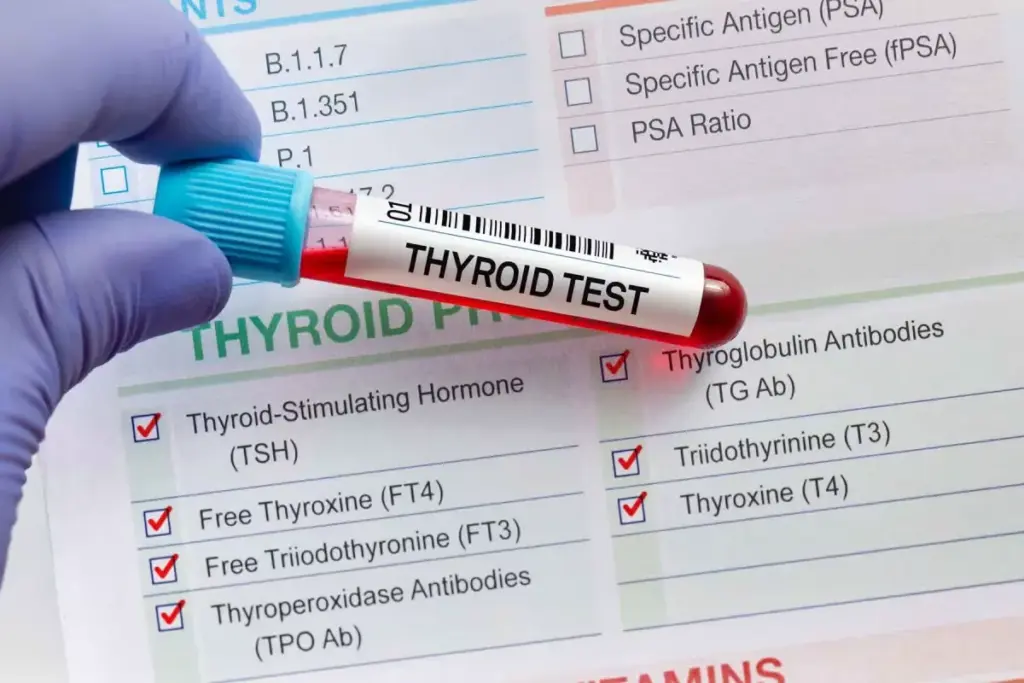
Comprehensive Pre-Transplant Testing
Comprehensive pre-transplant testing is key to check if a patient is ready for a bone marrow transplant. It looks for health risks and makes sure the patient is ready for the transplant.
Blood Work and Laboratory Tests
The first step is blood work and laboratory tests. These tests check the patient’s health, find infections, and check organ function. Tests include:
- Complete Blood Count (CBC)
- Blood chemistry tests
- Infectious disease screening
- Blood typing and cross-matching
Imaging Studies and Organ Function Tests
Patients also get imaging studies and tests on organ function. These include chest X-rays, CT scans, MRI, and echocardiograms. They check for any issues that could affect the transplant.
Psychological Evaluation
A psychological evaluation is also important. It checks if the patient is mentally ready for the transplant. It finds out if they need psychological support.
Dental and Other Specialty Assessments
Patients also need dental and other specialty assessments. This makes sure any health issues are fixed before the transplant. It lowers the risk of problems.
With thorough pre-transplant testing, patients and doctors can understand the transplant’s risks and benefits. This leads to a better outcome for the patient.
Finding a Compatible Stem Cell Donor
Stem cell therapy needs a compatible donor. Finding one is a detailed process. The success of a stem cell transplant depends on the donor and recipient’s match.
HLA Typing and Matching Process
HLA typing is key in finding a compatible donor. It tests proteins on white blood cells to find the individual’s tissue type. A close match between donor and recipient reduces the risk of complications.
HLA matching is critical for transplant success. The closer the match, the lower the risk of problems.
Family Members as Possible Donors
Family members are often the first choice for donors. Siblings have a 25% chance of being a match. Parents and children have a 50% chance of being a half-match. Family members get HLA typed to check their compatibility.
National Marrow Donor Program
If a family member isn’t a match, the next step is the National Marrow Donor Program (NMDP). The NMDP has a registry of donors. It helps find a compatible match for patients.
Cord Blood as an Alternative Source
Cord blood is another stem cell source. It’s available right after birth. But, it’s best for younger patients or those with smaller body mass because of limited stem cells.
| Donor Type | Match Probability | Advantages |
| Family Member | Higher chance of match | Immediate availability, better match possible |
| Unrelated Donor (NMDP) | Varies, depends on registry | Large donor pool, higher match chances |
| Cord Blood | Less stringent HLA matching required | Readily available, lower GVHD risk |
Finding a compatible stem cell donor is complex. It involves HLA typing, family members, unrelated donors, and cord blood. Knowing these options helps patients and families better navigate the process.
The Bone Marrow Transplant Procedure Step by Step
Learning about the bone marrow transplant process is key for those facing this treatment. It covers many steps, from getting ready to aftercare.
Pre-transplant Conditioning Regimen
The pre-transplant phase is vital. It gets the body ready for the transplant. This includes chemotherapy and/or radiation to kill cancer cells and weaken the immune system.
Stem Cell Collection Methods
Stem cells can come from the patient (autologous) or a donor (allogeneic). The choice depends on the transplant type and the patient’s health.
The Transplantation Process
The transplant involves putting stem cells into the patient’s blood. This is done through a central line, like an IV.
Immediate Post-Transplant Monitoring
After the transplant, patients are watched closely for any issues or GVHD. Quick care after the transplant is key for success.
Knowing each part of the bone marrow transplant helps patients prepare for what’s to come.
Insurance and Financial Qualification
Bone marrow transplant patients face complex insurance and financial hurdles. It’s key to understand the costs and insurance needs for a smooth process.
Average Cost of Bone Marrow Transplant
The cost of a bone marrow transplant varies widely. It can be from $200,000 to over $1 million. This depends on the transplant type, patient condition, and treatment center. Costs include pre-transplant checks, the transplant, hospital stay, and post-transplant care.
Insurance Pre-authorization Requirements
Getting insurance pre-authorization is vital before a bone marrow transplant. Patients must work with their healthcare team. They need to get pre-authorization from their insurance to ensure coverage.
Financial Assistance Programs and Resources
Many financial aid programs exist to help with transplant costs. These include patient advocacy groups, non-profit organizations, and government programs. They offer financial support.
- Patient advocacy groups offer financial guidance
- Non-profit organizations provide financial help
- Government programs for eligible patients
Exploring these resources can help manage treatment costs.
Physical and Psychological Preparation
Before a bone marrow transplant, getting ready physically and mentally is key. Studies show that well-prepared patients do better and recover faster.
Recommended Lifestyle Changes Before Transplant
To get ready for a bone marrow transplant, patients need to make some lifestyle changes. They should stop smoking, cut down on alcohol, and eat a nutritious diet full of fruits, veggies, and lean proteins. Also, regular exercise, if possible, helps keep them healthy and strong.
Building Your Support Network
A strong support network is very important for patients going through a bone marrow transplant. This network can include family, friends, and support groups. They offer emotional support, help with daily tasks, and go to medical appointments with the patient.
Caregiver Requirements and Planning
A caregiver is essential for a patient’s recovery. They handle medications, watch the patient’s health, and provide emotional support. It’s important to find a good caregiver and plan their role in advance.
Housing Arrangements for Out-of-Town Treatment
For patients traveling for a bone marrow transplant, finding housing near the treatment center is a must. Many transplant centers have resources or suggestions for places to stay. Patients should look into these options early to find a convenient and affordable spot.
Recovery and Follow-Up Requirements
Recovery and follow-up care are key parts of the bone marrow transplant process. After the transplant, patients need close monitoring. This ensures the new stem cells work right and handles any complications.
Hospital Stay Duration Expectations
The time in the hospital varies based on the transplant type and patient health. Usually, patients stay 2-4 weeks post-transplant. They get close monitoring and supportive care during this time.
The Critical First 100 Days
The first 100 days post-transplant are very important. Patients face a higher risk of infections and graft-versus-host disease (GVHD) during this time. Close follow-up with the transplant team is key to manage these risks well.
Long-term Follow-up Schedule
After the first 100 days, patients keep seeing their transplant team regularly. These visits help track the patient’s recovery and manage long-term side effects. They also catch any complications early.
Managing Possible Complications
Complications like infections, GVHD, and organ damage can happen after a bone marrow transplant. Patients should report any symptoms to their healthcare provider right away. This ensures quick action.
Understanding recovery and follow-up needs helps patients prepare for their journey. Working closely with their healthcare team is key to the best outcomes.
Conclusion: Taking the Next Steps Toward Stem Cell Therapy
Stem cell therapy, including bone marrow transplants, offers new hope for patients with various medical conditions. Understanding the process and qualifying for this treatment is key.
By consulting with a healthcare professional, patients can find out if they qualify for stem cell therapy. They can also learn about the benefits and risks. This first step is vital on the path to recovery.
Patients need to be ready to share their medical history and undergo tests. They should also look into the different treatment options. With the right help and support, individuals can move forward with stem cell therapy. This is the first step towards a healthier future.
FAQ
What is a bone marrow transplant?
A bone marrow transplant replaces a patient’s bone marrow with healthy stem cells. These stem cells come from the patient themselves or a donor.
What medical conditions qualify for stem cell therapy?
Stem cell therapy is for blood cancers, bone marrow failure, immune disorders, and genetic or metabolic diseases.
How do I qualify for a bone marrow transplant?
To qualify, you need a screening, meet health requirements, and pass pre-transplant tests.
What is the initial screening process for stem cell therapy?
The first step is getting a referral and talking to the transplant team. You’ll also need to provide medical records.
What are the medical eligibility requirements for bone marrow transplant?
Requirements include age, health check, organ function, and past treatments.
What is HLA typing and matching?
HLA typing matches donor and recipient stem cells. It’s based on human leukocyte antigen genes.
Can family members be potentially stem cell donors?
Yes, family members are often first tested for compatibility.
What is the average cost of a bone marrow transplant?
The cost varies by transplant type, location, and insurance.
Does insurance cover bone marrow transplant?
Insurance coverage varies by provider and policy. Some may need pre-authorization.
What are the recommended lifestyle changes before a bone marrow transplant?
Before the transplant, quit smoking, eat well, and exercise.
How long does it take to recover from a bone marrow transplant?
Recovery time is several months to a year or more for full immune system recovery.
Can I undergo a bone marrow transplant if I have a pre-existing medical condition?
The decision depends on the condition’s severity. It’s usually decided on a case-by-case basis.
What is the role of a caregiver during a bone marrow transplant?
A caregiver supports the patient emotionally, manages medications, and helps with daily tasks.
How is a bone marrow transplant performed?
The transplant involves a conditioning regimen, stem cell infusion, and monitoring for complications.
What are the possible complications of a bone marrow transplant?
Complications include graft-versus-host disease, infections, and organ damage.