Last Updated on November 17, 2025 by Ugurkan Demir
Choosing to have a bone marrow transplant is a big decision. It’s important to know the risks and complications to make the right choice.
At Liv Hospital, we understand the challenges of transplant rejection. We’re dedicated to giving our patients the best care and support. Our goal is to provide top-notch healthcare, focusing on your safety and the best results.
If you’re thinking about a bone marrow transplant, knowing the risks is key. We’ll explain the 12 main risks, side effects, and complications. This will help you make a well-informed decision about your treatment.
Key Takeaways
- Understanding the risks associated with bone marrow transplant rejection is vital.
- Complications can arise from the transplant procedure.
- Liv Hospital is committed to providing comprehensive care and support.
- Patient safety and top medical outcomes are our top priority.
- Informed decision-making is crucial for successful treatment outcomes.
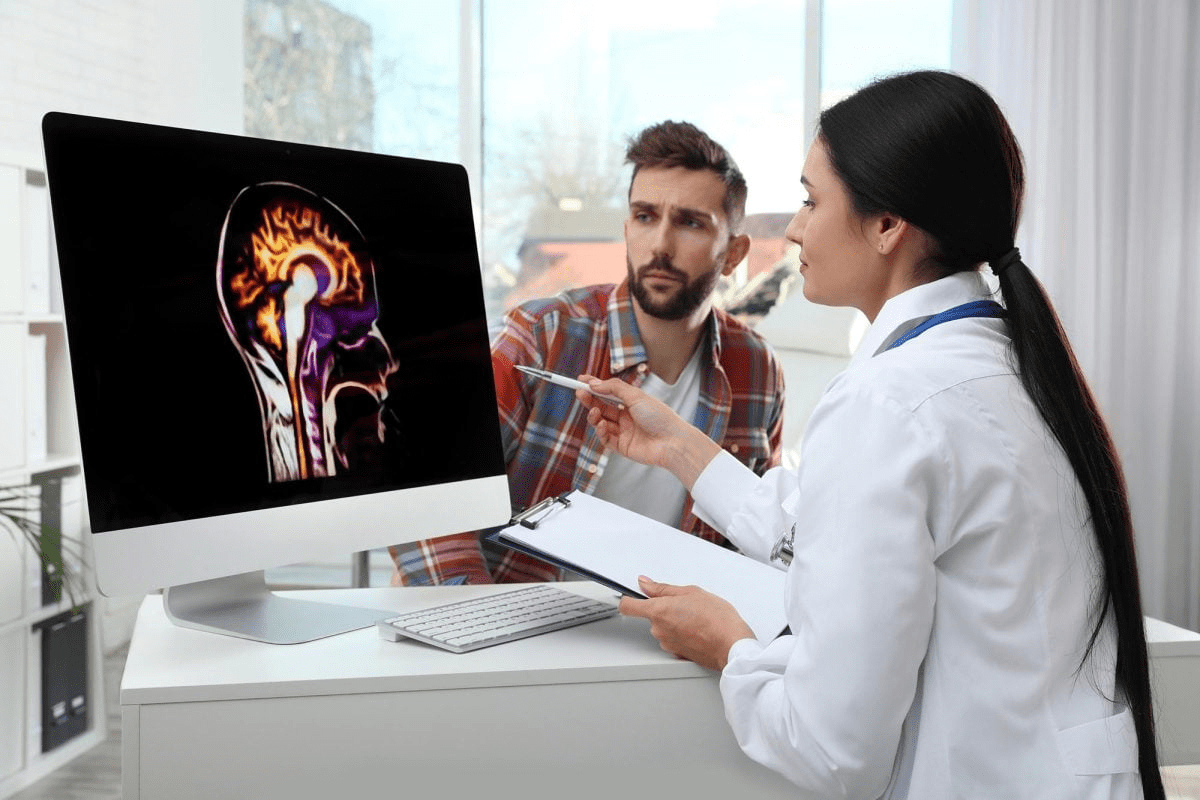
Understanding Bone Marrow Transplants: The Basics
Learning about bone marrow transplants is key for those thinking about this treatment. It’s a procedure that replaces bad bone marrow with good cells. This is often for cancer, blood disorders, or diseases that harm the bone marrow.
What is a Bone Marrow Transplant?
A bone marrow transplant puts healthy cells into your body to replace bad ones. It aims to fix your bone marrow so it can make healthy blood cells again.
Types of Bone Marrow Transplants: Allogeneic vs. Autologous
There are two main types: allogeneic and autologous. An allogeneic transplant uses cells from a donor, like a sibling or someone else. An autologous transplant uses your own cells, which are saved and then put back after treatment.
| Characteristics | Allogeneic Transplant | Autologous Transplant |
| Donor Source | Donor (sibling or unrelated) | Patient’s own cells |
| Graft-Versus-Host Disease (GVHD) Risk | Yes | No |
| Immune System Reconstitution | The donor’s immune system | Patient’s own immune system |
The Transplantation Process
The bone marrow transplant process has several steps. These include checking before the transplant, preparing the body, putting in the bone marrow cells, and caring for the patient after. The conditioning regimen uses strong chemotherapy and/or radiation to clear out bad bone marrow and weaken the immune system.
Bone Marrow Transplant Rejection: Causes and Mechanisms
It’s important for patients and doctors to know about bone marrow transplant rejection. This happens when the body sees the new cells as foreign and fights them off.
How the Immune System Responds to Transplants
The immune system has a complex way of reacting to bone marrow transplants. T cells and B cells are key players in this process. They help the body recognize and fight the new cells.
Key components of the immune response include:
- T cells: Directly kill foreign cells or coordinate the immune response.
- B cells: Produce antibodies against the transplanted cells.
Factors Increasing Rejection Risk
Several things can make bone marrow transplant rejection more likely. These include:
| Factor | Description | Impact on Rejection Risk |
| HLA Mismatch | Degree of mismatch between donor and recipient Human Leukocyte Antigens | Increased risk with greater mismatch |
| Recipient’s Age | Older recipients may have a higher risk due to decreased immune tolerance | Variable, depending on overall health |
| Conditioning Regimen | The intensity of the conditioning regimen before transplant | Can reduce rejection risk if intense enough |
Timeline of Rejection Events
Rejection can happen at different times after the transplant. Knowing when it might happen helps doctors keep an eye on it.
By understanding these points, we can work to lower the chance of bone marrow transplant rejection.
Graft-Versus-Host Disease (GVHD): A Major Complication
Graft-Versus-Host Disease (GVHD) is a big problem after bone marrow transplants. It happens when the donor’s immune cells see the recipient as foreign and attack. This can cause many symptoms and issues.
Acute GVHD: Symptoms and Impact
Acute GVHD starts within 100 days after the transplant. Symptoms include:
- Skin rash: A common sign, looking like a red, itchy rash.
- Liver dysfunction: Shows as jaundice or high liver enzymes.
- Gastrointestinal issues: Symptoms are nausea, vomiting, diarrhea, and stomach pain.
Acute GVHD can really hurt a patient’s quality. It often needs quick medical help.
Chronic GVHD: Long-term Challenges
Chronic GVHD starts after 100 days and can last for years. It affects organs like the skin, liver, mouth, and lungs. Symptoms include:
- Skin thickening: Makes it hard to move.
- Dry mouth and eyes: Causes discomfort and raises dental risks.
- Respiratory issues: Like bronchiolitis obliterans, which harms lung function.
Chronic GVHD needs ongoing care. It can greatly affect a patient’s quality.
Prevention and Management Strategies
To prevent GVHD, several steps are taken:
- Immunosuppressive therapy: Helps by weakening the immune system.
- T-cell depletion: Removes T-cells from the donor graft to lower GVHD risk.
- Careful donor selection: Pick a donor who matches well with the recipient.
Managing GVHD means finding it early and treating it. Treatments include corticosteroids, immunosuppressive drugs, and care to manage symptoms and prevent problems.
Infection Risks Following Transplantation
After a bone marrow transplant, one big risk is getting infections. The immune system is very weak and can’t fight off many pathogens well.
Bacterial Infections
Bacterial infections are a big worry after a transplant. Gram-positive bacteria often cause infections, like those from catheters. Gram-negative bacteria can also lead to serious infections, mainly in those with gut GVHD.
“The risk of bacterial infections is highest during the first few months after transplantation,” a study on bone marrow transplant complications found.
“Infections are a major cause of morbidity and mortality in the post-transplant period, with bacterial infections being a significant contributor.”
-Doctors highlight.
Viral Reactivation and Infections
Viral reactivation is another big risk after bone marrow transplantation. Viruses like Cytomegalovirus (CMV) and Epstein-Barr Virus (EBV) can wake up and cause serious illness. It’s important to watch for these and treat them early.
- CMV reactivation can lead to severe disease, including pneumonia and gastrointestinal disease.
- EBV reactivation can cause post-transplant lymphoproliferative disorder (PTLD), a potentially life-threatening condition.
Fungal Complications
Fungal infections are a serious problem after bone marrow transplantation. Aspergillus and Candida species are common culprits. To lower these risks, antifungal therapy and careful environmental control are key.
Using antifungal drugs to prevent infections has been shown to work. Voriconazole and Posaconazole are examples of drugs used for this purpose.
Organ Damage and Toxicity
Exploring the risks of bone marrow transplants, we see the danger of organ damage and toxicity. This damage can hit the liver, kidneys, heart, and brain. It’s a serious issue that can happen after a transplant.
Liver Complications
Liver toxicity is a big problem after a transplant. It often comes from the treatment that gets the patient ready for the transplant. This can cause sinusoidal obstruction syndrome (SOS), also known as veno-occlusive disease (VOD). SOS/VOD can be very dangerous if not treated right away.
The signs of liver trouble can be mild or very serious. Keeping a close eye on the liver is key after a transplant to catch problems early.
Kidney Dysfunction
Kidney problems can also happen after a bone marrow transplant. The treatment, some medicines, and infections can harm the kidneys. This can lead to acute kidney injury (AKI) and even chronic kidney disease.
To manage kidney issues, it’s important to watch fluid levels, check kidney function tests, and adjust medicines that might harm the kidneys. Finding problems early and treating them quickly is key to avoiding long-term kidney damage.
Cardiac and Neurological Effects
Heart problems can come from the treatment used in bone marrow transplants. This can include cardiomyopathy and heart failure. It’s important to check the heart regularly, even more so if the patient already has heart issues.
Brain problems can also happen, from mild memory issues to serious conditions like posterior reversible encephalopathy syndrome (PRES). Spotting brain symptoms quickly is important for getting the right treatment fast.
In summary, organ damage and toxicity are big risks with bone marrow transplants. Knowing these risks and acting early can help improve patient results.
Pulmonary Complications and Lung Injury
Lung injury is a risk with bone marrow transplants. It leads to various pulmonary complications. These can affect the transplant’s success and the patient’s quality.
Idiopathic Pneumonia Syndrome
Idiopathic pneumonia syndrome (IPS) is a serious issue after bone marrow transplants. It’s a diffuse lung injury without a known cause.
- Symptoms include dyspnea, cough, and fever.
- Diagnosis is typically made by excluding other causes of pneumonia.
- Treatment involves supportive care and, in some cases, immunosuppressive therapy.
Bronchiolitis Obliterans
Bronchiolitis obliterans is a major pulmonary complication after bone marrow transplants. It involves inflammation and fibrosis of the small airways.
Symptoms can include:
- Dry cough
- Dyspnea on exertion
- Wheezing
Diagnosis is often made through pulmonary function tests and imaging studies. Treatment options are limited, but may include immunosuppressive therapy and lung transplantation in severe cases.
Pulmonary Veno-Occlusive Disease
Pulmonary veno-occlusive disease (PVOD) is a rare but serious complication. It’s characterized by occlusion of the pulmonary veins. This can lead to pulmonary hypertension and right heart failure.
Symptoms include:
- Progressive dyspnea
- Fatigue
- Chest pain
Diagnosis is challenging and often requires a combination of imaging studies and histopathological examination. Treatment is largely supportive, and lung transplantation may be considered in eligible patients.
Understanding these pulmonary complications is key to managing patients with bone marrow transplants. Early recognition and proper treatment can greatly improve patient outcomes.
Hematologic Complications and Blood Count Issues
Bone marrow transplant patients face several blood-related problems. These can affect their blood counts and health. Issues can stem from the transplant type, the treatment used, and how the body reacts.
Persistent Cytopenias
Persistent cytopenias mean blood cell counts stay low for a long time. This can lead to anemia, neutropenia, and thrombocytopenia. Such conditions raise the risk of infections, bleeding, and feeling tired.
Managing cytopenias involves watching blood counts closely. Doctors may use growth factors to help blood cells grow. Sometimes, blood transfusions are needed to keep counts up.
Poor Graft Function
Poor graft function means the transplanted bone marrow doesn’t make enough blood cells. This can cause ongoing cytopenias and raise the risk of problems.
Things like graft rejection, viral infections, and some medicines can cause poor graft function. Doctors diagnose it through bone marrow biopsies and blood tests.
Secondary Graft Failure
Secondary graft failure is when a working graft stops making blood cells. This can happen months or years after the transplant.
Causes of secondary graft failure are similar to poor graft function. They include immune rejection and viral infections. Treatment might include immunosuppressive drugs, growth factors, or sometimes a second transplant.
| Complication | Causes | Management |
| Persistent Cytopenias | Conditioning regimen, graft dysfunction | Growth factors, transfusions |
| Poor Graft Function | Graft rejection, viral infections | Immunosuppressive therapy, growth factors |
| Secondary Graft Failure | Immune-mediated rejection, viral infections | Immunosuppressive therapy, second transplant |
Gastrointestinal Side Effects and Complications
Gastrointestinal side effects are a big worry for patients getting bone marrow transplants. These issues can really affect their quality and recovery. We’ll look at mucositis, digestive problems, and nutritional challenges.
Mucositis and Mouth Sores
Mucositis is common after bone marrow transplants. It causes painful mouth sores, making it hard to eat and drink. Managing mucositis well is key to avoiding malnutrition and dehydration. We suggest a detailed oral care plan, including gentle mouthwashes and pain relief.
Here are some ways to handle mucositis:
- Use topical anesthetics to ease pain
- Keep up with good oral hygiene
- Stay away from spicy or acidic foods
Digestive System Disruptions
The digestive system can face many challenges after a bone marrow transplant. Symptoms like nausea, vomiting, diarrhea, and stomach pain can occur. These can be due to the conditioning regimen, GVHD, or infections. We watch patients closely and use the right treatments.
Common digestive issues include:
- Graft-versus-host disease (GVHD)
- Infections like Clostridioides difficile (C. diff)
- Medications from the conditioning regimen
Nutritional Challenges
Nutritional challenges are a big worry for bone marrow transplant patients. Malnutrition can weaken the immune system, making recovery harder. We team up with nutritionists to create special diets for each patient.
Important nutritional points include:
- Make sure to get enough calories and protein
- Manage symptoms like nausea and diarrhea
- Use nutritional supplements when needed
By tackling these gastrointestinal issues, we can help patients do better and improve their quality during and after bone marrow transplants.
Secondary Malignancies: Long-term Cancer Risks
People who have had bone marrow transplants face a big challenge. They are at risk of getting secondary cancers years later. This is why it’s important to watch them closely and make sure they get the care they need.
Types of Secondary Cancers
After a bone marrow transplant, people can get different types of cancer. Myelodysplastic syndromes and acute myeloid leukemia are common. They can also get solid tumors like skin, breast, and thyroid cancers. This is more likely if they got total body irradiation before the transplant.
Risk Factors and Timeframes
Several things can increase the risk of getting secondary cancers. These include the treatment before the transplant, the patient’s age, and any genetic risks. The time it takes for these cancers to show up can vary a lot. Some can appear just a few years after the transplant, while others might take decades.
Knowing about these risks and timeframes helps doctors plan the best care for patients. For example, those who got total body irradiation might need closer monitoring.
Surveillance Recommendations
It’s very important for patients who have had bone marrow transplants to get regular check-ups. They should see a doctor who knows how to take care of transplant patients. This might include yearly skin checks, mammograms, and other tests based on their risk and medical history.
Also, teaching patients about the signs of secondary cancers helps them catch problems early. By watching closely and educating patients, we can find and treat these cancers sooner.
Recognizing Bone Marrow Transplant Failure Symptoms
Patients and doctors need to know the signs of bone marrow transplant failure. This condition can show itself in many ways, needing quick action. Spotting these signs early can help with treatment.
Declining Chimerism Levels
One sign of failure is when chimerism levels go down. Chimerism means both the patient’s and donor’s cells are in the body after a transplant. If donor chimerism drops, it might mean the graft is not working. It’s key to check chimerism levels often through blood tests.
Signs of Graft Loss
Graft loss happens when the transplanted bone marrow doesn’t make enough blood cells. This can cause problems like infections and bleeding. Patients might feel tired, have trouble breathing, or get sick easily because their immune system is weak.
When to Seek Immediate Medical Attention
Patients should know when to get help fast if they see signs of bone marrow transplant failure. Look out for severe infections, a lot of bleeding, or a big drop in blood cell counts. It’s important to watch your health closely and tell your doctor about any worries.
We know the fear of bone marrow transplant failure is real for patients. By staying alert and working with your healthcare team, you can handle any issues that come up.
Conclusion: Balancing Risks and Benefits of Bone Marrow Transplantation
Bone marrow transplantation is a complex procedure that can cure life-threatening diseases. But, it comes with big risks like graft-versus-host disease, infections, and organ damage.
We talked about the risks and side effects of bone marrow transplantation. This includes graft rejection, secondary malignancies, and long-term health issues. For example, autologous stem cell injections can lead to infections and pain at the site.
Even with these risks, bone marrow transplantation is a key treatment for many. Understanding the risks and benefits helps patients make better choices. It’s important to carefully choose patients, do thorough pre-transplant checks, and monitor them closely after.
In summary, bone marrow transplantation has big risks but can offer great benefits for many. By carefully balancing risks and benefits and providing detailed care, we can enhance patient outcomes and improve their quality of life.
FAQ
What are the risks associated with bone marrow transplant rejection?
Bone marrow transplant rejection is a big risk, mainly in allogeneic transplants. The recipient’s immune system attacks the donor cells. This can lead to graft failure and marrow aplasia.
What are the common side effects of a stem cell transplant?
Side effects include infections, organ damage, and graft-versus-host disease (GVHD). Patients may also feel tired, nauseous, and have low blood counts. They might experience pain and be more prone to infections.
What is graft-versus-host disease (GVHD), and how is it managed?
GVHD is when the donor’s immune cells attack the recipient’s tissues. It can be acute or chronic. Managing it involves immunosuppressive medications and supportive care.
What are the risks of infection after a bone marrow transplant?
Patients face risks of bacterial, viral, and fungal infections due to weakened immunity. Preventive measures include antimicrobial prophylaxis. Treatment involves quick action with the right antimicrobial therapy.
Can a bone marrow transplant cause organ damage?
Yes, it can cause organ damage. This includes liver, kidney, cardiac, and neurological effects. These are due to the conditioning regimen and immunosuppression.
What are the symptoms of bone marrow transplant failure?
Symptoms include declining chimerism levels and persistent cytopenias. Loss of engraftment and graft loss are also signs. Patients should seek immediate medical attention if they notice these symptoms.
Are there long-term cancer risks associated with bone marrow transplantation?
Yes, there’s a risk of secondary malignancies after bone marrow transplantation. Types, risk factors, and surveillance recommendations will be discussed with the healthcare provider.
What are the gastrointestinal side effects of a bone marrow transplant?
Side effects include mucositis, mouth sores, and digestive system disruptions. Nutritional challenges are also common. Management involves supportive care, nutritional support, and medications to alleviate symptoms.
How is bone marrow transplant rejection diagnosed?
Diagnosis involves monitoring chimerism levels, blood counts, and clinical symptoms. A bone marrow biopsy may be performed to assess graft function and detect rejection.
What are the complications of stem cell harvesting?
Complications include infection, pain at the harvest site, and bleeding. These risks are managed with proper care and follow-up.
What is the risk of pulmonary complications after a bone marrow transplant?
Pulmonary complications, such as idiopathic pneumonia syndrome, can occur. Symptoms and diagnosis involve imaging studies and pulmonary function tests.
Can autologous stem cell injections cause side effects?
Yes, autologous stem cell injections carry risks of infection and pain at the harvest site. Other complications related to the conditioning regimen and immunosuppression are also possible.
References
- Nauta, J., et al. (2013). Transfusion-induced bone marrow transplant rejection: mechanisms and clinical implications. Transfusion Medicine Reviews, 27(4), 214-223. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4284098/