Last Updated on November 17, 2025 by Ugurkan Demir

Bone marrow transplant side effects are an important consideration for patients undergoing this life-saving procedure. At Liv Hospital, we provide personalized care while keeping patients informed about potential side effects. Bone marrow transplants can cause immediate and long-term side effects due to high-dose chemotherapy, radiation, and the transplant itself. Common early side effects include fatigue, nausea, vomiting, hair loss, mouth and throat pain, infections, low blood counts, and graft-versus-host disease (GVHD) in allogeneic transplants, where donor cells attack the recipient’s tissues. Long-term complications may include chronic GVHD, infertility, secondary cancers, organ damage, cognitive issues, and chronic fatigue. Close monitoring and supportive care help manage these risks and improve outcomes.
A bone marrow transplant puts healthy stem cells into your body to replace bad bone marrow. This treatment works well, but it’s important to know the risks and complications it can bring.
We will cover 13 key risks and complications patients should know. This information helps you make better choices about your care.
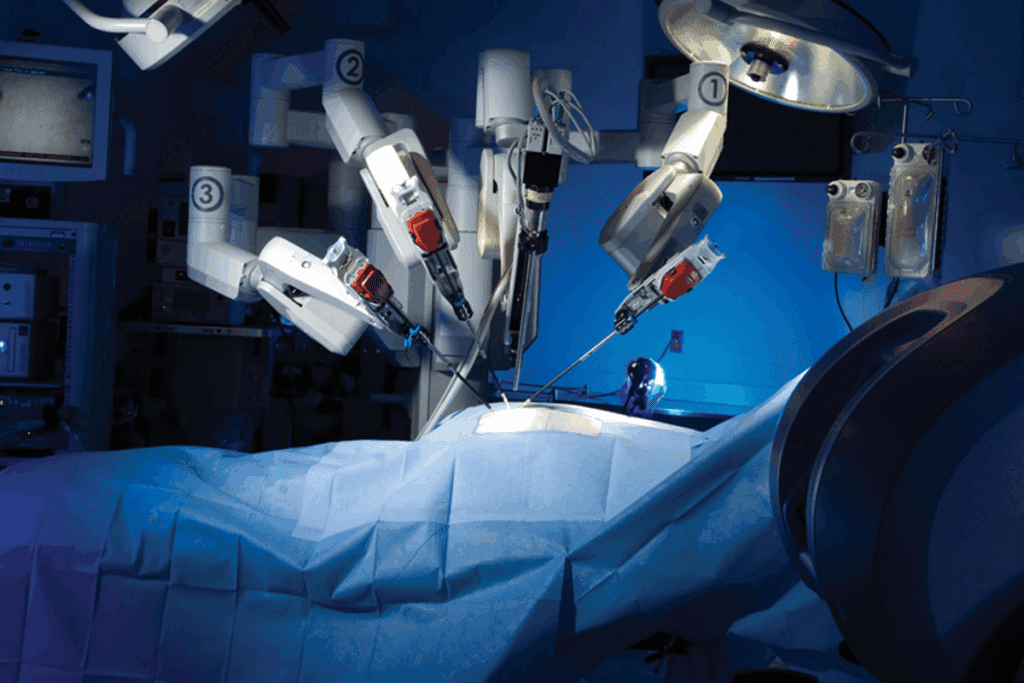
Bone marrow transplantation is a complex medical procedure. It replaces damaged or diseased bone marrow with healthy stem cells. This treatment is used for blood-related disorders like leukemia and lymphoma. The success of the transplant depends on several factors, including the type of transplant and the patient’s health.
There are two main types of bone marrow transplants: allogeneic and autologous. Allogeneic transplants use stem cells from a donor, often a sibling or unrelated donor. This type of transplant carries a risk of graft-versus-host disease (GVHD), where the donor’s immune cells attack the recipient’s tissues. On the other hand, autologous transplants use the patient’s own stem cells, collected, stored, and then reinfused after conditioning therapy. Autologous transplants eliminate the risk of GVHD but may have a higher risk of disease relapse.
The choice between allogeneic and autologous transplants depends on several factors, including the underlying disease, the patient’s overall health, and the availability of a suitable donor. We will discuss the specifics of each type and its implications for patient care.
The bone marrow transplant process starts with conditioning therapy. This involves high-dose chemotherapy and/or radiation to destroy the patient’s existing bone marrow and any remaining cancer cells. After conditioning, the patient receives the stem cell infusion, which is similar to a blood transfusion. The infused stem cells then migrate to the bone marrow, where they begin to produce new blood cells.
The transplant process carries several risks, including infections, bleeding, and organ damage. Patients undergoing bone marrow transplants are at a higher risk of developing infections due to their compromised immune systems. Other complications include graft failure, GVHD, and long-term side effects such as secondary malignancies and fertility issues.
In summary, bone marrow transplantation is a complex procedure that requires careful consideration of the type of transplant and the associated risks. Understanding the differences between allogeneic and autologous transplants, as well as the transplant process, is key for patients to make informed decisions about their care.
The pre-transplant conditioning process uses high-dose chemotherapy and sometimes radiation. It’s key to get the body ready for a bone marrow transplant. This method kills any cancer cells left and weakens the immune system to stop it from rejecting the new marrow.
High-dose chemotherapy is a main part of the conditioning. It works well to kill cancer cells but has side effects. These include nausea and vomiting, which can be treated with medicines, and fatigue, which can last for a while after treatment.
Another big issue is how it affects the body’s blood-making abilities. It can lower the production of red and white blood cells and platelets. This leads to anemia, more infections, and bleeding problems.
For some, radiation therapy is also used in the conditioning, mainly for localized cancers or to weaken the immune system further. Radiation can cause side effects based on where it’s aimed. Common ones are fatigue, skin reactions at the radiation site, and damage to organs if they’re in the radiation area.
Both chemotherapy and radiation can also have long-term effects. These can include problems with fertility, a higher risk of getting secondary cancers, and damage to the heart, lungs, and other organs. Knowing these long-term side effects is important for patients to make good choices about their care.
We know that a bone marrow transplant is a tough and complex process. Our team is dedicated to giving full care and support. We aim to help manage the side effects of pre-transplant conditioning and get the best results for our patients.
Patients going through bone marrow transplants face tough times in the first 30 days. They need to watch out for several side effects. The body’s fight against infections is weakened because of the treatment and the transplant itself. We’ll look at the main risks during this important time.
In the first 30 days after a bone marrow transplant, infections are a major concern. The treatment before the transplant weakens the immune system. This makes patients very likely to get sick. The main reasons for this risk are:
Graft failure is another big risk in the first 30 days after the transplant. This happens when the new bone marrow doesn’t make enough blood cells, or when the body rejects it. Graft failure can lead to severe complications, including:
In conclusion, the first 30 days after a bone marrow transplant are critical. Patients are at a heightened risk of infections and graft failure, among other complications. Understanding these risks is key to managing expectations and ensuring the best possible outcomes.
After a bone marrow transplant, patients often face blood-related complications. These can affect their recovery a lot. We will talk about anemia, thrombocytopenia, and neutropenia risks.
Anemia is when you have too few red blood cells. This leads to extreme fatigue, weakness, and shortness of breath. The conditioning regimen, which includes chemotherapy and/or radiation, can cause this.
To fight anemia, patients might need blood transfusions. They might also get medicines to help make more red blood cells. It’s important to tell your doctor if you feel anemic.
Thrombocytopenia is when you have too few platelets. This can cause bleeding problems. Platelets help blood clot, and without enough, you might bruise easily or have nosebleeds.
Neutropenia is when you have too few neutrophils. Neutrophils fight infections. After a bone marrow transplant, you might get neutropenia, making you more likely to get infections.
To lower this risk, patients often stay isolated. They might also get antibiotics to prevent infections. Keeping an eye on neutrophil counts and treating infections quickly is key.
Knowing about these blood-related complications and how to manage them is important for bone marrow transplant patients. By understanding the risks and taking steps to prevent them, patients can improve their recovery.
Getting a bone marrow transplant can really mess with your stomach. Patients often face many digestive problems. This is because the treatment, which includes strong chemotherapy and sometimes radiation, can hurt the stomach lining.
Mucositis is a big problem for those getting a bone marrow transplant. It causes painful sores in the mouth and throat. This happens because the treatment damages the mucous membranes, causing inflammation and ulcers.
Nutritional Impact: Having mucositis makes it hard to eat and drink. This can lead to malnutrition and dehydration if not handled properly.
Severe diarrhea and intestinal inflammation are big risks after a bone marrow transplant. The treatment can hurt the intestinal lining, causing inflammation and irritation.
Consequences: Bad diarrhea can cause dehydration, electrolyte imbalances, and malnutrition. This makes recovery even harder.
Patients need to get the right food after a bone marrow transplant. Good nutrition helps with healing, fighting off infections, and keeping overall health up.
We suggest eating foods high in protein, vitamins, and minerals. Some patients might need enteral nutrition or parenteral nutrition if they can’t eat normally.
| Nutritional Challenge | Impact on Recovery | Management Strategy |
| Mucositis | Painful eating, risk of malnutrition | Soft, bland diet; pain management |
| Severe Diarrhea | Dehydration, electrolyte imbalance | Fluid replacement, electrolyte supplements |
| Intestinal Inflammation | Malabsorption, weight loss | Anti-inflammatory medication, nutritional supplements |
Knowing about these digestive and nutritional problems helps us deal with bone marrow transplant side effects better. This way, we can support patients more during their recovery.
After a bone marrow transplant, patients face a risk of graft-versus-host disease (GVHD). This is when the donor’s immune cells attack the recipient’s body. GVHD is a serious condition, often seen in allogeneic transplants.
Acute GVHD happens within the first 100 days after the transplant. It can show up in different ways, such as:
We treat acute GVHD with medicines to stop the donor cells from attacking the recipient’s body.
Chronic GVHD can start after 100 days and last for months or years. Its symptoms are similar to acute GVHD, but can also include:
Managing chronic GVHD is long-term and can greatly affect a patient’s quality.
To prevent GVHD, we use several methods, including:
We also watch patients closely for GVHD signs and adjust their treatment as needed. Sometimes, extra treatments are needed to manage GVHD well.
Organ damage is a big risk after a bone marrow transplant. It can harm many parts of the body. The high doses of chemotherapy and radiation used can also cause side effects.
Liver and kidney problems can happen after a bone marrow transplant. The liver helps clean the body, and the kidneys filter waste. Chemotherapy and radiation can damage these organs, leading to problems.
The liver can get blocked, causing liver failure. Kidney issues can come from certain medicines, like antibiotics and immunosuppressants, needed after a transplant.
Heart and lung problems can also occur after a bone marrow transplant. The treatment before the transplant can harm these organs. This can lead to heart failure and lung scarring.
Heart issues can include irregular heartbeats, weak heart function, or even heart failure. Lung problems can cause infections, inflammation, or scarring. This makes it hard to breathe and get enough oxygen.
Fluid overload and electrolyte imbalances are also systemic complications. The use of IV fluids, medicines, and nutrition can upset the balance of important electrolytes like sodium, potassium, and calcium.
It’s important to watch and manage fluid levels to avoid heart and lung problems. Electrolyte imbalances can cause muscle weakness, heart rhythm issues, and other serious problems. This shows why it’s key to monitor and act quickly.
After a bone marrow transplant, patients face new challenges that can affect their health and quality. The transplant can save lives, but it’s important to know and manage long-term side effects.
One big risk after a bone marrow transplant is secondary malignancies. These cancers come from the transplant or treatments like chemotherapy and radiation. It’s key to watch for these cancers and manage them. Studies show the risk of secondary malignancies can vary, making long-term care important.
“The development of secondary cancers is a well-recognized complication of hematopoietic stem cell transplantation,” as noted in medical literature. This shows why regular check-ups and screenings are vital for patients after a transplant.
Fertility problems are another side effect of bone marrow transplants. The treatments before the transplant can harm reproductive organs, leading to infertility. Talking to a healthcare provider about fertility options before the transplant is important.
Endocrine problems, like thyroid issues and adrenal insufficiency, can also happen. These might need lifelong hormone therapy. It’s key to manage these issues to keep patients healthy and improve their quality of life.
Cognitive changes, or “chemo brain,” can affect memory, focus, and speed. The exact cause is not known, but chemotherapy and radiation are thought to play a role. Rehabilitation and cognitive training can help lessen these effects.
The mental impact of a bone marrow transplant is significant. Patients might feel anxious, depressed, or have PTSD. Having a strong support system, including mental health experts, is critical.
In summary, while a bone marrow transplant can save lives, it comes with long-term side effects that can affect quality of life. Knowing these risks and working with healthcare providers can help manage them. This can improve outcomes for those who have had a transplant.
It’s key for patients to know the risks of bone marrow transplants to manage life after treatment. After a transplant, patients need ongoing care to handle possible complications. This includes complications of stem cell transplant and side effects of stem cell harvesting, to improve their quality.
We’ve talked about the risks of bone marrow transplants. These range from side effects before the transplant to long-term issues like stem cell treatment side effects and side effects of a stem cell transplant. It’s vital for patients to know these risks to get help quickly.
With ongoing care, healthcare teams can quickly tackle any new problems. This helps improve patient results. Knowing the risks of bone marrow transplants helps patients navigate their recovery better. It helps them achieve the best life quality possible.
Common side effects include infections and graft failure. Other issues are anemia, thrombocytopenia, and neutropenia. Mucositis, diarrhea, and intestinal inflammation are also common. These problems can happen in the first 30 days and may last longer.
Allogeneic transplants use stem cells from a donor. Autologous transplants use the patient’s own stem cells. Allogeneic transplants have a higher risk of GVHD. Autologous transplants have a lower risk of GVHD but may have a higher risk of relapse.
Pre-transplant therapy can cause nausea, vomiting, and fatigue. It can also lead to hair loss. These treatments can cause long-term problems like infertility and secondary malignancies.
GVHD can be prevented or managed with immunosuppressive medications. Careful donor selection and monitoring are also important. Acute GVHD usually happens within 100 days. Chronic GVHD can occur later and may need ongoing treatment.
Long-term side effects include secondary malignancies and fertility issues. Endocrine dysfunction and cognitive changes are also possible. Patients may also experience chronic GVHD or organ damage.
Patients can manage digestive issues by eating healthy and staying hydrated. Avoiding irritating foods is also helpful. Nutritional support may be needed to ensure proper nutrition during recovery.
Patients are at risk of infections due to weakened immunity. Infections can be severe or life-threatening. Prophylactic antibiotics or antiviral medications may be needed to prevent infections.
Some side effects can be predicted based on individual risk factors. Others may not be preventable. Monitoring and managing side effects can help minimize their impact and improve outcomes.
Ongoing care and monitoring are key to managing complications and improving outcomes. Regular follow-up appointments can help identify and address issues promptly. This reduces the risk of long-term side effects.
Autologous stem cell injection carries risks like infection and pain. Complications related to the procedure can also occur. Patients should discuss the risks and benefits with their healthcare provider.
Complications include graft failure, GVHD, and infections. Organ damage and long-term side effects like secondary malignancies and fertility issues are also possible. Patients should be aware of these risks and work closely with their healthcare team.
Stem cell harvesting is generally safe but can cause side effects like pain and bruising. Fatigue is also possible. Patients should discuss the risks and benefits with their healthcare provider.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!