Last Updated on November 26, 2025 by Bilal Hasdemir
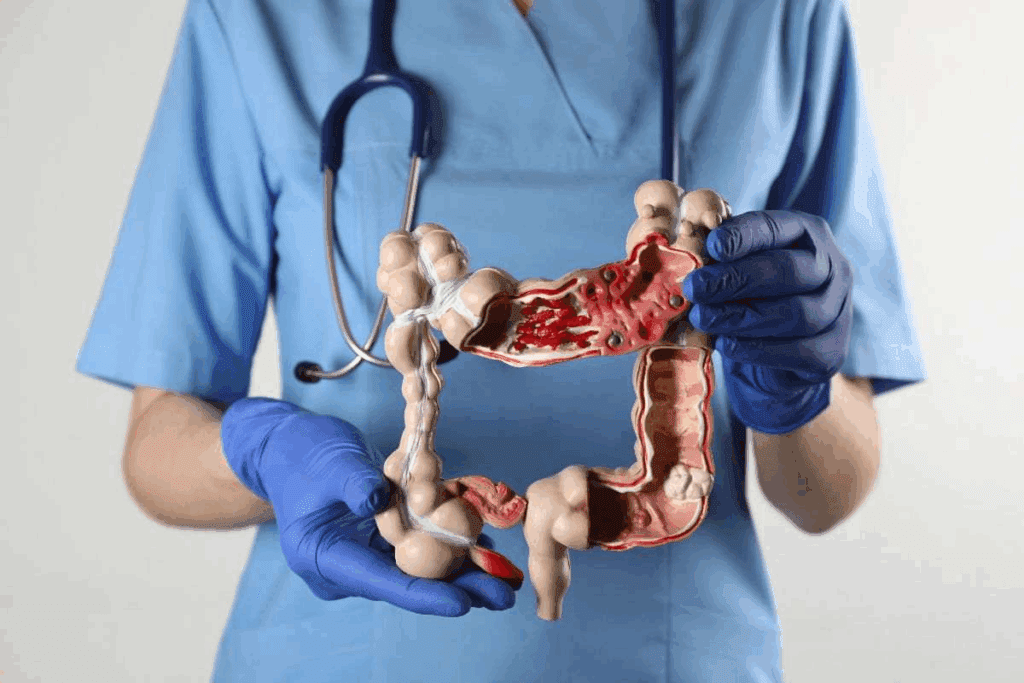
It’s vital to know the main bowel tumor removal options for those with colorectal cancer. Liv Hospital focuses on the latest methods and puts patients first. This means patients get the best surgery for colorectal cancer to help them heal well. Explore the 9 main bowel tumor removal surgeries for colorectal cancer treatment.
The choice of colon cancer surgery varies based on the tumor’s location and size. Different methods are used for the colon and rectum. These bowel operation types help remove cancer and boost survival chances.
Key Takeaways
- Various surgical techniques are available for treating colorectal cancer.
- The type of surgery depends on the cancer’s position and size.
- Liv Hospital offers advanced and patient-centered surgical options.
- Different surgeries are used for the colon and rectum.
- Effective bowel tumor removal surgery improves survival rates.
The Role of Surgery in Colorectal Cancer Treatment

Surgery is key in treating colorectal cancer, giving hope to many. The success of surgery depends on the tumor’s stage and location.
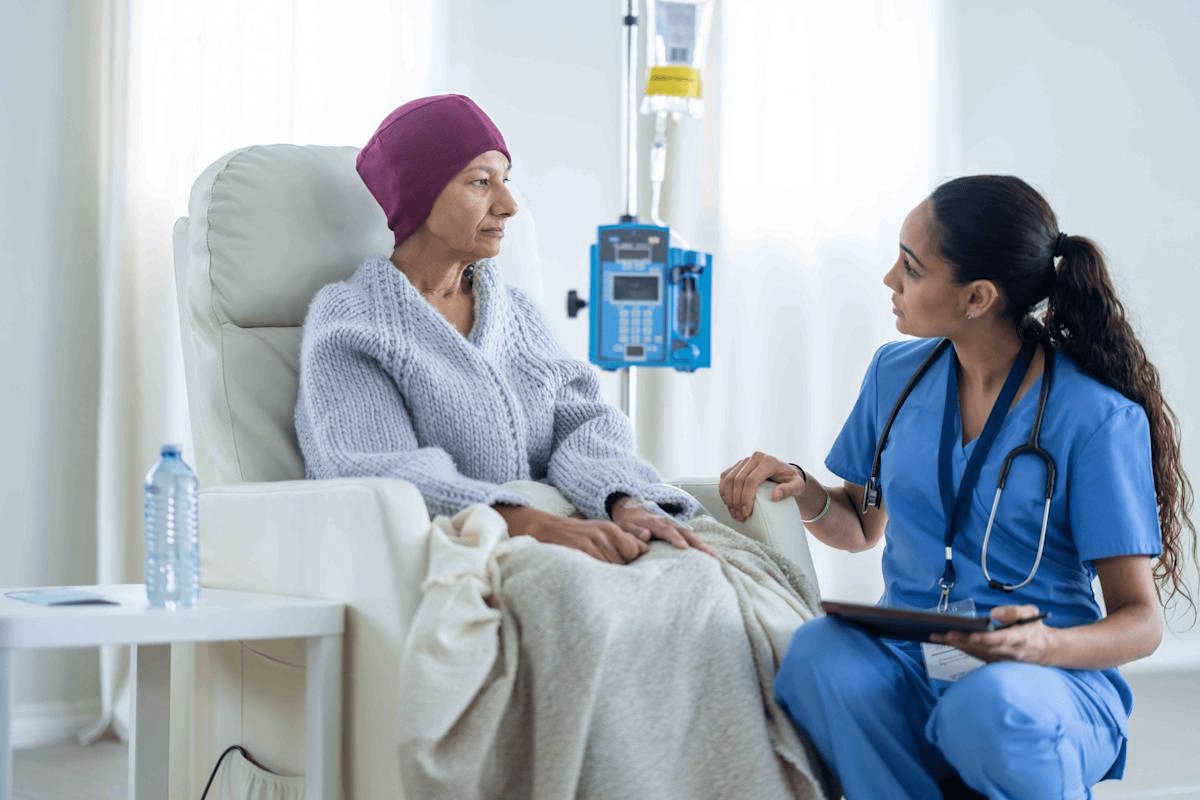
The Prevalence and Impact of Colorectal Cancer
Colorectal cancer is a common cancer worldwide, affecting millions yearly. In the U.S., tens of thousands are diagnosed each year. It impacts not just the patient but also their families and communities.
This highlights the need for good treatments. Surgery is a mainstay in treating colorectal cancer. It can cure early-stage cancer.
Why Surgical Intervention Remains Essential
Surgery is vital for removing the tumor and affected bowel parts. The surgery type varies with the cancer’s location and stage. For example, right hemicolectomy is used for ascending colon tumors, and low anterior resection for rectal cancer.
The surgical method, open, laparoscopic, or robotic, depends on the patient’s health and disease extent. Minimally invasive methods are gaining favor for quicker recovery and less scarring.
Pre-Surgical Evaluation and Planning
Before surgery, patients undergo detailed evaluations. This includes CT scans, MRI, blood tests, and more. It assesses their health and disease extent.
Planning is key to choosing the right surgery. A team of doctors, including surgeons and oncologists, creates a personalized plan. They consider the patient’s needs and the tumor’s specifics.
Right Hemicolectomy: Treating Ascending Colon Cancer
Removing the right colon is a common treatment for ascending colon cancer. This surgery takes out the cancerous area, some healthy tissue, and nearby lymph nodes.
Procedure Overview and Anatomical Considerations
A right hemicolectomy needs a good understanding of the colon’s layout. The ascending colon is on the right side of the abdomen. Surgeons must carefully avoid damaging important structures.
Key anatomical considerations include:
- The ileocolic vessels and their branches
- The right colic vessels
- The middle colic vessels
- The ileocecal junction
Open vs. Minimally Invasive Techniques
Right hemicolectomy can be done open or minimally invasive. The choice depends on the patient’s health, cancer stage, and the surgeon’s skill.
| Surgical Approach | Characteristics | Benefits |
| Open Surgery | Large incision in the abdomen | Direct visualization, potentially less complex equipment required |
| Minimally Invasive Surgery | Several small incisions, laparoscopic or robotic assistance | Less post-operative pain, quicker recovery, smaller scars |
Recovery Timeline and Post-Operative Care
Recovery time after a right hemicolectomy varies. Patients usually stay in the hospital for a few days. Care includes watching for complications, managing pain, and slowly getting back to normal.
Post-operative care tips:
- Follow the surgeon’s instructions regarding wound care and medication.
- Gradually increase physical activity as advised by the healthcare team.
- Attend follow-up appointments to monitor healing and address any concerns.
Left Hemicolectomy: Addressing Descending Colon Tumors
The left hemicolectomy procedure removes the part of the colon with the tumor. It then reconnects the rest of the bowel. This surgery is key to treating tumors in the descending colon.
Surgical Technique and Lymph Node Removal
During a left hemicolectomy, the surgeon carefully removes the affected colon segment and lymph nodes. Removing lymph nodes is vital for cancer staging and deciding on further treatments.
Lymph node removal is a key part of the procedure. It helps determine how far the cancer has spread. The surgeon aims to remove enough lymph nodes for accurate staging.
Indications and Patient Selection
Left hemicolectomy is for patients with tumors in the descending colon. The decision to do this surgery depends on several factors. These include the cancer stage, the patient’s health, and any other health conditions.
Patients with early-stage colon cancer may benefit from this surgery. It offers a chance for a cure. In more advanced cases, it might be part of a treatment plan that includes chemotherapy and radiation.
| Indication | Description |
| Tumor Location | Descending colon tumors |
| Cancer Stage | Early-stage to advanced colon cancer |
| Patient Health | Patients with acceptable surgical risk |
Potential Complications and Management
Like any surgery, left hemicolectomy has risks and complications. These can include infection, bleeding, and leakage at the surgical site. Surgeons use antibiotics and careful technique to reduce these risks.
If complications happen, quick action is needed. For example, leakage might need immediate surgery or endoscopic treatment.
Good post-operative care is key fotonaging complications and helping patients recover. Patients are watched closely for any signs of trouble. They get the support and treatment they need.
Sigmoid Colectomy for Distal Colon Cancer
Distal colon cancer treatment often involves sigmoid colectomy. This is a procedure where the surgeon removes the sigmoid colon. They then reconnect the remaining colon to the rectum. This surgery is key for patients with cancer in the distal colon.
Procedure Details and Surgical Approaches
Sigmoid colectomy can be done in different ways. This includes open surgery and minimally invasive techniques like laparoscopy. The choice depends on the cancer stage, the ent’s health, and the surgeon’s skills.
Key steps in sigmoid colectomy include:
- Removal of the sigmoid colon along with the tumor
- Dissection and removal of regional lymph nodes
- Reconnection of the remaining colon to the rectum
Advantages of Laparoscopic Sigmoid Resection
Laparoscopic sigmoid resection has many benefits. It uses smaller incisions, leading to less pain and shorter hospital stays. This approach is great for patients who can handle it, as it lowers the risk of complications and improves recovery.
The benefits of laparoscopic sigmoid resection are:
- Reduced trauma to the body
- Less post-operative pain
- Faster return to normal activities
Post-Operative Recovery and Bowel Function
After a sigmoid colectomy, patients need time to recover. They might see changes in bowel function. These changes depend on the extent and patient factors.
Post-operative care involves:
- Monitoring for complications
- Managing pain effectively
- Gradually returning to a normal diet and activities
Knowing what to expect can help patients prepare for a sigmoid colectomy. It can lead to better outcomes.
Low Anterior Resection for Rectal Cancer
Rectal cancer treatment has changed a lot. Low anterior resection is now a key surgery. It aims to remove tumors while keeping the bowel working well.
Technical Aspects and Sphincter Preservation
Low anterior resection removes the cancerous part of the rectum. Then, the rest of the rectum is connected to the colon. Keeping the sphincter intact is key to normal bowel function.
Surgeons use special techniques to save the sphincter. They check for clear margins during surgery. This ensures the cancer is fully removed.
“The goal is to remove the cancer and keep the patient’s bowel function,” says a top colorectal surgeon. This requires careful planning and skill.
Neoadjuvant Therapy Considerations
For many, neoadjuvant therapy is vital before surgery. It shrinks tumors, making them easier to remove. Therapy can be radiation, chemotherapy, or both.
The choice of therapy depends on the cancer’s stage and the patient’s health. It’s a complex decision.
Managing Low Anterior Resection Syndrome
After a low anterior resection, some patients face low anterior resection syndrome (LARS). Symptoms include bowel problems and urgency. Managing LARS needs a team effort.
“Understanding and addressing LARS is key for better patient quality of life,” says a colorectal surgery expert.
With a detailed care plan, including counseling and support, LARS can be managed. This improves patient outcomes.
Comprehensive Bowel Tumor Removal: Total Colectomy
Total colectomy is a big surgery to remove the whole colon. It’s often chosen for certain colorectal issues. This method is used when the disease covers the whole colon or when other treatments fail.
Indications for Complete Colon Removal
Several conditions lead to total colectomy. For example, familial adenomatous polyposis (FAP) causes many polyps in the colon. Other reasons include:
- Severe colorectal cancer in many parts of the colon
- Inflammatory bowel disease (IBD) that can’t be treated with medicine
- Multiple colon cancers at the same time
Choosing total colectomy requires careful thought. It depends on the patient’s health and recovery chances.
Surgical Technique and Reconstruction Options
The surgery removes the colon from start to finish. It can be done openly or with small incisions, based on the patient and surgeon.
After taking out the colon, the surgeon decides how to rebuild. Options include:
| Reconstruction Option | Description | Considerations |
| Ileorectal Anastomosis | Connecting the small intestine to the rectum | Keeps some normal bowel function but needs ongoing checks |
| Ileal Pouch-Anal Anastomosis (IPAA) | Creates a pouch in the small intestine for stool | More complex, might reduce bowel movements |
| Ileostomy | Makes an opening in the abdomen for waste | Needed for some, requires managing an ostomy bag |
Adapting to Life After Total Colectomy
Life after total colectomy changes a lot. Patients must get used to new bowel habits and possibly manage an ostomy or pouch. Eating differently is also key to feeling better and staying healthy.
Important things for aftercare include:
- Watching for problems like infection or blockage
- Handling bowel movements and possible incontinence
- Changing diet to ease symptoms and keep nutrition up
With the right care and support, many people live well after total colectomy. Regular check-ups with doctors are vital to catch any problems early and watch for disease return.
Local Excision Techniques for Early-Stage Tumors
Local excision techniques have changed how we treat early-stage bowel tumors. They allow for tumor removal through small incisions. This method cuts down on recovery time and keeps more of the bowel’s natural function.
Transanal Excision and Endoscopic Approaches
Transanal excision removes tumors through the anus with special tools. It works well for tumors in the lower rectum. Endoscopic approaches use a flexible tube with a camera and tools to remove tumors. These methods are less invasive and lead to faster recovery.
Choosing between transanal excision and endoscopic approaches depends on the tumor’s size, location, and stage. Advanced imaging techniques help decide the best method.
Patient Selection and Oncological Outcomes
Choosing the right patient for local excision is key. The tumor’s stage, grade, and lymphovascular invasion are checked. Early-stage tumors with good characteristics are usually good candidates.
Patients with local excision often have good outcomes. They have high rates of local control and survival. But close monitoring is needed to catch any recurrence early.
Follow-Up and Surveillance Requirements
After local excision, follow-up care is vital. It helps watch for recurrence and any complications. Regular endoscopic examinations and imaging studies are usually advised. The schedule and length of follow-up depend on the patient and their tumor.
Surveillance plans often include colonoscopy, CT scans, and MRI. These help find any recurrence or spread early. This allows for quick action.
Abdominoperineal Resection for Low Rectal Cancers
Abdominoperineal resection is a major surgery for low rectal cancers. It removes the anus, rectum, and part of the sigmoid colon. This can be a cure for those with this tough condition.
Understanding This Radical Procedure
Abdominoperineal resection, or APR, is used when tumors are near the anus. It’s done through the abdomen and perineum. This way, surgeons can remove the tumor and affected lymph nodes.
Choosing APR is made after careful checks, like scans and tumor assessments. The team looks at the cancer’s stage, the patient’s health, and whether they can keep the sphincter.
Permanent Stoma Creation and Management
APR means a permanent colostomy. Without an anus and a rectum, waste goes through a stoma. Learning to care for the stoma is key.
Patients get help with stoma care, like changing the appliance and spotting problems. Nurses and other healthcare teams offer vital support for adjusting to life with a stoma.
Quality of Life and Psychological Considerations
APR changes a patient’s life in many ways. It saves lives but also means losing normal bowel function and getting a stoma. Mental support is vital for coping with these changes.
Research shows many patients live well after APR with the right support. Counseling before surgery, good care after, and ongoing support are key to recovery and adjustment.
Advanced Surgical Approaches to Bowel Tumor Removal
New surgical technologies have made bowel tumor removal easier and faster. Now, patients can have less invasive surgeries with quicker recovery times. Techniques like robotic-assisted and laparoscopic surgery are becoming more common for treating colorectal cancer.
Robotic-Assisted Colorectal Surgery
Robotic-assisted surgery is a big step forward in colorectal surgery. It uses a robotic system to help surgeons. This system offers high-definition 3D views and precise tools.
It makes surgeries more precise and detailed. This can lead to better results for patients with colon cancer operation procedures.
Robotic surgery also means less blood loss, less pain, and shorter hospital stays. The robotic system’s dexterity helps in removing tumors more accurately. This could improve cancer treatment outcomes.
Laparoscopic Techniques and Benefits
Laparoscopic surgery is done through small cuts in the abdomen. It’s used for many colorectal procedures, like bowel resection for cancer. This method has many benefits over traditional surgery.
It causes less damage to tissues, less pain, and faster healing. Studies show patients recover faster and have less chance of complications.
Also, the small cuts reduce the risk of infection and improve how the scars look.
Comparing Recovery Between Traditional and Minimally Invasive Approaches
Traditional open surgery and minimally invasive methods like laparoscopic and robotic surgery have different recovery times. Minimally invasive surgeries usually mean less pain, fewer complications, and quicker healing.
| Recovery Aspect | Traditional Open Surgery | Minimally Invasive Surgery |
| Hospital Stay | Typically 5-7 days | Often 2-4 days |
| Recovery Time | 6-8 weeks | 3-6 weeks |
| Pain Level | Higher | Lower |
| Risk of Complications | Higher | Lower |
The table shows the benefits of minimally invasive surgery over traditional open surgery for to removal of colon cancer. While not all patients can have these surgeries, those who do often recover faster and with less pain.
Conclusion: The Future of Colorectal Cancer Surgery
The way we treat colorectal cancer is changing. There are many colorectal cancer surgery types now. This gives patients more choices for bowel tumour removal.
Each surgery has its own uses and benefits. For example, right hemicolectomy and left hemicolectomy are used for different types of tumors. Sigmoid colectomy and low anterior resection are also options. Total colectomy, local excision, and abdominoperineal resection have their own roles too.
New ways to do colon surgeries are making things better. Laparoscopic and robotic techniques are leading the way. They make recovery faster, scars smaller, and risks lower.
The future of colorectal cancer surgery is bright. With new technologies and techniques, we can do even better. Keeping up with these advancements is key to beating colorectal cancer.
FAQ
What is bowel tumor removal surgery?
Bowel tumor removal surgery, also known as bowel resection, is a procedure to remove tumors in the bowel. This includes the colon and rectum.
What are the different types of bowel tumor removal surgery?
There are several types of bowel tumor removal surgery. These include right hemicolectomy, left hemicolectomy, and sigmoid colectomy. Others are low anterior resection, total colectomy, local excision techniques, and abdominoperineal resection.
What is the role of surgery in treating colorectal cancer?
Surgery is key in treating colorectal cancer. It removes the tumor anthe d affected bowel part. This helps stop cancer spread and improves patient outcomes.
What is a right hemicolectomy?
Right hemicolectomy is a surgery for ascending colon cancer. It removes the right colon side.
What is the difference between open and minimally invasive surgical techniques?
Open surgery uses a big incision. Minimally invasive surgery, like laparoscopic or robotic-assisted, uses small incisions. This causes less tissue damage and faster recovery.
What is a sigmoid colectomy?
Sigmoid colectomy treats distal colon cancer. It removes the sigmoid colon.
What is a low anterior resection?
Low anterior resection treats rectal cancer. It removes the tumor while keeping the sphincter muscles.
What is a total colectomy?
Total colectomy removes the whole colon. It’s often for conditions like familial adenomatous polyposis.
What are local excision techniques?
Local excision techniques, like transanal excision and endoscopic approaches, remove early-stage tumors. They preserve tissue and bowel function.
What is abdominoperineal resection?
Abdominoperineal resection treats low rectal cancers. It removes the tumor, rectum, and anus, creating a permanent stoma.
What are the benefits of robotic-assisted and laparoscopic techniques in bowel tumor removal surgery?
Robotic-assisted and laparoscopic techniques reduce blood loss and post-operative pain. They also lead to faster recovery than open surgery.
How is patient selection determined for different types of bowel tumor removal surgery?
Patient selection depends on tumor location, size, and stage. It also considers the patient’s health and medical history.
What are the possible complications of bowel tumor removal surgery?
Complications include infection, bleeding, bowel obstruction, and anastomotic leakage. These are among the possible risks.
What is the recovery process like after bowel tumor removal surgery?
Recovery varies by surgery type and patient. It involves rest, pain management, and follow-up care to watch for complications.
How does bowel tumor removal surgery impact quality of life?
Surgery can greatly affect quality of life. Some procedures change bowel function, while others may require a permanent stoma.
References
- U.S. Food and Drug Administration. (2022). Innovations in minimally invasive colorectal surgery. https://www.fda.gov/medical-devices/innovation-initiative