Last Updated on December 1, 2025 by Bilal Hasdemir

Trauma neurosurgery is a very specialized field. It deals with life-threatening neurological emergencies. Every year, thousands of people in the United States get traumatic brain injuries that need surgery right away. What is brain injury surgery? We explore the critical role of a trauma neurosurgeon in treating TBI patients. Get the essential details.
A trauma neurosurgeon’s job is very important. They have to make quick decisions to save lives. These doctors go through a lot of training to learn how to handle traumatic head injuries.
Key Takeaways
- Trauma neurosurgeons specialize in surgical interventions for life-threatening neurological emergencies.
- Their expertise is critical in treating traumatic brain injuries.
- Rigorous training is required to become a skilled trauma neurosurgeon.
- Trauma neurosurgery involves making rapid decisions in high-pressure situations.
- Understanding the role of trauma neurosurgeons can help appreciate the complexity of their work.
The Role of a Trauma Neurosurgeon

In neurosurgery, trauma specialists are key for acute brain traumas and emergencies. They are highly skilled and play a critical role in emergency care.
They make quick decisions in high-pressure situations, where lives are at stake. Their role is complex, needing a deep understanding of neurosurgery and quick application in emergencies.
Specialized Focus on Neurological Emergencies
Trauma neurosurgeons handle many neurological emergencies, like traumatic brain injuries and spinal cord injuries. They provide focused care in critical times.
They perform complex surgeries under pressure, often with little time to plan. This demands technical skill and calm in chaotic settings.
Differences Between General and Trauma Neurosurgery
General neurosurgery covers many conditions, but trauma neurosurgery focuses on acute injuries. Trauma neurosurgeons must respond to severe trauma with speed and decisiveness.
Unlike general neurosurgery, which may include elective procedures, trauma neurosurgery is urgent. This highlights the unique challenges and rewards of being a trauma neurosurgeon.
Educational Path and Training Requirements
Trauma neurosurgery is a highly specialized field that requires a lot of education. To become a neurosurgeon for brain injury, one must commit to many years of study and training.
Medical School and Neurosurgical Residency
It starts with four years of medical school. Here, future neurosurgeons learn about human anatomy, physiology, and disease. Then, they enter a neurosurgical residency program, lasting six to seven years.
In this program, they learn about advanced brain injury treatment and more. They get hands-on experience under the watchful eyes of seasoned neurosurgeons. They help with patient care, surgeries, and research, improving their skills and knowledge.
Fellowship Training in Trauma Neurosurgery
After residency, those wanting to specialize in trauma neurosurgery do fellowship training. This can take one to two years. It focuses on the details of treating traumatic brain and spinal injuries.
Fellows work with top trauma neurosurgeons. They learn the newest surgical methods and advanced brain injury treatment strategies. This training is key for mastering complex trauma cases.
In summary, becoming a trauma neurosurgeon is a long and demanding journey. It involves a lot of neurosurgical training. But, it prepares these doctors to save lives by treating severe brain injuries.
Brain Injury Surgery: Core Procedures and Techniques
The complexity of brain injury surgery requires a detailed approach. Neurosurgeons use various techniques based on the injury type. They must be skilled in many procedures to treat different traumatic brain injuries well.
Types of Traumatic Brain Injuries Requiring Surgical Intervention
Traumatic brain injuries (TBI) needing surgery vary in how they appear and how severe they are. Some common types include:
- Epidural hematomas, which are bleeding between the skull and the outer brain layer.
- Subdural hematomas, where bleeding is between the outer and inner brain layers.
- Intracerebral hemorrhages, bleeding inside the brain tissue.
- Depressed skull fractures, which may need surgery to lift the skull and relieve brain pressure.
Evidence-Based Surgical Approaches for Different Brain Traumas
The choice of surgical options for brain injury depends on several factors. These include the injury type and severity, and the patient’s overall health. Evidence-based surgical methods include:
- Craniotomy, which temporarily removes a skull part to access the brain.
- Decompressive craniectomy, removing part of the skull to let a swollen brain expand.
- Hematoma evacuation, removing blood clots that press on the brain.
These traumatic brain injury treatment strategies are always improving. Ongoing research aims to better outcomes for patients with severe brain injuries.
Emergency Response and Initial Assessment
When a patient with a severe head injury arrives at the emergency department, the team acts fast. They do a quick check of the patient’s brain function.
This check is key to figuring out how bad the injury is and what to do first.
Rapid Neurological Evaluation in the Trauma Bay
In the trauma bay, a head trauma specialist starts the quick brain check. They look at how awake the patient is, the size and reaction of their pupils, and how well their limbs move.
The aim is to spot any urgent problems that need quick action.
The team uses the Glasgow Coma Scale (GCS) to check the patient’s brain function. This scale looks at eye opening, talking ability, and movement. A low score means a serious brain injury. Quick and correct checks are vital for sorting patients and using the right resources.
Critical Decision-Making in the Golden Hour
The first hour after a brain injury is called the “golden hour.” Decisions made in this time can greatly affect the patient’s recovery.
Decisions about emergency brain surgery are based on the first check, scans like CT scans, and how the patient is doing.
Trauma neurosurgeons must think about the benefits and risks of surgery. They consider how bad the injury is, if there are other serious problems, and the patient’s overall health.
Good communication with the trauma team is key for smooth care and making smart choices.
Craniotomy Procedures for Acute Head Trauma
Craniotomy for acute head trauma is a complex surgery. It requires careful planning and execution. The surgery involves opening the skull to relieve pressure, repair blood vessels, or remove damaged brain tissue.
Surgical Indications and Preoperative Planning
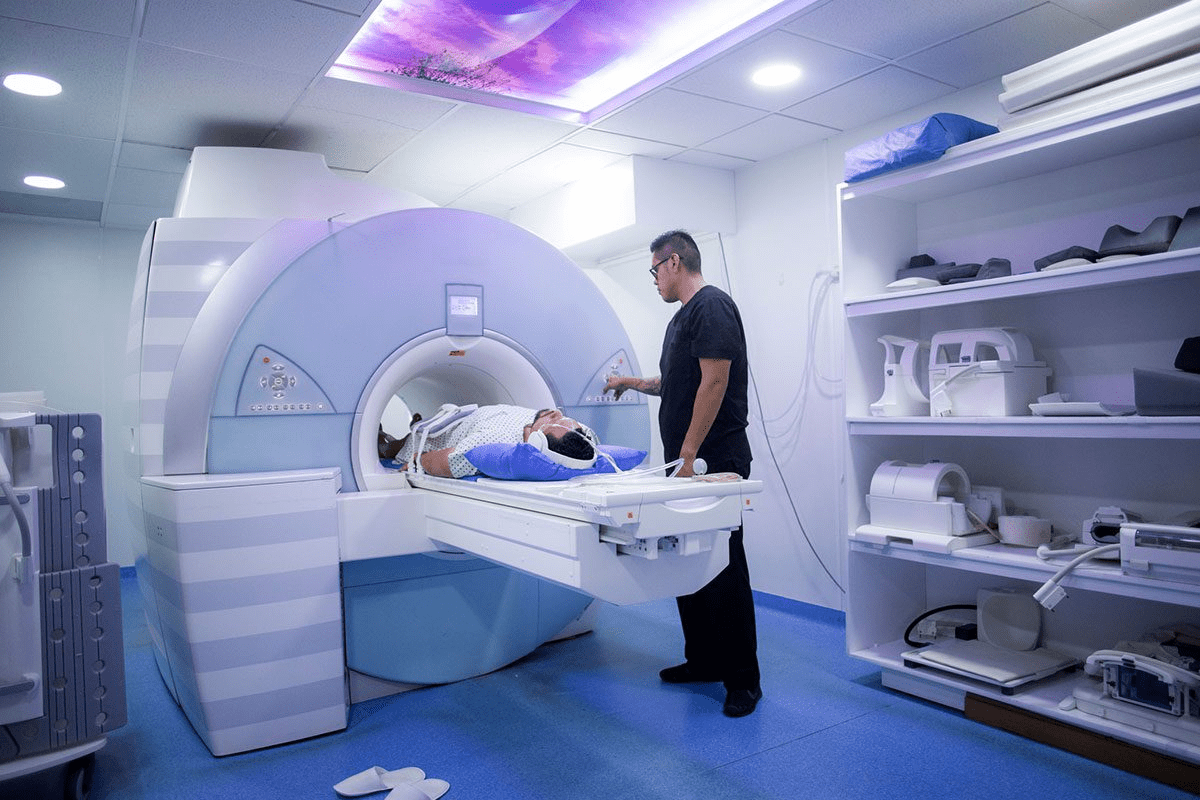
The decision to do a craniotomy depends on the patient’s condition. This includes looking at CT scans and MRI images. Key indications for craniotomy include:
- Acute subdural or epidural hematoma causing significant mass effect
- Large contusions or lacerations with significant edema
- Depressed skull fractures with underlying brain injury
- Penetrating head injuries with significant damage
Before surgery, a team of experts plans the operation. This team includes neurosurgeons, radiologists, and anesthesiologists. They look at the imaging, check the patient’s brain function, and decide how to approach the surgery.
Advanced Techniques and Technology in Modern Craniotomies
Modern craniotomies use new techniques and technology. These advancements help improve results and shorten recovery times. Some of these include:
| Technique/Technology | Description | Benefit |
| Neuronavigation | Uses imaging data to guide surgical approach | Enhanced precision, reduced risk of complications |
| Intraoperative MRI | Allows for real-time imaging during surgery | Immediate assessment of surgical progress, ability to make adjustments |
| Microsurgical Techniques | Utilizes operating microscopes for detailed work | Improved visualization, more precise repairs |
These new tools have made craniotomy safer and more effective. They help patients get better care for acute head trauma.
Skull Fracture Surgery and Reconstruction
Fixing cranial fractures needs a careful plan. The severity and type of fracture decide the surgery needed.
Classification and Assessment of Cranial Fractures
Doctors sort cranial fractures by location, severity, and if they’re open or closed. Knowing this helps pick the right surgery.
- Linear Fractures: These are common and often need little treatment unless they cause other problems.
- Depressed Fractures: Bone pieces press into the brain, so surgery is needed to lift them.
- Basilar Fractures: At the skull’s base, these are tricky because of nearby important areas.
Doctors use CT scans to see how bad the fracture is and if there are other injuries.
Surgical Repair Techniques for Complex Skull Injuries
Surgery fixes skull fractures to keep the brain safe and prevent infections or more damage.
| Fracture Type | Surgical Indication | Repair Technique |
| Depressed Fracture | Significant displacement or brain compression | Elevation and fixation of bone fragments |
| Comminuted Fracture | Multiple bone fragments | Reconstruction using cranioplasty techniques |
| Open Fracture | Risk of infection or CSF leak | Debridement, closure, and possibly cranioplasty |
Cranioplasty is used to fix big holes or shape the skull back. It helps with both looks and function.
The right surgery depends on the fracture, the patient, and the doctor’s skills. New neurosurgery methods and tools help patients get better.
Intracranial Pressure Management After Brain Trauma
Managing intracranial pressure (ICP) is key after a brain injury. This pressure can rise due to swelling, bleeding, or fluid buildup. If not controlled, it can cause more brain damage or even death.
Monitoring Systems and Medical Interventions
Keeping an eye on ICP is vital for brain trauma patients. Doctors use different tools like catheters and monitors to check the pressure. These tools help them see the pressure in the skull all the time.
To lower ICP, doctors use medicines like mannitol, sedatives, and hyperventilation. These methods help by reducing the brain’s volume or making it more flexible.
Surgical Decompression Techniques for Elevated ICP
When medicines don’t work, surgery might be needed. A procedure called decompressive craniectomy removes part of the skull. This lets the brain expand and lowers ICP.
This surgery is for severe brain injuries that don’t respond to medicine. Doctors decide if it’s right for each patient based on their health and chances of recovery.
Key considerations in managing ICP include spotting high pressure early and choosing the right monitoring tools. A brain injury specialist is also important, working with a team to care for patients.
The aim of intracranial pressure management is to stop further brain damage and help patients recover. By using advanced monitoring and treatments, doctors can greatly improve care for these patients.
Trauma neurosurgeons must respond to severe trauma with speed and decisiveness.
Spinal trauma can cause serious harm. Neurosurgeons play a key role in fixing and stabilizing the spine. Injuries can happen from car accidents, falls, or sports. If not treated right away, they can lead to serious problems or even death.
Assessment and Classification of Traumatic Spinal Injuries
First, doctors check the spine by looking at how well nerves work.
Imaging tests like MRI and CT scans are also key. They help see if the spine is broken or if there are any blockages.
Surgical Approaches to Protect and Restore Spinal Cord Function
Surgery for spinal trauma aims to free the spinal cord and make the spine stable. It also tries to bring back nerve function. The surgery type depends on where and how bad the injury is.
- Anterior approaches are often used for cervical spine injuries, allowing for direct decompression of the spinal cord.
- Posterior approaches are commonly utilized for thoracic and lumbar injuries, providing stabilization through instrumentation and fusion techniques.
In some cases, a combined anterior-posterior approach may be necessary to achieve optimal decompression and stabilization.
The main goal of spinal trauma repair is to save lives and improve quality of life. It aims to help patients recover as much as possible and reduce long-term disabilities. New neurosurgical methods and tools are helping improve care for these patients.
Surgical Management of Traumatic Intracranial Hemorrhage
Intracranial hemorrhage from trauma needs quick and effective surgery to avoid brain damage. This serious condition can lead to severe outcomes if not treated fast.
Neurosurgeons use various procedures to relieve brain pressure and prevent injury. They make critical decisions to save lives.
Subdural and epidural hematomas need immediate surgery. Removing these hematomas is a complex task. It aims to reduce brain pressure and restore function.
To remove the hematoma, a craniotomy is performed. This involves temporarily removing a part of the skull. It requires precision to avoid further bleeding.
| Type of Hematoma | Surgical Approach | Outcome |
| Subdural Hematoma | Craniotomy with evacuation | Relief of pressure, possible recovery |
| Epidural Hematoma | Craniotomy with evacuation | Relief of pressure, possible recovery |
Intracerebral Hemorrhage Treatment Strategies
Intracerebral hemorrhage occurs within the brain tissue. Treatment combines medical and surgical methods. These aim to reduce the hemorrhage and ease brain pressure.
- Medical management to control blood pressure and intracranial pressure
- Surgical intervention to evacuate the hemorrhage or decompress the brain
- Rehabilitation to address any resulting neurological deficits
The treatment choice depends on the hemorrhage’s size, location, and the patient’s condition. Neurosurgeons collaborate with other healthcare professionals to find the best treatment.
Emergency brain surgery is often needed for traumatic intracranial hemorrhage. This shows the importance of skilled neurosurgeons who can act quickly and effectively.
Trauma Team Collaboration in Neurosurgical Emergencies
In neurosurgical emergencies, teamwork is key to saving lives. These situations need quick and precise actions. So, it’s vital for different medical teams to work together well.
Coordinating with Emergency Medicine and Trauma Surgery
Neurosurgeons, emergency doctors, and trauma surgeons must work as one. They quickly check the patient, decide what to do first, and make big decisions together.
- Rapid Assessment: The team quickly checks the patient’s brain health and decides if surgery is needed right away.
- Communication: Good communication means everyone shares important info fast.
- Decision-Making: Working together helps the team create a plan that fits the patient’s needs.
Multidisciplinary Approach to Polytrauma with Neurological Injuries
Polytrauma patients with brain injuries are very challenging. The team works with many experts, like brain doctors, bone doctors, and rehab specialists. They tackle all parts of the patient’s problem together.
| Specialty | Role in Polytrauma Care |
| Neurosurgery | Manages traumatic brain and spinal injuries, performing surgical interventions as necessary. |
| Orthopedic Surgery | Addresses fractures and other musculoskeletal injuries, often working in conjunction with neurosurgeons. |
| Rehabilitation Medicine | Provides early intervention to optimize functional recovery and minimize long-term disability. |
Success in neurosurgical emergencies comes from teamwork. When different specialties work well together, patients get better care. This teamwork can save lives and improve outcomes.
Post-Surgical Neuro-Critical Care
Post-surgical neuro-critical care is key for brain injury patients. It helps improve outcomes and prevent more damage.
Specialized Neurological ICU Protocols
Brain injury patients need special care in the ICU. This care focuses on monitoring vital signs and brain pressure.
Advanced systems track patient data in real-time. Multimodal monitoring gives a full picture of the brain’s health. This includes checking pressure, oxygen levels, and brain waves.
| Monitoring Technique | Purpose | Benefits |
| Intracranial Pressure Monitoring | Measures pressure within the cranial vault | Helps in managing elevated ICP, reducing risk of brain herniation |
| Cerebral Oxygenation Monitoring | Assesses oxygen delivery to brain tissue | Guides therapy to optimize cerebral oxygenation, improving outcomes |
| Continuous Electroencephalography | Monitors electrical activity in the brain | Aids in detecting seizures, guiding anticonvulsant therapy |
Preventing and Managing Secondary Brain Injury
Stopping secondary brain injury is vital. It can happen due to low blood pressure, lack of oxygen, or high brain pressure.
To prevent it, keep blood pressure right, ensure enough oxygen, and control brain pressure. Vasopressor therapy helps with blood pressure. Hyperosmolar therapy lowers brain pressure.
Good care for brain injury patients needs a team effort. Neurosurgeons, neurointensivists, nurses, and others work together. This team approach ensures the best care for these patients.
Innovations in Traumatic Brain Injury Treatment
The field of traumatic brain injury treatment is changing fast. New technologies and less invasive methods are leading the way. This change is key to better patient care and simpler treatment for TBI.
Minimally Invasive Neurosurgical Techniques
Minimally invasive neurosurgery is changing how we treat brain injuries. It uses smaller cuts, which means less damage and quicker healing. Some important methods include:
- Endoscopic Surgery: This method lets surgeons work through small openings. They use a camera and special tools to fix problems without big cuts.
- Stereotactic Surgery: It uses a 3D system to find and treat brain spots accurately. This method helps avoid harming nearby tissue.
- Neuroendoscopy: It lets doctors see and treat problems inside the brain without open surgery. This is great for treating bleeding and other issues.
These methods cut down on risks and make surgeries more precise. This leads to better results for patients.
Emerging Technologies and Future Directions
New technologies are also key in TBI treatment. Some exciting areas include:
- Advanced Imaging Techniques: High-definition MRI and CT scans give clear views of brain injuries. This helps doctors diagnose and plan treatments better.
- Neurostimulation Therapies: Methods like TMS and tDCS are being studied. They might help improve brain function and aid in recovery.
- Biomaterials and Implants: New materials are being made for implants. These could help fix skull damage and other TBI issues more effectively.
As these technologies get better, they will likely make TBI treatment even more effective. They offer new ways to help patients recover and improve their lives.
Patient Recovery and Rehabilitation Pathways
The journey to recovery for patients with brain injuries is complex. It needs a detailed approach to rehabilitation. Effective recovery pathways are key for better patient outcomes and quality of life.
Transition from Acute Care to Specialized Rehabilitation
The move from acute care to specialized rehabilitation is vital. Healthcare teams work together to assess needs and create a personalized plan. Specialized rehabilitation programs tackle the unique challenges of brain injury patients, including cognitive, physical, and emotional issues.
Patients are checked to see if they’re ready for rehabilitation. They might need physical, occupational, speech, or cognitive therapy. The aim is to help them regain independence and improve their abilities.
Long-term Neurological Outcome Assessment and Follow-up
Long-term assessments and follow-ups are key in rehabilitation. They let healthcare providers track progress, spot complications early, and adjust treatments. Regular check-ups help understand the patient’s recovery and make informed care decisions.
Long-term outcomes vary among brain injury patients. They depend on injury severity, initial treatment, and overall health. Assessments cover cognitive function, motor skills, and emotional well-being. These guide long-term care plans, including therapy, medication, and lifestyle changes.
Healthcare providers focus on both immediate and long-term recovery goals. This approach offers complete care that boosts patient outcomes and quality of life.
Conclusion: The Life-Saving Impact of Trauma Neurosurgeons
Trauma neurosurgeons play a key role in emergency care, focusing on complex brain injuries. Their training and skills help them make a big difference in patient care.
Their work is truly life-saving. They quickly assess and treat traumatic brain injuries. This prevents more damage and boosts survival chances. Their efforts highlight the need for ongoing progress in trauma neurosurgery.
As medical tech and methods improve, trauma neurosurgery will also advance. New tools like minimally invasive surgery and better imaging will help these doctors save more lives.
FAQ
What is the role of a trauma neurosurgeon in treating brain injuries?
A trauma neurosurgeon specializes in surgeries for brain and spinal cord injuries. They are key in emergency situations. They perform craniotomies and manage pressure inside the skull.
What kind of training is required to become a trauma neurosurgeon?
To become a trauma neurosurgeon, you need to finish medical school. Then, you do a neurosurgery residency. After that, you get specialized training in trauma neurosurgery. This requires a lot of education and hands-on experience.
What are the common types of traumatic brain injuries that require surgical intervention?
Common injuries needing surgery include acute subdural hematomas and epidural hematomas. Also, depressed skull fractures and intracerebral hemorrhages require surgery. Each injury needs a specific surgical approach.
How is intracranial pressure managed after a brain trauma?
Managing intracranial pressure involves tracking ICP levels. Medical treatments are used to lower pressure. Sometimes, surgery like decompressive craniectomy is needed to relieve pressure and prevent damage.
What is the importance of trauma team collaboration in neurosurgical emergencies?
Collaboration is key in neurosurgical emergencies. It involves working with emergency medicine and trauma surgery. This ensures a team approach, which is vital for patients with complex injuries.
What advancements are being made in traumatic brain injury treatment?
New treatments include minimally invasive surgeries and technologies like neuroendoscopy and robotic surgery. Future advancements include stem cell therapy and advanced monitoring. These aim to improve recovery and reduce recovery times.
What does the recovery and rehabilitation process entail for patients with brain injuries?
Recovery for brain injury patients starts with moving from acute care to rehabilitation. It focuses on regaining lost functions and managing symptoms. Long-term follow-up is also important to help patients recover fully.
How do trauma neurosurgeons contribute to saving lives in emergency situations?
Trauma neurosurgeons save lives by providing immediate surgical care for brain and spinal injuries. Their expertise is critical in emergency situations, greatly impacting patient outcomes and survival.
What is a craniotomy, and when is it performed?
A craniotomy involves temporarily removing part of the skull to access the brain. It’s done for acute head trauma, intracranial hemorrhage, or other conditions needing direct brain intervention. It helps relieve pressure, repair damaged areas, or remove hematomas.
How are spinal trauma injuries assessed and treated?
Spinal trauma injuries are assessed through imaging and clinical evaluation. Treatment involves surgery to stabilize the spine and protect the spinal cord. It may include decompression, stabilization, and fusion techniques.
References
The Lancet. Trauma neurosurgery acute care decision making. Retrieved from https://www.thelancet.com/journals/laneur/article/PIIS1474-4422(17)30371-X/fulltext