Last Updated on December 2, 2025 by Bilal Hasdemir

Nearly 70% of patients who have brain stem surgery do well, studies show. This is a big deal, given how complex and delicate these surgeries are. The survival rate depends on several things, like the condition being treated and the patient’s health.
We’ll dive into these factors, giving you a full picture of what to expect from brain stem operations. The condition being treated, the patient’s age, and the surgery method all play big roles in the survival statistics.
Key Takeaways
- The overall survival rate for brain stem surgery is approximately 70%.
- The underlying condition being treated significantly influences survival rates.
- Patient age and overall health are critical factors.
- The surgical approach used can impact the outcome.
- Recent advancements in medical technology have improved survival statistics.
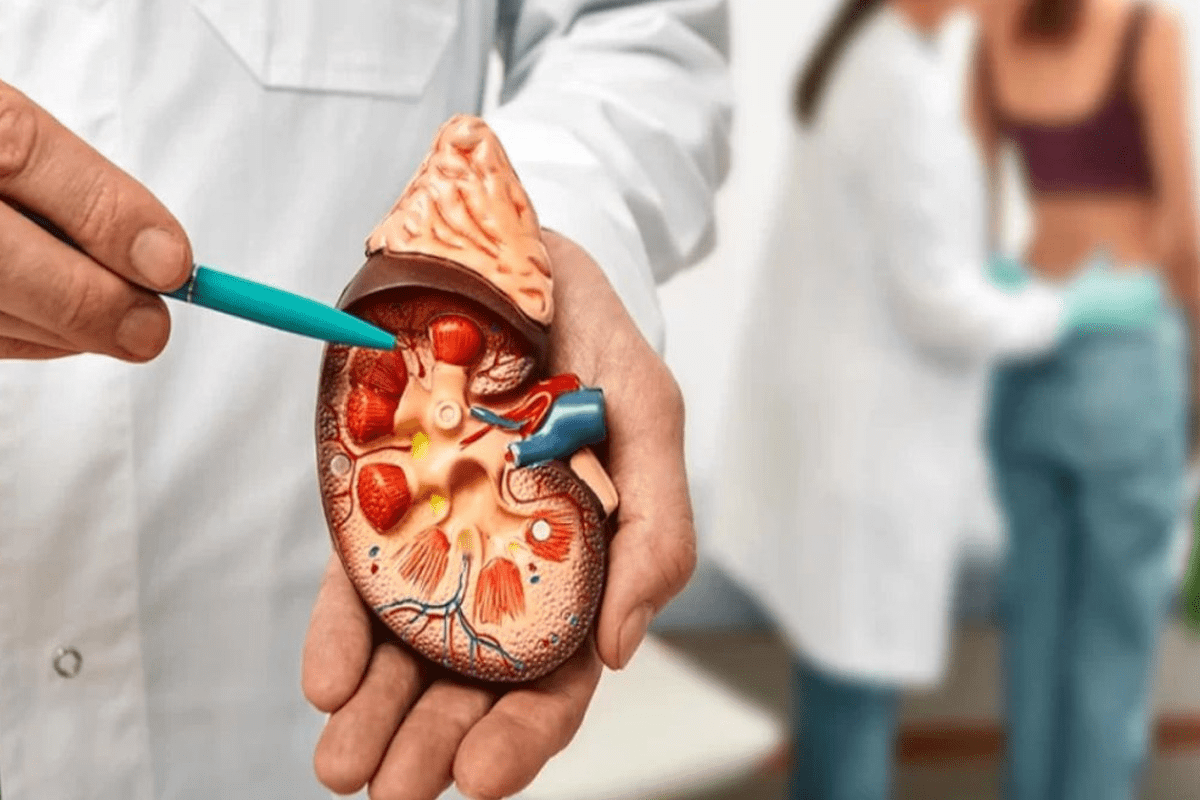
Understanding the Brain Stem and Its Critical Functions
The brain stem is a key part of our nervous system. It helps control many automatic body functions. It connects the brain to the spinal cord, sending signals for different body operations.
Anatomy of the Brain Stem
The brain stem has three main parts: the midbrain, pons, and medulla oblongata. Each part has its own job, making the brain stem complex. The midbrain handles hearing and sight. The pons control sleep and wakefulness. The medulla oblongata is key for breathing and heart rate.
Vital Functions Controlled by the Brain Stem
The brain stem manages many body actions we can’t control, like breathing, heart rate, and blood pressure. These are vital for living. It also helps control how alert we are and our sleep patterns.
Why Brain Stem Surgery is Considered High-Risk
Surgery on the brain stem is risky because of its delicate nature and important functions. Any surgery here needs careful planning and execution to avoid complications. The risks of brain stem surgery include damage, infection, and bad reactions to anesthesia.
Knowing about the brain stem’s anatomy and functions is key to understanding surgery challenges here. Its complex nature and vital role in body functions make it a tough area for surgery.
Brain Stem Surgery Survival Rate: Current Statistics
Medical technology and surgery have improved a lot. This has led to better survival rates for brain stem surgery. We’ll look at the latest stats on survival rates for these complex surgeries.
Overall Survival Percentages
Survival rates for brain stem surgery depend on the condition being treated. Studies show rates from 70% to 90% for some cases. For example, a study on brain stem gliomas found a 75% survival rate at one year after surgery.
Survival rates are affected by the patient’s age, the condition, and the surgery. Better surgery techniques and care have helped improve these rates over time.
Mortality Rates During and After Surgery
Mortality rates during and after surgery are important. They show the risks of these procedures. Studies say the 30-day mortality rate is between 5% and 15%, based on the case’s complexity and the patient’s health before surgery.
Most deaths are due to surgery complications or the condition itself. Knowing these risks helps patients and doctors make treatment choices.
How Survival Statistics Are Collected and Analyzed
Survival stats for brain stem surgery come from clinical studies and registries. These track patient outcomes over time. Sophisticated methods analyze the data, considering many factors that affect survival rates.
The data collection process is detailed. It involves following up with patients to see if they’re alive and any complications they face. This helps find trends and improve patient care.
Condition | 1-Year Survival Rate | 5-Year Survival Rate |
Brain Stem Glioma | 75% | 40% |
Cavernoma | 90% | 85% |
AVM | 80% | 70% |
Types of Brain Stem Conditions Requiring Surgery
The brain stem is a key part of the brain. It can face many conditions that might need surgery. These issues can be very serious and are a big challenge for doctors. Knowing what condition a patient has is key to finding the right treatment and understanding the outcome.
Brain Stem Tumors
Brain stem tumors are abnormal growths in the brain stem. They can be either benign or malignant. Their size and location greatly affect a patient’s life quality. Surgery is often needed to ease symptoms and improve survival rates.
Types of Brain Stem Tumors:
- Gliomas: These are the most common type of brain stem tumor, arising from the brain’s glial tissue.
- Ependymomas: These tumors originate from the ependymal cells lining the ventricles and central canal of the spinal cord.
Vascular Malformations
Vascular malformations in the brain stem are abnormal blood vessel formations. They can cause serious neurological problems. These malformations can bleed, leading to hemorrhages. Surgery may be needed to stop further issues.
“Vascular malformations are a significant cause of brain stem hemorrhages, and their management requires a multidisciplinary approach.”
Medical Expert, Neurosurgeon
Type of Malformation | Description | Treatment Approach |
Arteriovenous Malformation (AVM) | Abnormal connection between arteries and veins | Surgical resection or embolization |
Cavernous Malformation | Abnormally large blood vessel cavities | Surgical removal or radiosurgery |
Traumatic Injuries and Hemorrhages
Traumatic brain injuries can cause hemorrhages or hematomas in the brain stem. These are serious and need immediate surgery. The goal is to reduce pressure on the brain stem and prevent more damage.
Prompt surgical intervention is critical in cases of traumatic brain injuries to minimize long-term neurological damage.
Infections and Abscesses
Infections in the brain stem are rare but serious. They can lead to abscesses, which are collections of pus. These need quick treatment, often through surgical drainage of the abscess. This is to prevent severe damage or death.
Managing brain stem infections and abscesses involves antibiotics and surgery. The choice to operate depends on the abscess’s size, location, and the patient’s health.
Survival Rates by Specific Brain Stem Pathologies
The survival rate for brain stem surgery depends on the specific condition being treated. Different brain stem issues have different outcomes. It’s important to know the exact diagnosis and its survival stats.
Brain Stem Glioma Survival Statistics
Brain stem gliomas are tough to treat because of their location and the surgery challenges. Survival rates for brain stem glioma have gotten better with new surgical methods and treatments. For kids, the 5-year survival rate is 20% to 30%. For adults, the outlook is less hopeful.
Cavernoma Surgery Outcomes
Cavernomas, or vascular lesions, can happen in the brain stem. Surgery for cavernomas is considered when there’s a high risk of bleeding or symptoms. The surgery success rate is high, with low death rates in specialized hospitals.
AVM Surgery Survival Rates
Arteriovenous malformations (AVMs) in the brain stem are complex and risky. AVM surgery survival rates have improved with new techniques. The survival rate is generally high, but it depends on the AVM’s size, location, and the patient’s health.
Brain Stem Metastasis Prognosis
Brain stem metastases are rare but have a poor outlook. The survival rate for brain stem metastasis is lower than other conditions. Treatment aims to control symptoms and improve quality of life, as the cancer is often advanced.
Pathology | Typical Survival Rate | Treatment Options |
Brain Stem Glioma | 20-30% (5-year) | Surgery, Radiation, Chemotherapy |
Cavernoma | High (post-surgery) | Surgery |
AVM | High (post-treatment) | Surgery, Radiosurgery, Endovascular |
Brain Stem Metastasis | Poor (varies by primary cancer) | Palliative Care, Radiation |
Surgical Approaches to the Brain Stem
Neurosurgery has made big strides, leading to many surgical techniques for the brain stem. The right surgical approach is key to a good outcome. We’ll look at open surgery, minimally invasive methods, and stereotactic procedures.
Open Surgical Techniques
Open surgery means making a cut in the skull to reach the brain stem. It’s a traditional method used for complex cases or big lesions. Open surgery gives a wide path to the brain, which is good in some cases.
Minimally Invasive Approaches
Minimally invasive surgery uses smaller cuts and less damage than open surgery. Endoscopic or keyhole surgeries are examples. These methods cut down recovery time and lower complication risks.
Stereotactic Procedures
Stereotactic surgery uses a 3D system to find small targets in the brain. It’s great for small lesions or tumors hard to reach. Stereotactic procedures are very precise, protecting the brain around the target.
Impact of Surgical Approach on Survival
The surgical method chosen can greatly affect survival and outcomes for brain stem surgery patients. The type of problem, the patient’s health, and the surgeon’s skill play a role. We’ll keep seeing better surgical techniques that help patients more.
Factors Affecting Brain Stem Surgery Survival Rate
Brain stem surgery survival rates depend on many factors. Knowing these factors helps predict outcomes and guide treatment choices.
Patient-Related Factors
Patient-related factors are key in brain stem surgery survival. These include:
- Age: A patient’s age can greatly affect recovery and survival. Older patients might face more risks.
- Overall Health: Existing health conditions can impact recovery from surgery.
- Neurological Status: The patient’s brain function before surgery is very important for their outcome.
Disease-Related Factors
The type and characteristics of the condition needing surgery also matter a lot. These include:
- Type of Pathology: Different brain stem issues (like tumors or malformations) have different survival chances.
- Tumor Characteristics: For tumors, the grade, size, and location are key.
- Vascular Malformation Complexity: The size and complexity of malformations affect surgery difficulty and success.
Disease-Related Factor | Impact on Survival |
Tumor Grade | Higher grades generally have poorer prognosis |
Vascular Malformation Size | Larger malformations are associated with higher surgical risk |
Pathology Type | Different pathologies have varying survival rates |
Treatment-Related Factors
Treatment choices also play a big role in brain stem surgery outcomes. These include:
- Surgical Technique: The surgical method (like open or minimally invasive) can affect results.
- Surgeon Experience: The skill and experience of the surgical team are very important for success.
- Adjuvant Therapies: Treatments like radiation or chemotherapy can also impact survival.
Understanding these factors helps doctors predict outcomes and make better treatment plans for brain stem conditions.
Complications and Risks of Brain Stem Surgery
Brain stem surgery can save lives but comes with big risks. These risks are important for both patients and doctors to think about. The brain stem is complex and vital, making surgery tricky. Complications can affect how well a patient does after surgery.
Immediate Postoperative Risks
The time right after surgery is very important. There are several risks that need to be watched closely. These include:
- Respiratory Complications: Trouble breathing or failing to breathe because of the brain stem’s role.
- Cardiovascular Instability: Changes in blood pressure or heart rate that can be dangerous if not handled quickly.
- Neurological Deficits: New or worse problems with movement, feeling, or speaking and swallowing.
We keep a close eye on patients in the ICU to spot and handle these risks fast.
Common Complications
There are also common problems that can happen after brain stem surgery. These include:
Complication | Description | Management Strategies |
Infection | Surgical site infections or meningitis | Prophylactic antibiotics, close monitoring for signs of infection |
Cerebrospinal Fluid (CSF) Leak | Leakage of CSF through the surgical site or ear/nose | Bed rest, lumbar drain placement, or surgical repair |
Vascular Complications | Stroke or vasospasm due to vascular injury | Nimodipine administration, close monitoring of vascular status |
A neurosurgical expert says, “The key to managing complications is early detection and intervention. This requires a team effort from neurosurgeons, intensivists, and rehabilitation specialists.”
“The management of brain stem surgery complications requires a complete and team-based approach. It combines surgical skills with advanced neurocritical care.”
Long-term Mortality Considerations
Survival chances after brain stem surgery depend on several things. These include the reason for surgery, the patient’s age, and overall health. We think about these when talking about the future with patients and their families.
Knowing about long-term survival helps in making choices about treatment and care after surgery.
Recovery and Rehabilitation After Brain Stem Surgery
The journey to recovery after brain stem surgery is complex. It involves rehabilitation and support. Knowing the recovery process is key for patients and their families.
Typical Recovery Timeline
The recovery time after brain stem surgery varies. It depends on the patient’s condition, the surgery’s complexity, and any complications. The initial recovery in the hospital can last from a few days to weeks.
During this time, patients are watched for any neurological issues or complications. The medical team manages pain, prevents infections, and deals with immediate postoperative problems.
“The initial recovery phase is critical, and our medical team is dedicated to providing the highest level of care to ensure the best possible outcomes.”
Medical Expert, Neurosurgeon
Rehabilitation Requirements
Rehabilitation is key in the recovery after brain stem surgery. The type and extent of rehabilitation needed depend on the patient’s condition after surgery.
- Physical therapy to regain strength and mobility
- Occupational therapy to improve daily functioning and independence
- Speech therapy if there are issues with speech or swallowing
A detailed rehabilitation plan is made for each patient. It aims to help them regain function and improve their quality of life.
Neurological Function Recovery Patterns
Recovering neurological functions after brain stem surgery takes time. Recovery varies among patients. It depends on the surgery area and the condition being treated.
Neurological Function | Typical Recovery Pattern |
Motor Function | Gradual improvement over weeks to months |
Speech and Swallowing | Variable recovery, often requiring intensive therapy |
Cognitive Function | Generally improves over time, though some deficits may persist |
Knowing these recovery patterns helps set realistic expectations. It helps patients and their families plan for the future.
As neurosurgical techniques and care improve, patient outcomes are getting better. Our focus is on giving full support during recovery and rehabilitation.
Quality of Life Following Brain Stem Surgery
After brain stem surgery, patients and their families face many challenges. These include physical, cognitive, and emotional impacts. Understanding these challenges is key to providing the best care.
Physical Limitations and Management
Brain stem surgery can lead to physical limitations. Patients might struggle with moving, balancing, and coordinating. To help, we use physical therapy, occupational therapy, and assistive devices.
For example, physical therapy can improve a patient’s mobility and strength. This process takes time and requires dedication. We create personalized plans to meet each patient’s needs and goals.
Cognitive and Emotional Impacts
After surgery, patients may have memory problems, trouble focusing, or mood swings. These changes can be tough for everyone involved. We stress the importance of psychological support and counseling.
We also offer cognitive rehabilitation programs. These are customized to help patients improve their memory, attention, and problem-solving skills.
Return to Daily Activities and Work
Getting back to daily life and work is a big step in recovery. The time it takes varies based on the surgery and the patient’s health. We advise starting with less strenuous activities to avoid exhaustion.
Some patients may need vocational rehabilitation to return to work. This can involve adjusting job tasks or training on new skills to accommodate any limitations.
Patient-Reported Outcome Measures
Patient-reported outcome measures (PROMs) help us understand the quality of life after surgery. They give insights into physical, cognitive, and emotional well-being. We use these measures to tailor care and support to each patient’s needs.
By understanding patients’ challenges, we can improve our care. This patient-centered approach is vital for better outcomes and quality of life.
Aspect of Quality of Life | Common Challenges | Management Strategies |
Physical Limitations | Mobility, coordination, balance issues | Physical therapy, occupational therapy, assistive devices |
Cognitive Impacts | Memory issues, difficulty concentrating | Cognitive rehabilitation programs |
Emotional Impacts | Mood swings, emotional changes | Psychological support, counseling |
Return to Daily Activities | Varying recovery times, overexertion | Gradual resumption of activities, vocational rehabilitation |
Long-Term Survival Outcomes and Prognosis
Understanding long-term survival after brain stem surgery is key for patients. The prognosis depends on several factors. These include the condition being treated, the patient’s health, and the surgery techniques used.
Long-term survival rates are important for patients and their families. We will look at 5-year and 10-year survival rates. We will also discuss what predicts long-term survival and recurrence rates.
5-Year Survival Rates
Five-year survival rates are a key measure of long-term outcomes after brain stem surgery. These rates vary a lot based on the underlying pathology. For example, some brain stem tumors have better 5-year survival rates than others.
- Patients with low-grade gliomas tend to have better 5-year survival rates.
- Those with high-grade gliomas or metastatic lesions often face poorer outcomes.
- The surgical approach and adjuvant therapies play a significant role in determining long-term survival.
10-Year Survival Rates
Ten-year survival rates give a longer view of outcomes after brain stem surgery. These rates are very important for younger patients or those with a history of successful initial treatment. Factors influencing 10-year survival include the effectiveness of initial surgery, the presence of any recurrence, and the patient’s overall health over time.
- Patients who undergo successful surgery and adjuvant therapy may achieve favorable 10-year survival rates.
- Regular follow-up and monitoring are critical for detecting any recurrence early.
- Advances in surgical techniques and adjuvant therapies continue to improve long-term outcomes.
Factors Predicting Long-Term Survival
Several factors predict long-term survival after brain stem surgery. These include the patient’s age, the nature of the pathology, the extent of surgical resection, and the use of adjuvant therapies. Understanding these factors helps clinicians provide more accurate prognoses and tailor treatment plans to individual patient needs.
Recurrence Rates and Management
Recurrence rates after brain stem surgery vary based on the initial condition treated. Effective management of recurrence is critical for improving long-term survival outcomes. Strategies for managing recurrence may include repeat surgery, radiation therapy, or other adjuvant treatments.
- Regular monitoring is essential for early detection of recurrence.
- Treatment plans for recurrence are highly individualized based on the patient’s condition and previous treatments.
- Advances in imaging and diagnostic techniques aid in the early detection and management of recurrence.
Adjuvant Therapies and Their Impact on Survival
Adjuvant therapies have changed how we treat brain stem surgery patients. They offer hope for better survival rates. These include radiation, chemotherapy, and new targeted and immunotherapies. They are key to improving brain stem surgery outcomes.
Radiation Therapy Outcomes
Radiation therapy is a key part of treating brain stem conditions. It’s used after surgery to kill any leftover tumor cells. It also helps with conditions that can’t be removed by surgery.
Studies show it can greatly improve survival rates for certain brain stem tumors.
- Improved Local Control: Radiation therapy helps control the tumor better, lowering the chance of it coming back.
- Enhanced Survival: It targets any remaining tumor cells, helping patients live longer.
Chemotherapy Results
Chemotherapy is used for brain stem conditions, mainly for tumors that respond well to it. How well it works depends on the tumor type and grade.
Chemotherapy Outcomes include:
- It can improve survival for patients with tumors that are sensitive to it.
- It can also shrink tumors, making other treatments more effective.
Emerging Targeted and Immunotherapies
Targeted and immunotherapies are new in treating brain stem conditions. They aim to target specific parts of tumor growth and progression.
Benefits of Targeted and Immunotherapies include:
- They might be more effective with fewer side effects than traditional chemotherapy.
- They offer personalized treatments based on the tumor’s molecular makeup.
Multimodal Treatment Approaches
Using surgery, radiation, chemotherapy, and targeted therapies together is becoming more common. These approaches are customized for each patient and their condition.
Advantages of Multimodal Treatment include:
- They manage the condition fully, tackling both local and systemic disease.
- They can lead to better survival rates and quality of life through a well-coordinated plan.
Pediatric vs. Adult Brain Stem Surgery Outcomes
It’s important to know how brain stem surgery results differ between kids and adults. The age of the patient greatly affects the surgery’s success. Many factors influence the outcome.
Survival Differences by Age Group
Survival rates after brain stem surgery differ between kids and adults. Kids often face different health issues and recover better than adults. They tend to do well in surgeries like tumor removals.
Adults, on the other hand, may have more health problems. This can make surgery and recovery harder. Adults’ survival rates depend on their health, the surgery type, and the brain stem issue.
Pediatric-Specific Considerations
Pediatric brain stem surgery has its own special needs. The developing brain and long-term effects on a child’s brain are key. Kids need care that fits their age and growth stage.
The surgical team must think about the child’s health, the surgery type, and recovery chances. Also, kids and their families need emotional and psychological support.
Elderly Patient Outcomes and Considerations
Elderly patients face unique challenges in brain stem surgery. Older adults may have weaker bodies, making surgery risks higher. Health issues like heart disease or diabetes can also affect outcomes.
Despite these challenges, better surgery techniques and care have helped elderly patients. Choosing the right patient, thorough checks before surgery, and custom surgical plans are key for better results.
Recent Advances Improving Brain Stem Surgery Survival
The field of neurosurgery has seen big steps forward in brain stem surgery. New technologies and better surgical methods are helping patients more. These advancements are making brain stem surgery safer and more effective.
Technological Innovations
New technologies are key in brain stem surgery. Intraoperative MRI and CT scans let surgeons see the brain stem live during surgery. This helps them remove tumors more accurately and safely.
Advanced navigation systems are also important. They give surgeons detailed, 3D images of the brain stem. This helps them plan and do complex surgeries better.
Improved Surgical Techniques
Surgical methods have also gotten better. Minimally invasive surgeries are now used more. They have smaller cuts and less damage, leading to quicker recovery and fewer problems.
Also, microsurgical techniques allow for precise work on small brain stem areas. High-powered microscopes and special tools help surgeons do detailed surgery.
Personalized Medicine Approaches
Personalized medicine is being used more in brain stem surgery. It tailors treatments to each patient’s needs. This includes using genetic and molecular tests to understand the patient’s condition.
It also means customizing surgical plans based on detailed tests. This ensures the surgery fits the patient’s unique situation, leading to better results.
As we keep improving, brain stem surgery outcomes will likely get even better. The mix of new technologies, better surgery methods, monitoring, and personalized care is setting a new standard in neurosurgery.
Conclusion: The Future of Brain Stem Surgery Outcomes
Looking back, brain stem surgery has seen big improvements thanks to new neurosurgery techniques. These advances have made a real difference in how well patients do after surgery. We’re seeing better survival rates and a higher quality of life for those who have had brain stem surgery.
The outlook for brain stem surgery is bright. New technologies and methods are on the horizon. These will likely make surgery even safer and more effective. We’re excited about the role that new surgical methods, treatments, and personalized care will play in the future.
We’re committed to making brain stem surgery better. By learning from our successes and tackling the tough challenges, we aim to improve outcomes. As we move forward, we promise to provide top-notch care to patients from around the world.
FAQ
What is the overall survival rate for brain stem surgery?
Survival rates vary widely depending on the condition, patient age, and surgery type. Studies show rates from 50% to 90% or more, depending on the disease and treatment.
How do brain stem tumors affect surgery survival rates?
Brain stem tumors, such as gliomas, can lower survival rates. Surgery for these tumors ranges from 20% to 60% or more, depending on tumor grade, patient age, and other treatments. Other tumor types have different survival outcomes.
What are the risks associated with brain stem surgery?
Risks include neurological complications, infection, bleeding, and long-term effects like cognitive changes or emotional challenges. Understanding these risks helps guide treatment decisions.
How does the surgical approach impact brain stem surgery outcomes?
The type of surgery—open, minimally invasive, or stereotactic—affects outcomes. Each approach has different risks and benefits, influencing survival and quality of life. The surgeon chooses the method based on the patient and condition.
What role do adjuvant therapies play in improving survival rates?
Radiation, chemotherapy, targeted therapies, and immunotherapies are often used after surgery. These treatments can reduce recurrence risk and improve survival, depending on the condition and patient.
How do pediatric and adult brain stem surgery outcomes differ?
Children and adults may have different outcomes due to age, overall health, and condition type. Children may recover faster, while older adults might face more complications.
What are the long-term survival outcomes for brain stem surgery patients?
Long-term survival varies by condition and treatment. Some studies report 5-year survival rates from 30% to 70%, depending on tumor type, patient health, and therapies used.
How have recent advances improved brain stem surgery survival rates?
Advances such as better imaging, surgical techniques, minimally invasive methods, and personalized medicine have improved survival rates and patient quality of life.
What can patients expect during recovery and rehabilitation after brain stem surgery?
Recovery varies per individual. Some patients improve quickly, while others need extended rehabilitation. Therapy may include physical, occupational, and speech therapy to regain function and independence. Understanding recovery expectations helps patients and families prepare.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/31279362/