Last Updated on December 2, 2025 by Bilal Hasdemir
Awake brain surgery, also known as awake craniotomy, is a complex procedure. Patients stay awake during parts of the operation. This lets surgeons watch the patient’s brain functions in real-time. It helps them avoid harming important areas.
Many patients worry about the pain during awake brain surgery. It’s normal to feel scared about surgery. People often wonder what they’ll feel during the procedure.
In this article, we’ll look at awake brain surgery. We’ll talk about how pain is managed and what patients go through. This should help answer your questions.
Key Takeaways
- Awake brain surgery is performed while the patient is conscious to monitor neurological functions.
- Advanced pain management techniques are used to minimize discomfort.
- The procedure requires careful planning and a skilled medical team.
- Patients are typically able to recover quickly from the surgery.
- Understanding the process can help alleviate concerns about pain and the overall experience.
What Is Awake Brain Surgery?

Awake brain surgery is a complex technique where the patient stays awake during part of the surgery. It’s also known as awake craniotomy. This method lets neurosurgeons do precise tasks while the patient is awake. This is important for the surgery’s success.
Definition and Purpose of Awake Craniotomy
Awake craniotomy is a surgery where the patient is awake and can talk to the surgeon. The main goal is to map brain functions in real-time. This helps surgeons avoid harming areas that control speech, movement, and other important functions.
The benefits of awake craniotomy are:
- It helps remove brain tumors safely while keeping important brain areas intact.
- It lowers the chance of brain damage during surgery.
- It lets surgeons test brain functions right during the surgery.
Historical Development of the Procedure
The idea of awake brain surgery started in the early 20th century. It has grown a lot over time. This growth came from new neurosurgical methods, better anesthesia, and brain mapping tech.
Important steps in awake craniotomy’s history include:
- The start of using local anesthesia, which lets patients stay awake during surgery.
- The creation of brain mapping tools, helping surgeons find and save key brain areas.
- Improvements in imaging tech, like functional MRI and intraoperative MRI, making awake craniotomy more precise.
Now, awake craniotomy is a key part of neurosurgery. It combines precision with safety for patients.
Why Doctors Perform Awake Brain Surgery
Awake craniotomy lets surgeons map brain functions with high precision. This makes surgery safer. It’s especially useful for complex brain conditions that need careful handling.
Functional Brain Mapping Necessity
Functional brain mapping is key in awake brain surgery. It helps identify and map important brain areas. This way, surgeons can avoid damaging them during surgery.
Surgeons use electrical stimulation to find out what each brain region does. This info is crucial for keeping brain functions intact. It helps ensure the patient’s quality of life after surgery.
Preserving Critical Brain Functions
The main goal of awake brain surgery is to keep vital brain functions intact. These include motor skills, language, and senses. By keeping the patient awake, surgeons can test these functions as they go.
This method lowers the chance of problems after surgery. It also lets surgeons tailor the surgery to the patient’s needs. This can lead to better results.
Advantages Over Traditional Surgery
Awake brain surgery has many benefits over traditional methods. It reduces the risk of brain damage and allows for more precise tumor removal. It also lowers the chance of complications after surgery.
Advantages | Description | Benefit |
Real-time Feedback | Surgeons get immediate feedback during the procedure. | Enhanced precision and safety. |
Preservation of Brain Functions | Critical brain areas are identified and preserved. | Better post-operative outcomes. |
Reduced Risk | Lower risk of damaging critical brain structures. | Improved patient recovery. |
Choosing awake brain surgery can greatly improve patient outcomes. It also reduces the risks of traditional brain surgery complications.
Medical Conditions Requiring Awake Craniotomy
Several critical medical conditions need awake craniotomy. This procedure maps the brain in real-time during surgery. It’s especially useful for treating conditions that affect important brain areas.
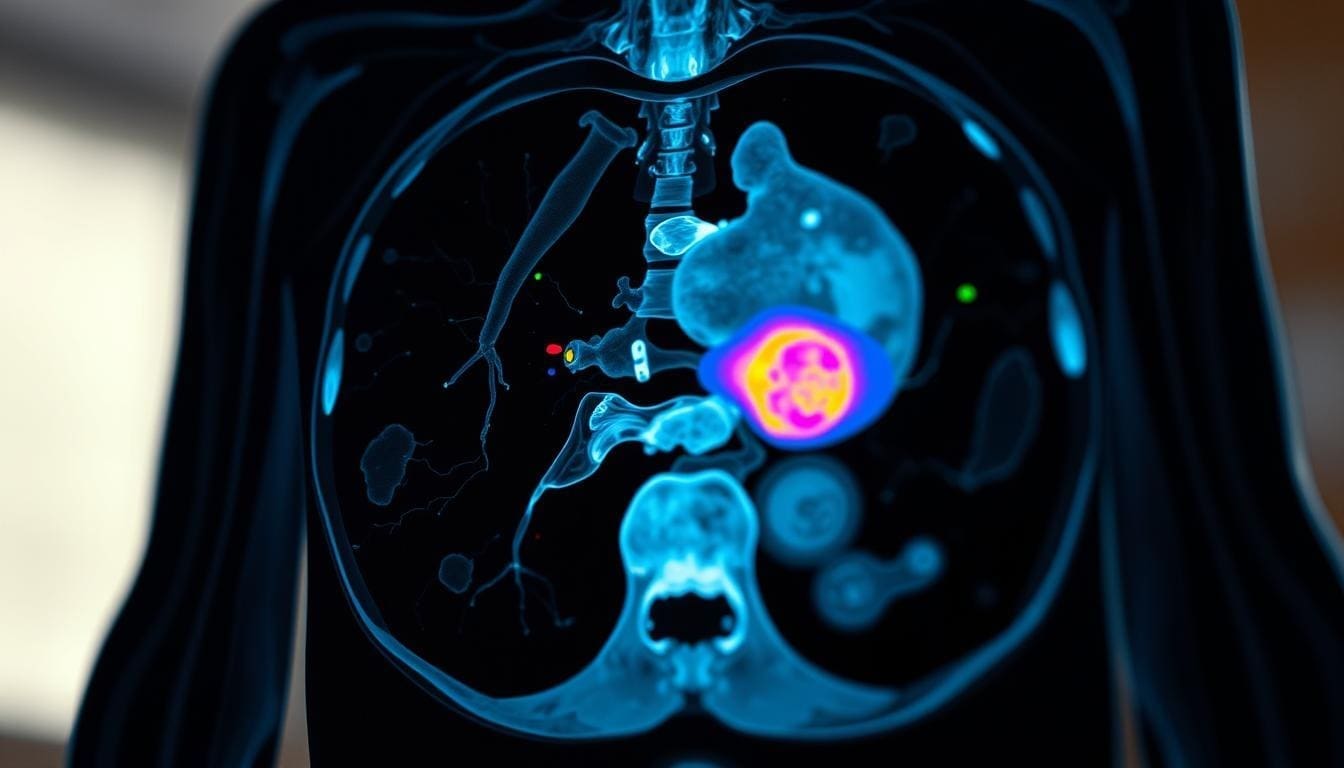
Brain Tumors in Eloquent Areas
Brain tumors in key brain areas are a big challenge for neurosurgeons. These areas handle vital functions like speech and movement. Awake craniotomy lets surgeons remove tumors without harming these areas.
By keeping the patient awake, surgeons can check how the brain responds. This ensures the tumor is removed safely.
Epilepsy and Seizure Disorders
Awake craniotomy can change lives for those with epilepsy or seizure disorders. It lets surgeons find and remove the seizure source while the patient is awake. This reduces the risk of harming important brain areas.
Real-time feedback from the patient helps surgeons locate the seizure source accurately. This improves surgery outcomes.
- Identification of seizure focus
- Real-time assessment of neurological functions
- Precise removal of the epileptogenic zone
Vascular Malformations
Vascular malformations, like AVMs, can also be treated with awake craniotomy. This method is great for AVMs in key brain areas. It lets surgeons monitor the patient’s brain status in real-time.
This precision reduces the chance of brain damage after surgery.
- Preoperative planning and imaging
- Intraoperative neurological monitoring
- Precise surgical resection of the malformation
In conclusion, awake craniotomy is a key tool for treating complex brain conditions. It makes neurosurgery safer and more effective by allowing real-time interaction with the patient.
The Truth About Pain During Brain Surgery
It’s important for patients to know about pain during brain surgery, especially with awake craniotomy. The thought of pain is natural due to the surgery’s delicate nature. Yet, it’s key to know the difference between the brain’s pain sensitivity and the discomfort during surgery.
Why the Brain Itself Cannot Feel Pain
The brain doesn’t have pain receptors, which are needed to feel pain. This makes the brain different from other body parts. The brain itself cannot feel pain because of this. This fact is vital in neurosurgery, as it lets surgeons work on the brain without causing pain.
Which Parts of the Procedure May Cause Discomfort
Even though the brain can’t feel pain, other parts involved in surgery can. For example, the scalp, skull, and meninges have pain receptors. These areas can cause discomfort during surgery. Also, moving or retracting these tissues can make patients feel uncomfortable.
Patient Sensations During Different Stages
Patients in awake brain surgery might feel different sensations at various times. At the start, they might feel discomfort from local anesthesia or the incision. As the surgery goes on, they might do tasks to check brain function. It’s important for patients to tell the surgical team about any discomfort or unusual feelings. This way, the team can make changes to improve comfort.
The surgical team keeps a close eye on the patient’s comfort throughout. By understanding where discomfort might come from and talking openly, patients can handle awake brain surgery better.
Pain Management Techniques in Awake Craniotomy
Pain management in awake craniotomy uses both medical and psychological methods. It’s key to keep patients comfortable and the surgery successful.
Local Anesthesia for Scalp and Skull
Local anesthetics are used to numb the scalp and skull. This greatly reduces pain during the surgery. Lidocaine and bupivacaine are common choices because they work well without harming the brain.
A famous neurosurgeon once said,
“The use of local anesthesia is a cornerstone in awake craniotomy, allowing us to perform complex procedures while keeping the patient comfortable and cooperative.”
Conscious Sedation Methods
Conscious sedation is also used to keep patients relaxed and comfortable. Sedatives like dexmedetomidine or propofol are used. They help patients relax without affecting their breathing too much.
- Dexmedetomidine provides sedation without significant respiratory depression.
- Propofol offers rapid onset and recovery, allowing for adjustable levels of sedation.
Psychological Pain Management Strategies
Psychological strategies are also important in pain management. Techniques like guided imagery, deep breathing exercises, and cognitive-behavioral therapy help patients deal with anxiety and pain. Preparing patients mentally before surgery helps them handle the procedure better.
As neurosurgery advances, these pain management techniques will keep getting better. They are key to improving patient outcomes and experiences during awake craniotomy.
Preparing for Awake Brain Surgery
Getting ready for awake brain surgery can make you feel less anxious. We’ll walk you through the steps, covering physical and mental preparation.
Physical Preparation and Testing
Before awake brain surgery, physical prep is key. You’ll go through tests to check your health and if you’re ready for the surgery.
- Medical History Review: Your medical team will look at your past health to spot any risks or conditions.
- Imaging Tests: MRI or CT scans will be done to see your brain clearly, helping surgeons plan.
- Physical Examination: A detailed check-up will be done to see how you’re doing and if there are any issues.
What to Expect Before Surgery Day
Knowing what to expect before surgery can ease your worries. It makes sure you’re ready for what’s ahead.
- Pre-Surgery Instructions: You’ll get clear instructions on how to get ready for surgery, including diet and medication changes.
- Logistical Arrangements: You’ll talk about your hospital stay and care after surgery, including travel and family accommodations.
- Final Preparations: The day before, make sure you have all your documents and follow any last-minute instructions from your team.
The Complete Brain Surgery Procedure
Learning about the brain surgery process can ease worries for those facing it. The journey includes several key steps, each vital for a successful surgery.
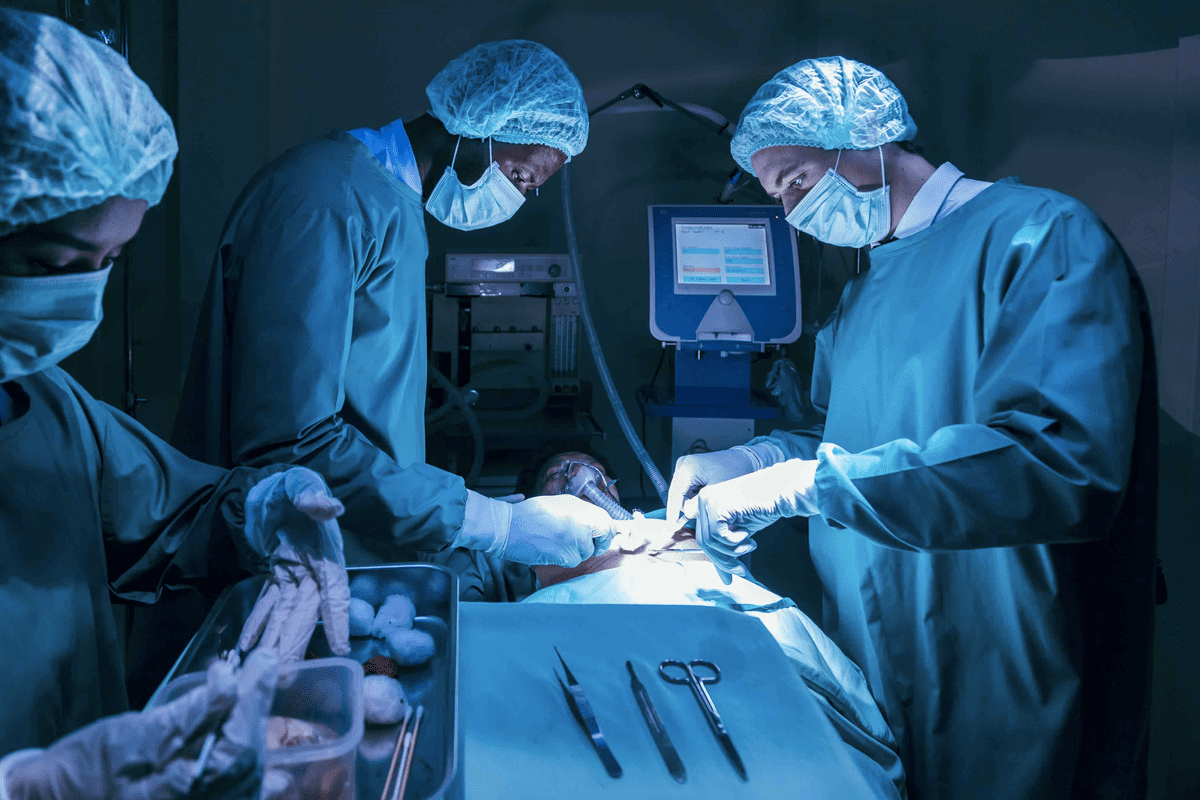
Initial Sedation and Positioning
The first step is sedation and positioning. We give sedation to calm the patient. Then, we place them on the table for the best brain access.
Craniotomy and Dura Opening
Next, we do a craniotomy to reach the brain. We remove a skull part. Then, we open the dura mater to see the brain tissue.
Awakening Process and Intraoperative Testing
After the craniotomy, we wake the patient up slowly. We test the brain to see how it’s working. This is key for mapping the brain and keeping important functions safe.
Tumor Removal or Treatment Phase
With the brain mapped, we start removing the tumor or treating the area. We use the test results to remove the tumor carefully. This way, we avoid harming the brain around it.
The table below shows the main parts of the brain surgery process:
Stage | Description | Purpose |
Initial Sedation and Positioning | Administering sedation and positioning the patient | Relaxation and optimal access |
Craniotomy and Dura Opening | Removing part of the skull and opening the dura mater | Access to the brain |
Awakening Process and Intraoperative Testing | Awakening the patient and testing brain function | Real-time brain mapping |
Tumor Removal or Treatment Phase | Removing the tumor or treating the targeted area | Treating the condition while preserving brain function |
Knowing these steps helps patients prepare for brain surgery. It makes them understand what to expect during their treatment.
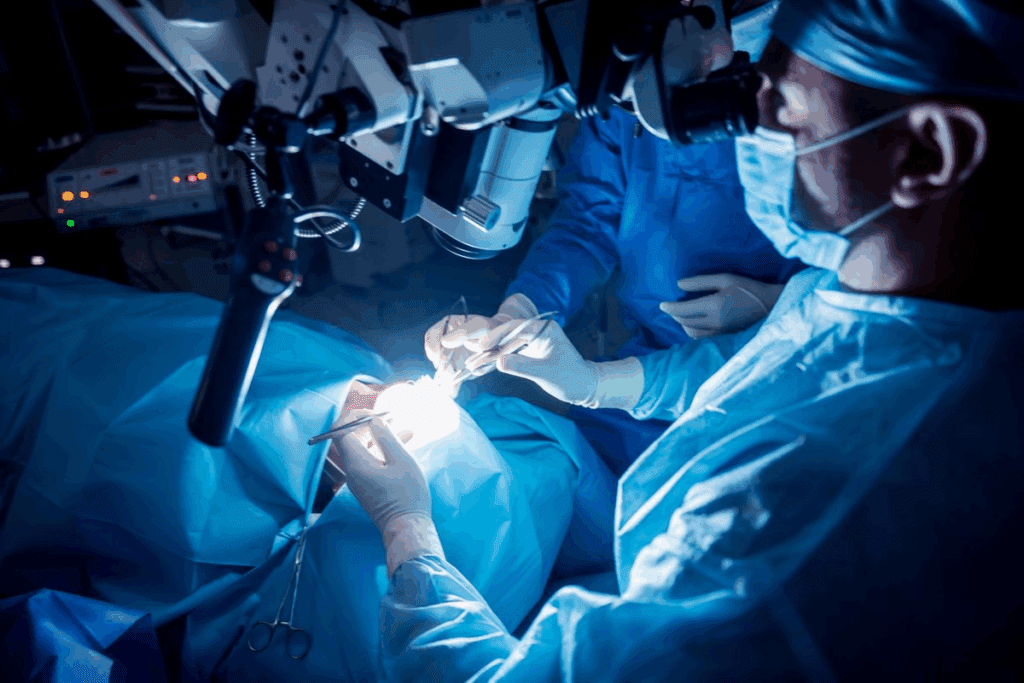
Brain Mapping During Surgery: How It Works
Brain mapping during surgery is a key technique for neurosurgeons. It helps them navigate the brain’s complex areas with precision. This method uses advanced methods to find and protect important brain parts, making surgery safer and more effective.
Electrical Stimulation Techniques
Electrical stimulation is a main method in brain mapping. It uses a small electrical current to stimulate brain areas. Electrical stimulation helps surgeons identify vital brain areas, like those controlling movement, sensation, and language.
We use an electrical stimulator to apply a controlled current to specific brain regions. The patient’s response is then assessed, giving us important information about the function of the stimulated area.
Motor and Sensory Function Testing
Testing motor and sensory functions is a key part of brain mapping. By assessing how the brain responds to different stimuli, we can map out areas responsible for movement and sensation. This is crucial for avoiding damage to these areas during surgery.
For motor function testing, patients may be asked to perform simple movements, such as wiggling their toes or fingers. Sensory testing involves assessing the patient’s sensation in response to various stimuli, helping us to delineate the sensory cortex.
Language and Cognitive Assessment
Language and cognitive functions are also meticulously mapped during awake brain surgery. This involves a series of tests designed to evaluate the patient’s language abilities, such as naming objects, reading, or performing simple arithmetic. These assessments help us identify areas crucial for language processing, allowing us to preserve them during the surgery.
Cognitive functions, including memory and attention, are also assessed. By understanding how different parts of the brain contribute to these functions, we can minimize the risk of post-operative cognitive deficits.
What Patients Experience While Awake
During awake brain surgery, patients stay awake and alert. This lets them talk with the surgical team in real time. It’s a special part of the surgery that helps surgeons check brain function as they work.
Common Sensations and Awareness Levels
Patients might feel different things during surgery. Some might feel pressure or hear tools being used. Others might feel like they’re watching from outside their body. How awake they feel can change, from very alert to a bit sleepy.
The kind of anesthesia used and how the patient reacts to it can affect these feelings. Our team keeps a close eye on how comfortable the patient is. They adjust the sedation to make sure the experience is as smooth as possible.
Communication with the Surgical Team
Talking well with the surgical team is key during awake brain surgery. Patients should tell the team about any feelings or changes they notice. This helps the surgeons understand the brain better and make the right moves during surgery.
We use different ways to make sure communication is clear. This includes giving simple commands, asking questions, and having patients do tasks. This interaction is crucial for the surgery’s success.
Tasks Patients Might Perform During Surgery
Patients might be asked to do simple tasks to check brain function. These tasks could be moving their limbs, speaking, or reacting to sounds or pictures. These activities help the team find and protect important brain areas.
Task Type | Purpose | Examples |
Motor Tasks | Assess motor function and identify areas controlling movement. | Moving fingers, toes, or limbs on command. |
Language Tasks | Evaluate language processing and identify areas crucial for speech. | Naming objects, reading sentences, or engaging in conversation. |
Sensory Tasks | Assess sensory perception and identify areas responsible for sensation. | Identifying tactile sensations, responding to visual or auditory stimuli. |
By doing these tasks, patients help make their surgery better. The information they provide is very important. It helps us map brain function and guide the surgery.
Ideal Candidates for Awake Brain Surgery
Finding the right candidates for awake brain surgery is complex. It looks at both medical and psychological aspects. The goal is to pick patients who can safely have the surgery and get the most benefits.
Medical Criteria for Selection
The medical criteria for choosing candidates include the type and location of the brain lesion. Patients with tumors or lesions in areas that control important functions like speech or movement are often good candidates. The size and depth of the lesion also matter.
We use advanced imaging like functional MRI (fMRI) and diffusion tensor imaging (DTI) to check the lesion’s details. This helps us decide if awake surgery is the best option.
Medical Criteria | Description | Importance |
Type of Lesion | Tumors, vascular malformations, or epilepsy foci | High |
Location of Lesion | Eloquent areas controlling speech, movement, or sensation | High |
Size and Depth | Assessed using advanced imaging techniques | Medium |
Psychological Factors Considered
Psychological factors are key in deciding if a patient is right for awake brain surgery. We check if the patient can stay calm and cooperate during the surgery. We also look at their mental health and how well they handle stress.
Patients with anxiety, claustrophobia, or other mental health issues are evaluated carefully. We also consider their understanding of the surgery and what they expect.
When Awake Surgery Is Not Recommended
Awake brain surgery is not for everyone. Patients with severe heart disease or uncontrolled seizures might not be good candidates. Also, those who can’t cooperate during the surgery due to cognitive or psychological issues are not ideal.
We weigh the benefits and risks for each patient to choose the best surgical approach. This ensures the best outcomes for our patients.
In conclusion, picking the right candidates for awake brain surgery is a detailed process. It looks at both medical and psychological factors. By carefully evaluating these, we can ensure the best results for our patients.
Recovery After Awake Craniotomy
The journey to full recovery after awake brain surgery has many stages. It starts with immediate care and goes all the way to long-term healing. Knowing what to expect at each stage helps patients and their families prepare for the road ahead.
Immediate Post-Operative Experience
Right after surgery, patients go to the recovery room. There, they are watched closely for any problems. The team checks for brain issues, manages pain, and deals with any discomfort. Patients might feel:
- Fatigue and drowsiness from the anesthesia
- Headache or pain at the surgical site
- Nausea or vomiting
- Confusion or disorientation
These symptoms are usually short-lived and managed with medicine and rest. Our team works hard to keep patients comfortable during this important time.
Hospital Stay Duration
The time spent in the hospital after awake craniotomy varies. It depends on the patient’s condition and the surgery’s complexity. Generally, patients stay for:
- 1-3 days for observation and initial recovery
- Monitoring for potential complications
- Adjusting medications and managing pain
Our hospital team helps patients smoothly move from the hospital to home. They provide the necessary instructions and support.
Long-Term Recovery Timeline
Recovering fully from awake brain surgery can take weeks to months. The recovery timeline includes:
- Initial recovery phase (1-2 weeks): Rest and gradual return to light activities
- Intermediate phase (2-6 weeks): Gradual increase in activity levels and return to most daily routines
- Advanced recovery phase (3-6 months): Full recovery of strength and return to normal activities, including work and exercise
It’s crucial for patients to follow their surgeon’s advice and attend follow-up appointments. This helps monitor progress and address any concerns.
Returning to Normal Activities
Returning to normal activities after awake craniotomy should be gradual. Patients should follow their doctor’s guidance. They are advised to:
- Avoid heavy lifting and bending
- Gradually increase physical activity
- Monitor for signs of complications or neurological changes
By following these guidelines and staying in touch with their healthcare providers, patients can ensure a safe and effective recovery.
Risks and Complications of Awake Brain Surgery
Awake brain surgery has many benefits, but it also comes with risks. It’s important for patients to know about these risks. Like any surgery, awake craniotomy has its own set of risks.
Surgical Complications
Complications can happen during or after awake brain surgery. These might include infection, bleeding, or swelling in the brain. We do our best to avoid these risks, but it’s good for patients to know they can happen.
“The risk of infection is a big worry in any surgery, including awake brain surgery,” say doctors. We follow strict infection control to lower this risk.
- Infection control measures are strictly followed.
- Bleeding risks are managed through careful patient selection and monitoring.
- Swelling is controlled with medication and other treatments.
Anesthesia-Related Risks
Even though the brain can’t feel pain, anesthesia-related risks are still a concern. Local anesthesia numbs the scalp and skull. While safe, there are risks to consider.
Some patients might feel discomfort or pain during the surgery, but this is rare. We use conscious sedation to help patients relax and reduce discomfort.
Psychological Effects and Management
The psychological effects of awake brain surgery are important to consider. Patients might feel anxious or stressed about being awake during the surgery. We offer psychological support and counseling to help them prepare and cope.
Managing psychological effects is key for a good outcome. This includes counseling before surgery, support during it, and care after. We help address any emotional or psychological challenges that may come up.
Knowing the risks and complications of awake brain surgery helps patients make informed choices. We are dedicated to providing full care and support throughout the process.
Modern Advancements in Neurosurgical Techniques
Neurosurgery has seen big changes, making surgeries safer and more effective. New technologies and methods have greatly improved patient results.
Minimally Invasive Approaches
Minimally invasive neurosurgery is now more common. It aims to reduce recovery time and scarring. With endoscopic surgery and stereotactic radiosurgery, surgeons can do complex tasks with less harm to the brain.
- Reduced Risk: These procedures often have fewer complications.
- Faster Recovery: Patients usually have shorter hospital stays and get back to normal faster.
- Less Pain: Smaller cuts mean less pain after surgery.
Improved Imaging and Mapping Technologies
New imaging tech like fMRI and DTI has improved brain mapping. This is key for awake brain surgeries.
These tools help us:
- Make detailed brain function maps.
- Spot areas to avoid during surgery.
- Plan the safest, most effective surgery.
Future Directions in Awake Neurosurgery
The future of awake neurosurgery is bright. Ongoing research aims to improve outcomes even more. Key areas include:
- Advanced Neuromonitoring: Watching brain function in real-time during surgery.
- Personalized Medicine: Customizing surgery to fit each patient’s needs.
- Robot-Assisted Surgery: Using robots to increase precision.
We’re always looking to do better in neurosurgery. Our goal is to give the best care and improve our patients’ lives.
Conclusion: Balancing Consciousness and Comfort in Brain Surgery
Awake brain surgery is a fine line between being awake and feeling comfortable. We’ve looked into how this works, from its start to today’s advanced techniques.
Success in awake brain surgery depends on managing pain well. This is done with local anesthesia and conscious sedation. Knowing why this surgery is needed helps us see its importance.
As neurosurgery gets better, we must focus on patient comfort and awareness. This ensures the best results for those needing this complex surgery.
FAQ
What is awake brain surgery?
Awake brain surgery, also known as awake craniotomy, is a procedure where the patient stays awake. This lets the team watch brain function in real-time. It’s especially useful for surgeries near areas that control speech, movement, and sensation.
Does awake brain surgery hurt?
The brain can’t feel pain because it lacks pain receptors. But, patients might feel discomfort during parts of the surgery. This could be when the scalp is cut or the skull is opened. To reduce pain, doctors use local anesthesia and conscious sedation.
Why is brain mapping necessary during awake brain surgery?
Brain mapping is key to avoid damaging important brain areas during surgery. Techniques like electrical stimulation help the team find and protect these areas. This ensures the surgery doesn’t harm vital functions.
What are the advantages of awake brain surgery over traditional surgery?
Awake brain surgery is more precise and safer. It helps avoid damaging critical areas. This can lead to better outcomes for patients with brain tumors or other conditions in important brain regions.
How long does awake brain surgery typically last?
The time awake brain surgery varies. It depends on the surgery’s complexity and the condition being treated. On average, it can last from 4 to 12 hours, including preparation and recovery.
What kind of preparation is required for awake brain surgery?
Preparing for awake brain surgery includes a medical check-up and psychological assessment. Patients get detailed instructions on pre-operative care. They’re also told what to expect during the surgery and how to manage anxiety or discomfort.
How is pain managed during awake craniotomy?
Pain management involves local anesthesia for the scalp and skull, and conscious sedation to relax the patient. Psychological strategies are also used to handle discomfort or anxiety.
What are the potential risks and complications of awake brain surgery?
Awake brain surgery is generally safe but carries risks like infection, bleeding, seizures, and neurological deficits. These risks are minimized by careful patient selection, advanced techniques, and close monitoring.
How long is the recovery period after awake brain surgery?
Recovery time varies, but most patients stay in the hospital for a few days to a week. Full recovery can take several weeks to months, depending on the surgery’s extent and the patient’s health.
Can anyone undergo awake brain surgery?
Not everyone is a good candidate for awake brain surgery. The decision depends on the brain condition’s location and nature, the patient’s health, and their ability to cooperate during the surgery.
What advancements have improved the outcomes of awake brain surgery?
Advances in neurosurgery, like minimally invasive techniques and better imaging, have made awake brain surgery safer and more effective. These advancements have greatly improved outcomes.