Last Updated on December 2, 2025 by Bilal Hasdemir
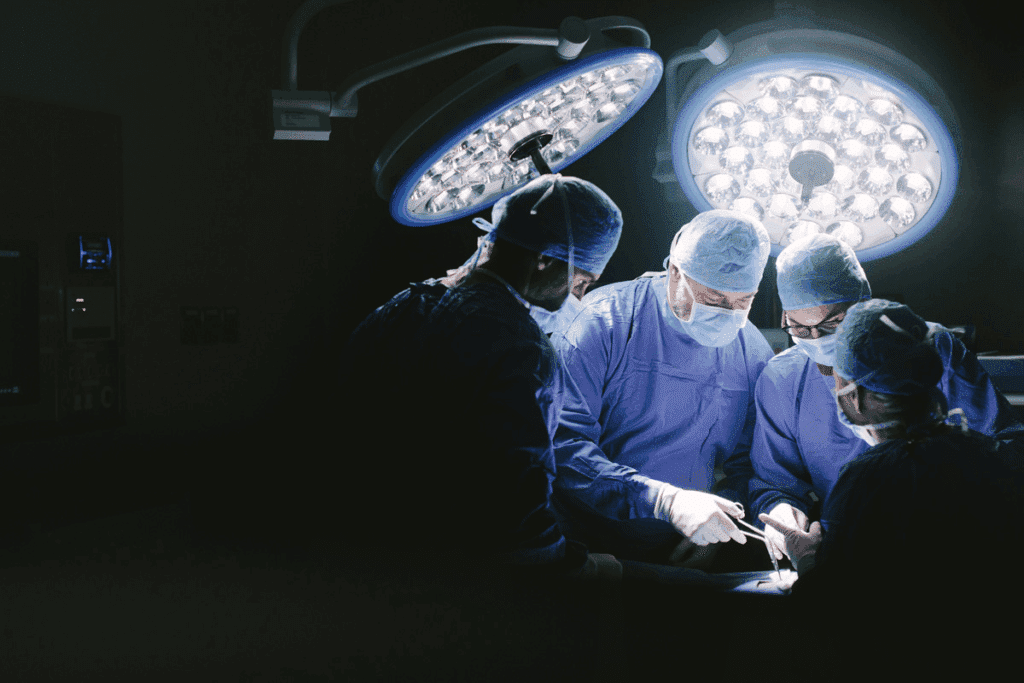
Awake brain surgery is a complex and delicate procedure. It has gained a lot of attention in recent years. Did you know that nearly 90% of patients undergoing awake tumor surgery report a successful outcome with minimal complications?
The thought of being awake during such a critical procedure can be daunting. But this technique allows our skilled surgeons to remove tumors or lesions while you remain responsive. This ensures the best possible outcome. The possibility of movement during the procedure is carefully considered. Our team takes every precaution to ensure your safety and comfort.
Key Takeaways
- Awake brain surgery is a complex procedure that requires careful planning.
- The technique involves removing tumors or lesions while the patient is responsive.
- Movement during the procedure is carefully monitored and managed.
- Our team of experts guides you through the process, ensuring the best care possible.
- Awake brain surgery has shown promising results in treating brain tumors and lesions.
- What Is Awake Brain Surgery?

Awake brain surgery is a cutting-edge method. It lets neurosurgeons work on the brain while the patient is awake. This method has changed neurosurgery, helping with brain tumors and lesions.
Definition and Medical Purpose
Awake brain surgery, also known as awake craniotomy, is a complex procedure. The patient stays awake and can respond during surgery. This helps surgeons avoid damaging important brain areas.
By keeping the patient awake, surgeons can check brain functions like speech and movement. This makes sure the surgery goes smoothly and safely.
Historical Development of the Technique
The idea of awake brain surgery started in the early 20th century for epilepsy treatment. Over time, it has become safer and more precise. Now, it’s used for many conditions, including brain tumors.
Our team is experienced in awake brain surgery. We aim to give our patients the best care and results. We keep up with the latest technology to improve our methods.
Aspect | Description | Benefit |
Real-time Monitoring | Surgeons can assess brain function during surgery | Minimizes risk to critical brain areas |
Patient Feedback | Patients can respond during the procedure | Enhances precision in navigating brain structures |
Historical Evolution | Technique has evolved from epilepsy treatment to various brain conditions | Expanded applications in neurosurgery |
When Is Awake Brain Surgery Necessary?
Choosing awake brain surgery depends on several factors. These include the type and location of the brain tumor or lesion. It’s usually recommended for tumors in critical brain areas.
Types of Brain Tumors and Conditions
Awake brain surgery is needed for tumors near vital functions. This includes speech, motor function, or sensory perception. Common tumors needing this surgery are gliomas, meningiomas, and metastatic brain tumors.
Tumor Type | Characteristics | Awake Surgery Necessity |
Gliomas | Originate from glial cells, can be low-grade or high-grade | High |
Meningiomas | Typically benign, arise from meninges | Moderate to High |
Metastatic Brain Tumors | Spread from other cancers, such as lung, breast, or melanoma | High |
Critical Brain Areas Requiring Conscious Monitoring
Certain brain areas need monitoring during surgery. These include those for speech, motor function, and sensory perception. Our team uses advanced mapping to protect these areas.
Patient Selection Criteria
Choosing patients for awake brain surgery is thorough. We look at their health, tumor type and location, and ability to cooperate. We discuss the risks and benefits with each patient.
By carefully choosing patients and using advanced techniques, we aim to improve outcomes. This approach helps minimize risks.
The Step-by-Step Process of Awake Brain Surgery
Awake brain surgery is a detailed process that ensures safety and success. We’ll guide you through the main steps, from preparation to the surgery itself.
Pre-Surgical Preparation
Before awake brain surgery, patients go through a lot of preparation. This includes:
- Detailed medical evaluations to check overall health and the specific condition needing surgery.
- Imaging studies, like MRI or CT scans, to find the exact area of the brain to operate on.
- Talking with the surgical team about what to expect during and after the surgery.
- Psychological preparation to handle anxiety and understand their role during surgery.
Anesthesia Protocols: Asleep-Awake-Asleep Technique
The asleep-awake-asleep technique is often used in awake brain surgery. Here’s how it works:
- The patient starts under general anesthesia for comfort during skull opening.
- The patient is then woken up during the key part of the surgery, allowing for real-time brain function monitoring.
- After the critical part, the patient is put back under anesthesia for the rest of the surgery.
Surgical Phases and Timeline
The surgery has several phases:
- Preparation Phase: Setting up monitoring equipment and giving initial anesthesia.
- Surgical Exposure: The team carefully exposes the brain area to be operated on.
- Awake Phase: The patient is woken up, and brain functions are monitored in real-time.
- Completion of Surgery: After the key phase, the patient is anesthetized again, and the surgery is finished.
Knowing these steps helps patients and their families prepare for the procedure and recovery.
Movement During Brain Surgery: What’s Possible?
It’s important to know what’s possible and what’s not during awake brain surgery. Patients must stay awake and alert. This helps surgeons avoid damaging important brain areas.
Types of Movements Patients Can Perform
Patients may be asked to do different movements during surgery. These can include:
- Simple motor tasks, such as squeezing a hand or moving a limb
- More complex actions, like grasping or manipulating objects
- Repetitive movements to test motor control and coordination
These tasks help surgeons understand brain function. They also spot any risks during the surgery.
Movement Limitations and Restrictions
While patients can move during surgery, there are limits for safety. For example:
- Patients are secured to prevent too much movement
- Certain movements are restricted to protect the surgical area
- Surgeons and anesthesiologists watch the patient closely and adjust as needed
These steps help reduce risks and improve outcomes.
How Surgeons Manage Patient Movement
Managing patient movement during surgery is key. Our team uses several methods, including:
Strategy | Description |
Pre-Surgical Planning | Planning ahead to prepare for possible movements |
Real-Time Monitoring | Watching the patient’s vital signs and brain activity during surgery |
Adjustable Restraints | Using restraints that can be adjusted to safely hold the patient while allowing movement |
By using these methods, we ensure the surgery is done safely and effectively, even with patient movement.
Neurological Testing and Movement Assessment
Neurological testing is key in awake brain surgery. It lets our team check brain activity as it happens. These tests help us see how the patient’s brain is working during surgery. This way, we can make the right choices and adjust as needed.
Motor Function Evaluation During Surgery
We check the patient’s motor skills during awake brain surgery. We look at muscle strength, reflexes, and coordination. This helps us avoid touching parts of the brain that control important movements.
Motor function testing happens right as we’re doing the surgery. Our surgeons can change their approach based on what they see. They might ask the patient to move their toes or fingers to check how they respond.
Speech and Language Testing
Speech and language tests are very important in awake brain surgery. They’re key when we’re near areas of the brain that handle language. These tests help us keep language skills safe, reducing the chance of problems after surgery.
We do language mapping to find out where language is processed in the brain. We use tasks like naming objects, reading, and talking to see how language works in the patient’s brain.
“The ability to perform real-time language testing during surgery has revolutionized our approach to brain surgery, allowing us to preserve critical language functions in our patients.”
Cognitive Tasks Performed While Awake
Patients also do cognitive tasks while they’re awake. These tests check memory, attention, and problem-solving skills. They give us insights into how the brain is working.
Cognitive testing helps us plan the surgery to protect the brain. By asking patients to remember things or solve math problems, we see how the surgery might affect their thinking.
The Patient Experience: What It Feels Like
Going through awake brain surgery is a unique journey. Patients often say it’s both tough and enlightening. It’s key to know what makes up the patient’s experience during the surgery.
Sensations and Awareness During the Procedure
Patients might feel different things during awake brain surgery. They could feel pressure, discomfort, or even pain. But, thanks to good pain management, pain is rare.
It’s important for patients to tell the surgical team if they’re feeling pain. This way, the team can adjust things to make the patient more comfortable.
Patients usually know what’s going on around them during the surgery. This can make them feel both at ease and anxious. The surgical team is there to reassure and support the patient, helping to ease their worries.
Pain Management Strategies
Managing pain is a big part of awake brain surgery. There are many ways to reduce pain, like local anesthesia for the scalp and sedatives to relax the patient. The “asleep-awake-asleep” method is one way to do this, where the patient is sedated, then awake, and then sedated again.
Patients are encouraged to share how much pain they’re in. This helps the surgical team adjust things to keep the patient comfortable.
Psychological and Emotional Aspects
The mind and emotions play a big role in awake brain surgery. Patients might feel anxious, scared, relieved, or hopeful. The support and communication from the surgical team are key in helping with these feelings.
Getting ready for the surgery beforehand is also important. Being prepared helps patients deal with their anxiety and focus on the positive aspects of their treatment.
Preparing Physically and Mentally for Awake Brain Surgery
To have a successful awake brain surgery, patients need to get ready both physically and mentally. This detailed preparation is key for a smooth surgery and the best results.
Physical Conditioning Requirements
Being in good physical shape is very important before awake brain surgery. Patients should manage any health issues, like diabetes or high blood pressure, and live a healthy lifestyle.
It’s good to do some light exercise to get your body ready. But, always talk to your doctor before starting any new workout. A strong body can handle the surgery and recovery better.
Physical Conditioning Aspect | Recommendation |
Managing Chronic Conditions | Work with your primary care physician to ensure conditions like diabetes and hypertension are well-managed. |
Exercise | Engage in gentle exercises like walking or yoga, after consulting with your healthcare provider. |
Nutrition | Maintain a balanced diet rich in nutrients to support your body’s needs during recovery. |
Psychological Preparation Techniques
Getting ready mentally is just as important as getting ready physically. There are many ways to lower anxiety and get ready for surgery. These include:
- Counseling: Talking to a mental health expert can help face fears or worries.
- Relaxation Techniques: Activities like meditation, deep breathing, or progressive muscle relaxation can lessen stress.
- Support Groups: Being part of a support group can give a sense of community and understanding.
Practice Sessions and Movement Rehearsals
Practice sessions and movement rehearsals are a big part of getting ready. They help patients know what to expect and how to work with the surgical team. Patients might practice staying calm, doing certain movements, or following commands.
By practicing these actions, patients can feel less anxious and more in control during the surgery. Our team works with patients to make these practice sessions fit their needs and the surgery’s requirements.
In summary, getting ready for awake brain surgery needs a complete approach. By focusing on physical health, mental readiness, and practice sessions, patients can greatly help their surgery’s success.
Recovery and Rehabilitation After Brain Surgery
Recovery and rehabilitation are key after awake brain surgery. They need careful management and support. The journey includes immediate care and long-term rehab to help patients regain strength and return to normal life.
Immediate Post-Operative Experience
Right after surgery, patients are watched closely in the recovery room or ICU. We focus on managing pain, preventing problems, and checking brain function. Patients might feel pain, tiredness, or confusion, but these are usually short-term and can be managed.
Key aspects of immediate post-operative care include:
- Monitoring of vital signs and neurological status
- Pain management through medication
- Prevention of infections and other complications
Short-Term Recovery Timeline
The short-term recovery lasts a few weeks after surgery. Patients might face headaches, tiredness, and brain changes. We help manage these symptoms and support their recovery.
The recovery timeline varies based on surgery extent and patient health.
Week | Typical Recovery Milestones |
1-2 | Initial recovery, managing pain and basic self-care |
2-4 | Gradual improvement in strength and cognitive function |
4-6 | Return to light activities and social interactions |
Long-Term Rehabilitation and Return to Activities
Long-term rehab is vital for full recovery. It focuses on regaining strength, brain function, and independence. We create a rehab plan that might include physical, occupational, and speech therapy, based on the patient’s needs.
As patients get better, we encourage them to slowly return to their usual activities. This includes work, exercise, and social events. Our goal is to help them fully recover and improve their quality of life.
Risks and Complications of Awake Craniotomy
Awake craniotomy is usually safe, but there are risks and complications. These risks are important to know about before the surgery.
Surgical Complications
During awake craniotomy, problems like infection, bleeding, and brain damage can happen. We use the latest techniques and careful wound care to avoid these issues.
Common Surgical Complications:
- Infection
- Bleeding or hemorrhage
- Cerebral edema
- Damage to surrounding brain tissue
Anesthesia-Related Risks
Anesthesia risks are also a concern during awake craniotomy. The “asleep-awake-asleep” method aims to reduce pain. Yet, there are risks like breathing and heart problems.
Anesthesia-Related Risk | Description | Mitigation Strategy |
Respiratory Complications | Issues related to breathing, such as obstruction or depression | Close monitoring of respiratory function |
Cardiac Complications | Issues related to heart function, such as arrhythmias or ischemia | Continuous cardiac monitoring and pre-operative cardiac evaluation |
Movement-Induced Complications
Moving unexpectedly during surgery can cause problems. We help patients stay calm and in place. This includes using gentle restraints and careful positioning.
Knowing the risks of awake craniotomy helps patients prepare. It lets them make informed choices about their care.
Technological Advancements in Awake Brain Surgery
Technology has changed awake brain surgery a lot. It makes the surgery safer and more effective. New tech has improved how well patients do and opened up new ways to operate.
Intraoperative Mapping Technologies
Intraoperative mapping is key in awake brain surgery. It helps surgeons find important brain spots. With intraoperative MRI and electrocortical stimulation mapping, they can see brain functions live. This cuts down the chance of harming key areas.
Improved Surgical Instruments and Techniques
New surgical tools and methods have made awake brain surgery better. Microsurgical techniques and clear images help surgeons be more precise. Laser technology and ultrasonic aspirators also help remove tumors safely.
Enhanced Monitoring Systems
Monitoring systems are very important in awake brain surgery. They keep an eye on the patient’s brain activity all the time. With neurophysiological monitoring like EEG and EMG, surgeons can make quick changes if needed. This helps ensure the best results for the patient.
Real Patient Stories: Movement During Awake Brain Surgery
Real patient stories show the details of awake brain surgery. They talk about the challenges and the good results. This surgery keeps patients awake during parts of the operation.
Looking at these stories helps us understand what it’s like. Many patients have done well after the surgery. Some even got back to their usual activities quickly.
Success Stories and Positive Outcomes
For example, a patient might talk about being able to move their limbs during surgery. This helped the doctors understand the brain better.
These success stories show how well awake brain surgery works. They also highlight the progress in neurosurgery and patient care. The hard work and skill of the medical team are clear.
Challenges and Unexpected Situations
But, there are also tough moments during awake brain surgery. Patients might feel anxious or uncomfortable. They might also have unexpected reactions that need quick action from the doctors.
A patient might feel unexpected sensations or struggle with movements. This could be because of where the tumor is or the patient’s health. The team’s quick thinking is key to success.
Patient Advice and Recommendations
Patients who have had awake brain surgery share useful tips. They talk about the importance of being mentally ready and having support during recovery.
One piece of advice is to stay calm and listen to the doctors. This can greatly affect the surgery’s success. Also, being ready for being awake during surgery can help manage worries.
Alternatives When Awake Brain Surgery Isn’t Possible
When awake brain surgery isn’t an option, we look at other treatments. Every patient is different, so what works for one might not work for another. We explore both surgical and non-surgical options when awake surgery isn’t possible.
Conventional Surgery Options
Conventional surgery uses general anesthesia. It’s used when the tumor or area doesn’t need the patient to be awake. Conventional brain surgery can remove tumors or fix damaged brain tissue.
We use advanced imaging to guide surgeons during these operations. This ensures accuracy and reduces risks. The choice of conventional surgery is made after careful evaluation and talking with the patient and their family.
Non-Surgical Treatment Approaches
For some, non-surgical treatments are recommended. These include radiation therapy, chemotherapy, or other treatments. The choice depends on the tumor or condition, its size, and the patient’s health.
We create a personalized treatment plan for each patient. Radiation therapy can shrink tumors that can’t be removed by surgery.
Our team provides full care, including support during and after treatment. We aim to empower our patients with the knowledge to make informed decisions about their care.
Conclusion
Awake brain surgery is a complex and delicate procedure. It needs careful consideration and planning. We’ve looked at its definition, medical purpose, step-by-step process, and risks in this article.
Our team is committed to giving the best care to our patients. We know how important precise testing and movement assessment are during the surgery. This ensures the best results for our patients.
We keep improving our approach to awake brain surgery. We’re dedicated to delivering top-notch healthcare to our international patients. By understanding awake brain surgery, we can better handle its challenges and opportunities.
FAQ
What is awake brain surgery?
Awake brain surgery is a special surgery where the patient stays awake. This lets surgeons check how the brain works and make changes if needed.
Why is awake brain surgery necessary?
It’s needed when the tumor or lesion is in a key brain area. This area controls speech or movement. It helps avoid damage to these important parts.
Can you move during awake brain surgery?
Yes, patients might have to move a little during surgery. This helps surgeons check the brain’s function. But, the movements are controlled and limited.
What kind of movements can patients perform during awake brain surgery?
Patients can do different movements. For example, they might move their limbs or speak. This helps surgeons check how well the brain works.
How is pain managed during awake brain surgery?
To keep patients comfortable, doctors use local anesthesia and sedation. This helps manage pain during the surgery.
What are the risks and complications of awake craniotomy?
There are risks like surgical problems and issues with anesthesia. Also, moving too much can cause complications. But, these risks are low with careful planning and execution.
How long does it take to recover from awake brain surgery?
Recovery time varies. But, most patients need weeks to months to get back to normal. It depends on the surgery and the patient’s health.
What are the benefits of awake brain surgery?
It has many benefits. For example, it reduces the risk of harming key brain areas. It also leads to better outcomes and faster recovery.
Are there alternative treatment options when awake brain surgery isn’t possible?
Yes, there are other options. These include regular surgery and non-surgical methods. They are used when awake brain surgery isn’t an option.
How can I prepare physically and mentally for awake brain surgery?
Getting physically fit and mentally ready can help. Practice sessions and psychological preparation can improve your chances of a good outcome.
What technological advancements have improved awake brain surgery?
New technologies have made surgery safer and more effective. These include better mapping tools, instruments, and monitoring systems.
What is the role of neurological testing during awake brain surgery?
Neurological tests are key during surgery. They check motor function, speech, and thinking. This helps surgeons make the right adjustments during the surgery.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4710339/