Last Updated on December 1, 2025 by Bilal Hasdemir

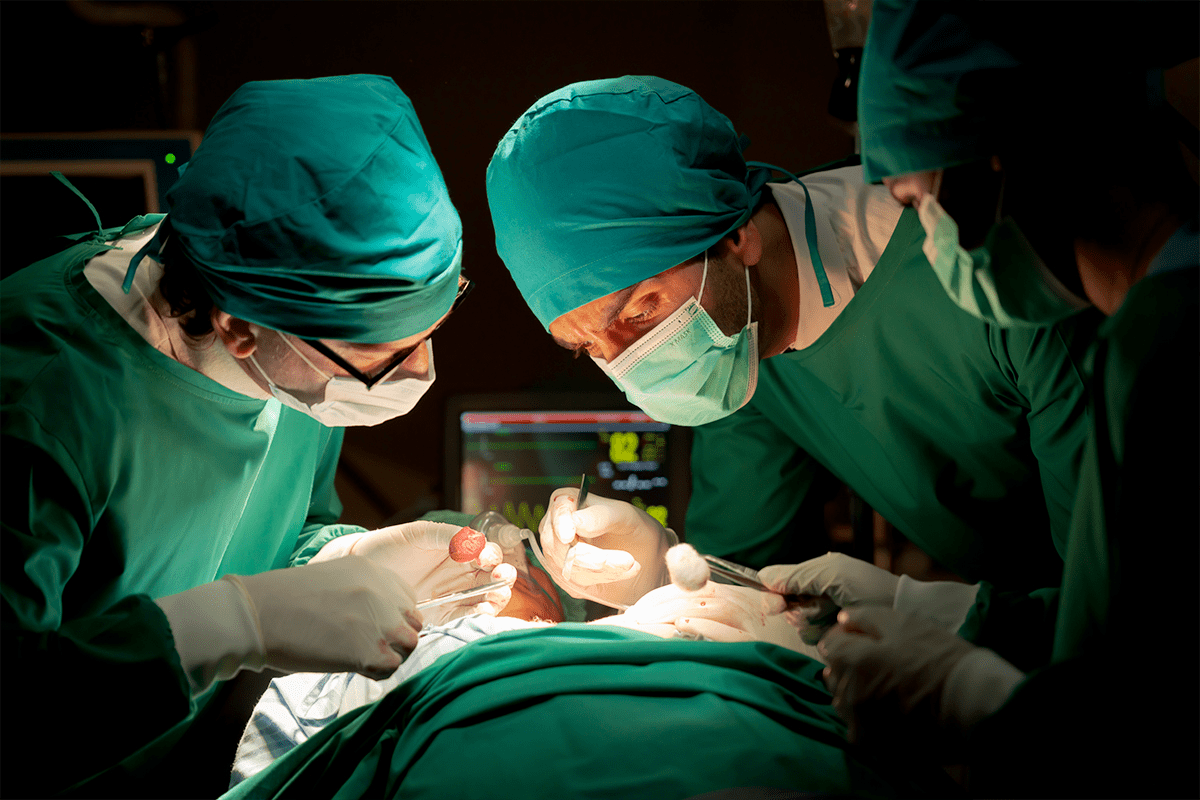
Discover the amazing facts about awake brain tumor surgery. Learn why surgeons wake you up and the critical benefits of this technique. Awake brain surgery is a complex procedure that necessitates the patient’s consciousness.
This type of surgery is used to treat conditions such as brain tumors or epileptic seizures. By keeping the patient awake, surgeons can monitor the brain‘s function in real-time. This reduces the risk of damage to critical areas.
Key Takeaways
- Awake brain surgery is a complex procedure that necessitates the patient’s consciousness.
- It’s used to treat certain neurological conditions, including brain tumors and epileptic seizures.
- The procedure allows surgeons to monitor the brain’s function in real-time.
- This real-time monitoring reduces the risk of damage to critical areas of the brain.
- Awake brain surgery is a complex procedure that necessitates the patient’s consciousness. team.
Awake brain surgery is a complex procedure that necessitates the patient’s consciousness.

Awake brain surgery is a complex procedure that necessitates the patient’s consciousness.
What is Awake Craniotomy?
Awake brain surgery is a complex procedure that necessitates the patient’s consciousness.
When Doctors Recommend Staying Conscious
Doctors suggest awake craniotomy for a few main reasons. It’s mainly for tumors in sensitive spots. The surgery lets doctors get feedback from the patient, keeping important brain functions safe. The choice to do an awake craniotomy depends on the tumor’s location, size, and the patient’s health.
Procedure | Benefits | Risks |
Awake Craniotomy | Real-time monitoring of brain activity, precise tumor removal | Patient anxiety, possible complications during surgery |
Awake brain surgery is a complex procedure that necessitates the patient’s consciousness. | Well-known method, patient is asleep | Risk of damage to key brain areas, longer recovery |
Knowing about awake brain surgery helps patients get ready for it. It shows how far neurosurgical techniques and care for patients have come.
The Science Behind Conscious Brain Procedures
Awake brain surgery is a complex procedure that necessitates the patient’s consciousness.
How the Brain Lacks Pain Receptors
Brain tissue doesn’t have pain receptors, which is key for awake craniotomy. Even though the scalp is numbed, patients might feel pressure or vibrations during surgery. This is why patients don’t feel pain during brain surgery.
Consciousness and Brain Function During Surgery
During awake brain surgery, patients stay awake. This lets doctors watch how the brain works in real time. It’s very important for surgeries near areas that control speech, movement, and thinking.
Being able to talk to the patient during surgery helps doctors avoid damaging these critical areas.
Local vs. General Anesthesia in Neurosurgery
Choosing between local and general anesthesia depends on the surgery. Local anesthesia is used for awake craniotomies, so patients can stay awake and respond. General anesthesia is used when patients need to be asleep.
Knowing the difference between local and general anesthesia helps us understand neurosurgery better. It shows the careful thought that goes into picking the right anesthesia for each surgery.
Brain Tumor Surgery: When Patients Stay Awake
Brain tumor surgery needs precision. Patients often stay awake to help the doctors. This way, they can see how the brain works in real-time. It’s key when tumors are close to important brain parts.
Types of Tumors Requiring Awake Surgery
Awake brain surgery is a complex procedure that necessitates the patient’s consciousness.
Mapping Critical Brain Areas
Brain mapping is the best way to find and keep safe important brain parts. During awake surgery, doctors use electrical stimulation to see how the brain works. This helps them avoid harming these areas.
Protecting Speech, Motor, and Cognitive Functions
The main goal of awake brain surgery is to remove tumors while keeping brain functions safe. Doctors use brain mapping and watch the patient’s brain functions closely during surgery.
Real-time Functional Testing
During surgery, patients do tasks to check their brain functions. They might speak, move limbs, or do cognitive tasks. This lets the doctors adjust their approach as needed.
Neuropsychological Monitoring
Neuropsychological monitoring is key in awake brain surgery. It checks the patient’s thinking and feelings during surgery. This helps the doctors make the best choices for the patient.
Function | Test/Task | Purpose |
Speech | Reading, naming objects | Assess language processing |
Motor | Moving limbs on command | Evaluate motor control |
Cognitive | Memory recall, problem-solving | Assess cognitive function |
The Patient Experience During Awake Brain Surgery
Awake brain surgery can seem scary, but with the right prep, patients can feel confident. It’s not just the surgery; it’s also the prep and the patient’s role during it.
Preoperative Preparation and Psychological Counseling
Before surgery, patients get ready with psychological counseling. This helps them face their fears and anxieties. It’s key to being mentally ready for the surgery.
Preoperative preparation includes talks with the surgical team. They cover the patient’s history, the surgery details, and what to expect. This helps patients understand what’s happening.
What Patients Actually Feel and See
During awake brain surgery, patients are awake and might feel some things. But they won’t feel pain because of local anesthesia. Everyone’s experience is different, based on their own situation and the surgery type.
Patients might see the team working and do tasks to help the surgeons. This is a special part of awake brain surgery.
Communication Between Surgical Team and Patient
Good communication between the surgical team and the patient is key. The team keeps an eye on the patient’s brain functions and shares updates on the surgery.
Tasks Patients Might Perform
Patients might do tasks like identifying pictures or words, counting, or naming objects. These tasks help the surgeons know which brain areas are important.
Task | Purpose |
Identifying pictures or words | To map language areas of the brain |
Counting or naming objects | To assess cognitive and motor functions |
Patient Testimonials
Many patients say they felt a mix of emotions during awake brain surgery. But they often look back positively. They talk about the care and support they received.
Patients often say the team’s support was key. They also value being well-informed and prepared.
Types of Brain Surgeries and Consciousness Levels
Different brain surgeries need different levels of consciousness. This can range from being fully asleep to fully awake. The level needed depends on the surgery type and the patient’s needs.
Fully Asleep Procedures
Fully asleep procedures, or general anesthesia, make the patient completely unconscious. This is often used for complex or long surgeries. It’s important for the patient’s comfort and to keep them from moving.
Sleep-Awake-Sleep Technique
The sleep-awake-sleep technique starts and ends with general anesthesia. But the patient is awake during the most important part of the surgery. This method is great for surgeries near critical brain areas. It lets doctors monitor brain functions in real-time.
Fully Awake Procedures
Fully awake procedures, or awake craniotomies, require the patient to be awake and responsive. This is good for surgeries near areas that control speech and motor skills. It’s a way to avoid harming these important functions.
Specialized Equipment Used
Special equipment like intraoperative MRI and neuronavigation systems are used in awake brain surgeries. They help make the surgery more precise and safe.
Type of Surgery | Level of Consciousness | Special Considerations |
Fully Asleep | Unconscious | Complex or lengthy surgeries |
Sleep-Awake-Sleep | Partially Conscious | Critical brain areas |
Fully Awake | Fully Conscious | Vital functions like speech and motor skills |
Technological Advancements in Neurosurgery
Neurosurgery has seen big changes thanks to new tech. Now, treatments for brain problems are more precise and effective. These advances have greatly improved how well surgeries go and the care patients receive.
Intraoperative MRI and Imaging
Intraoperative MRI lets surgeons see the brain in real-time during surgery. This helps them remove tumors more accurately and safely. It’s been a game-changer for surgeries on brain tumors and epilepsy.
Neuronavigation Systems
Neuronavigation systems use 3D brain images to guide surgeons. They make surgeries more precise and reduce damage to the brain. This is key for complex procedures.
Fluorescence-Guided Surgery
Fluorescence-guided surgery uses special dyes to light up tumors. This makes it easier for surgeons to see what’s normal and what’s not. It helps remove tumors more completely and lowers the chance of them coming back.
Future Directions in Brain Surgery Technology
The future of neurosurgery looks bright with new imaging, robotics, and AI. These technologies promise even more precise and less invasive surgeries. They’re set to change the game in brain surgery.
Technology | Description | Benefits |
Intraoperative MRI | Real-time imaging during surgery | Improved accuracy, reduced risk of complications |
Neuronavigation Systems | 3D imaging for surgical guidance | Enhanced precision, minimized damage to brain tissue |
Fluorescence-Guided Surgery | Use of fluorescent dyes to highlight tumors | Better differentiation between tumor and normal tissue, improved tumor removal |
As neurosurgical tech keeps getting better, we can expect even better results for patients. It will also open doors to treating conditions that were once thought impossible to operate on.
Risks and Benefits of Awake Brain Surgery
Awake brain surgery is a complex procedure that necessitates the patient’s consciousness.rgeons to operate on the brain while the patient is awake. This is important for certain brain surgeries.
Improved Surgical Precision and Outcomes
One big advantage of awake brain surgery is improved surgical precision. Surgeons can better identify and protect important brain areas. This includes areas for speech, motor functions, and thinking.
This precision can lead to better results and fewer complications after surgery.
Potential Complications and Risks
Awake brain surgery also has risks. These include bleeding, brain swelling, infection, brain damage, or even death. The surgery’s complexity and the need for patient cooperation add to the challenges.
Psychological Impact and Considerations
The psychological effects of awake brain surgery are significant. Patients may feel a lot of anxiety or stress from being awake during surgery. It’s important to manage this anxiety well.
Managing Anxiety During the Procedure
To manage anxiety, preoperative counseling and intraoperative support are key. Sometimes, anxiolytic medications are used. Preparing and supporting patients well can greatly reduce their anxiety.
Understanding the benefits and risks of awake brain surgery helps patients and families make better decisions. Success depends on careful planning, precise surgery, and strong support for the patient.
Awake brain surgery is a complex procedure that necessitates the patient’s consciousness.
The journey to recovery starts right after the surgery. Patients are watched closely in the ICU to make sure they move smoothly from surgery to recovery.
Immediate Post-Operative Period
Right after surgery, patients are checked for any signs of problems. The team keeps an eye on their vital signs and manages their pain well.
Long-term Recovery Timeline
How long it takes to recover varies. It depends on the surgery and the patient’s health. Patients usually stay in the hospital for a few days. It can take weeks or months to fully recover, with feelings of tiredness, headaches, or changes in thinking.
Physical and Cognitive Rehabilitation
Rehab is key to getting back to normal. It includes physical, speech, and cognitive therapy. These programs are made just for the patient’s needs.
Returning to Normal Activities
Getting back to normal takes time. Patients should avoid heavy work for weeks after surgery. The team helps figure out when it’s okay to start doing daily things again, driving, and going back to work.
Support Resources for Patients
Having support is important for patients. This includes family, counseling, and support groups. These resources help a lot with the recovery, giving emotional and mental support.
Recovery Stage | Timeline | Key Activities |
Immediate Post-Operative | 0-3 days | Monitoring in ICU, pain management |
Short-term Recovery | Several weeks | Rehabilitation, gradual return to activities |
Long-term Recovery | Months | Continued rehabilitation, full recovery |
Awake brain surgery is a complex procedure that necessitates the patient’s consciousness.
Conclusion
Awake brain surgery is a complex procedure that necessitates the patient’s consciousness.
This allows the surgical team to monitor the patient’s brain function in real-time. They can ensure that critical areas are preserved. The decision to perform awake brain surgery depends on various factors.
These include the type and location of the brain tumor or lesion. By keeping the patient awake, surgeons can map critical brain areas. They protect speech, motor, and cognitive functions.
Ongoing advancements in neurosurgery continue to improve outcomes for patients. In conclusion, awake brain surgery is a sophisticated procedure. It offers benefits for certain neurological conditions.
By understanding the complexities and benefits of this procedure, patients can make informed decisions. As medical technology continues to evolve, the field of neurosurgery will likely see further improvements. This will lead to better patient outcomes.
Awake brain surgery is a complex procedure that necessitates the patient’s consciousness.
FAQ
Awake brain surgery is a complex procedure that necessitates the patient’s consciousness.
It’s done to remove tumors or lesions near important brain spots. These spots control speech, movement, or thinking. It aims to avoid harming these areas.
Awake brain surgery is a complex procedure that necessitates the patient’s consciousness.
The brain doesn’t feel pain, so the surgery isn’t painful. But, the patient might feel some discomfort. This is managed with local anesthesia and careful watching.
How long does awake brain surgery take?
The time needed varies based on the surgery’s complexity and the case. It can take from a few hours to several hours.
What are the risks associated with awake brain surgery?
Risks include infection, bleeding, and damage to brain areas. But, the benefits often outweigh the risks, like when tumors are near important areas.
How is the patient’s consciousness monitored during awake brain surgery?
The team watches the patient’s consciousness and brain functions closely. They check speech, movement, and thinking to avoid damage.
What is the recovery process like after awake brain surgery?
Recovery involves close monitoring in the hospital and then slowly getting back to normal. The patient might feel tired, uncomfortable, or have cognitive changes. These usually get better with time and rehab.
Are there any long-term side effects of awake brain surgery?
There’s a chance for long-term effects like cognitive changes, speech issues, or weakness. But, careful planning and execution can minimize these risks.
How has technology improved awake brain surgery?
New tech like intraoperative MRI, neuronavigation, and fluorescence-guided surgery has made the surgery safer and more precise. These tools help the team see and navigate the brain better.
Can anyone undergo awake brain surgery?
Not everyone can have awake brain surgery. It depends on the tumor or lesion’s location, the patient’s health, and their ability to stay awake during the surgery.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK572053/