Last Updated on December 2, 2025 by Bilal Hasdemir

Nearly 80,000 people in the United States get diagnosed with a primary brain tumor each year. Many of them need surgery. Brain tumor surgery is very complex and delicate. It comes with big risks and possible complications.Learn the crucial brain tumor surgery risks and seriousness. Understand the potential complications and how surgeons manage them clearly.
Thinking about surgery on the brain can be scary. The risks are high, and serious problems can happen. This worries patients and their families a lot.
Key Takeaways
- Knowing the risks of brain tumor surgery is key for patients and their families.
- The surgery’s complexity makes it serious and can lead to complications.
- Planning and evaluation before surgery help reduce risks.
- New surgical methods and technology are making outcomes better.
- Good care after surgery is important for managing problems and recovery.
Understanding Brain Tumors and the Need for Surgical Intervention

Surgery is a key part of treating brain tumors. It depends on the tumor’s type and how it behaves. We’ll look at the different brain tumors, their traits, and how surgery helps manage them.
Types of Brain Tumors and Their Characteristics
Brain tumors fall into two groups: benign and malignant. Benign tumors are not cancerous and grow slowly. Malignant tumors are cancerous and grow faster, spreading to other brain areas.
The most common tumors are meningiomas, gliomas, and pituitary tumors. Meningiomas are usually benign and come from the meninges. Gliomas start in brain cells and can be low-grade or high-grade (glioblastoma). Pituitary tumors affect hormone regulation.
When Surgery Becomes Necessary
Surgery is needed for tumors that cause symptoms like headaches or seizures. It’s also necessary when the tumor’s type is unsure. A biopsy might be needed to find out. Surgery is considered when other treatments don’t work.
Goals of Brain Tumor Surgery
The main goals of surgery are to remove the tumor, ease symptoms, and improve life quality. Sometimes, surgery is not a cure but helps other treatments work better.
Choosing to have surgery is tough. Our team offers full care and support. We aim to give patients the best results.
Types of Brain Tumor Surgical Procedures
There are many ways to treat brain tumors, from old methods to new ones. As we learn more about neurosurgery, we have more ways to help patients. This means we can make treatment plans that fit each person better.
Craniotomy: The Most Common Approach
A craniotomy is the most common way to remove brain tumors. It means taking part of the skull off to get to the brain. This lets surgeons see and take out the tumor. Thanks to better imaging and tools, craniotomies are more precise, which helps protect the brain around the tumor.
Minimally Invasive Techniques
Less invasive methods are becoming more popular for brain surgery. They use small tools or endoscopes through tiny cuts. These methods are great for tumors in hard-to-reach spots, because they’re more accurate and cause less damage.
Awake Brain Surgery: Purpose and Process
Awake brain surgery, or awake craniotomy, is done while the patient is awake. It’s used for tumors near important brain areas. This way, surgeons can watch how the brain works and keep important parts safe. Studies show awake brain surgery helps patients with tumors in key brain areas.
Awake craniotomy allows for real-time monitoring of neurological function, significantly reducing the risk of postoperative deficits.
Laser Interstitial Thermal Therapy (LITT)
Laser Interstitial Thermal Therapy (LITT) uses laser heat to kill tumor cells. It’s good for tumors deep in the brain. The laser probe is put in the tumor and heats it up to kill the cells. LITT is a good option for those who can’t have regular surgery.
| Surgical Procedure | Description | Benefits |
| Craniotomy | Temporary removal of a portion of the skull to access the brain | Direct visualization and removal of the tumor |
| Minimally Invasive Techniques | Use of endoscopes or specialized instruments through small incisions | Reduced recovery time and minimal scarring |
| Awake Brain Surgery | Surgery performed while the patient is conscious and alert | Real-time monitoring of neurological functions |
| LITT | Use of laser heat to destroy tumor cells | Minimally invasive treatment for deep-seated tumors |
What Happens During Brain Tumor Surgery
Brain tumor surgery is a complex procedure that needs a skilled team. It can be scary, but knowing what to expect helps. We aim to prepare patients for the surgery.
Anesthesia and Surgical Preparation
First, the patient gets general anesthesia to stay comfortable and pain-free. We then position the patient for the best access to the tumor. This step is key for a successful surgery.
The Surgical Process Step-by-Step
The surgery has several important steps. We start with a craniotomy, removing part of the skull to reach the brain. Next, we use advanced imaging and navigation to find the tumor.
Once found, we carefully remove the tumor. We aim to take out as much as we can without harming the brain.
Tumor Removal Techniques
There are different ways to remove tumors. We often use microsurgical techniques for precise removal. Sometimes, ultrasonic aspiration is used to break up the tumor for easier removal.
Surgical Closure and Immediate Recovery
After removing the tumor, we close the surgery site. We replace the bone flap and secure it. Then, the patient goes to the recovery room for close monitoring.
Post-operative care is vital for managing pain and watching for complications. Our team provides detailed care during this important time.
Pre-Surgical Assessment and Patient Evaluation
To reduce risks and improve results, a detailed pre-surgical evaluation is done. This includes advanced imaging and criteria for patient selection. It’s a key step to make sure patients are right for brain tumor surgery.
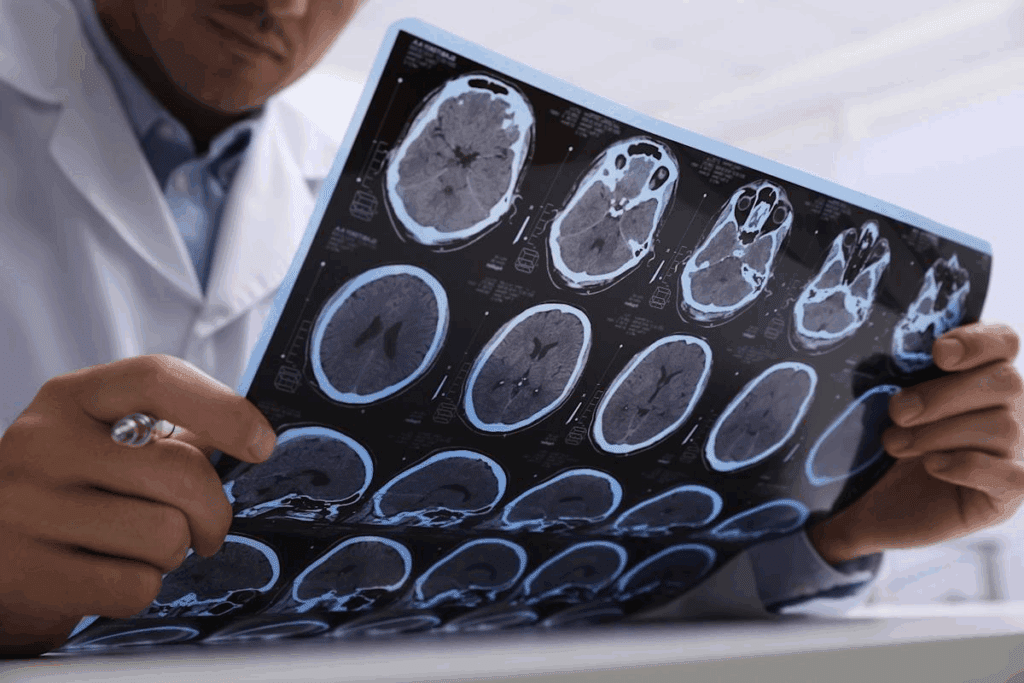
Diagnostic Imaging and Tumor Mapping
Diagnostic imaging is vital for brain tumor patients before surgery. MRI and CT scans give us detailed images of the tumor. These images help us create a precise map for surgery.
Key diagnostic imaging techniques include:
- MRI (Magnetic Resonance Imaging)
- CT (Computed Tomography) scans
- fMRI (Functional MRI) for mapping brain function
- DTI (Diffusion Tensor Imaging) for white matter tractography
Medical Clearance and Risk Assessment
Before surgery, patients get a full medical check-up. We look at their health, medications, and any other conditions that might affect surgery.
We also do a detailed risk assessment to find possible complications. This might involve talking to other doctors to make sure the patient is ready for surgery.
Patient Selection Criteria
Not every patient is a good fit for brain tumor surgery. We look at the tumor’s type, size, and location, and the patient’s health and history.
Key factors in patient selection include:
- Tumor characteristics (type, size, location)
- Patient’s overall health and medical history
- Presence of comorbid conditions
- Potential for surgical benefit versus risk
By carefully looking at these factors, we can find the best treatment for each patient. This helps ensure the best possible results.
Brain Tumor Surgery Risks: A Complete Overview
It’s key for patients to know the risks of brain tumor surgery. This surgery is complex and can affect outcomes. Knowing these risks helps patients choose the best treatment.
Immediate Surgical Complications
Complications can happen right during or after surgery. These may include:
- Bleeding or hemorrhage: Too much bleeding can happen during or after surgery. This can lead to serious issues.
- Infection: Surgery can lead to infection. This is treated with antibiotics but might need more care.
- Stroke or cerebral vasospasm: Surgery might cause a stroke or cerebral vasospasm. This can harm brain function.
“The risk of immediate complications shows the importance of choosing patients carefully and using precise surgical techniques,” says a top neurosurgeon. “Knowing these risks helps us prepare patients and their families for what’s ahead.”
Neurological Complications
Neurological issues can affect patients long-term after surgery. These may include:
- Cognitive changes: Patients might see changes in thinking, like memory loss or trouble focusing.
- Motor function impairments: Surgery near certain areas can cause weakness or paralysis.
- Speech and language deficits: Tumors near speech and language areas can cause problems after surgery.
When dealing with brain tumor surgery, we must weigh the risks against the benefits. This way, we can offer patients the best chance for a good outcome and quality of life.
Is Brain Surgery Life-Threatening? Understanding Mortality Rates
Brain tumor surgery is a serious matter that needs careful look at its death rates. This surgery is a big step for many brain issues, like tumors. It comes with risks that affect how well patients do.
Statistical Analysis of Brain Surgery Fatality Rates
Recent studies have given us important info on brain tumor surgery death rates. A big study in a top medical journal found that death rates have gone down. This is thanks to better surgery methods and care before and after surgery.
“The death rate for brain tumor surgery has dropped a lot,” says a top neurosurgeon. “This shows how far neurosurgery has come.”
Factors That Increase Mortality Risk
Many things can make brain surgery riskier. These include:
- The tumor’s location and size
- The patient’s age and health
- Other health problems
- The tumor’s type and how fast it grows
Knowing these factors helps figure out the risks of brain tumor surgery. It helps in making smart choices about treatment.
Emergency vs. Planned Procedures
Whether surgery is urgent or planned affects the risk. Emergency surgeries, done quickly, are riskier than planned ones.
Planned surgeries give time to prepare and improve the patient’s health. This lowers risks.
Chances of Dying from Brain Tumor Surgery
While brain tumor surgery death rates are a worry, it’s key to remember that risks vary. Things like the tumor type, surgery method, and care after surgery all play a part.
Understanding these helps patients and their families get a better grasp of the risks. It helps them make informed choices about their care.
Brain Tumor Surgery Side Effects and Neurological Impacts
After brain tumor surgery, many neurological side effects can occur. It’s important to understand how these can affect patients’ brain function and quality of life.
Motor Function Impairments
Brain tumor surgery can lead to motor function problems. Patients might feel weak, numb, or paralyzed in different body parts. Rehabilitation is key to help them regain strength and mobility.
Speech and Language Deficits
Speech and language issues can happen if the tumor is near language areas. Patients might struggle with speaking clearly or understanding others. Speech therapy is often needed to improve communication skills.
Cognitive Changes
Cognitive changes, like memory or concentration problems, can occur after surgery. These changes might be temporary or permanent. It’s important for patients and their families to understand these impacts for future planning.
Sensory Disturbances
Sensory issues, such as vision or hearing problems, can also arise from surgery. The severity of these issues depends on the tumor’s location and the surgery method.
| Side Effect | Description | Potential Intervention |
| Motor Function Impairments | Weakness, numbness, or paralysis | Rehabilitation therapy |
| Speech and Language Deficits | Difficulties with articulation or comprehension | Speech therapy |
| Cognitive Changes | Memory, concentration, or problem-solving issues | Cognitive rehabilitation |
| Sensory Disturbances | Vision changes, hearing loss, or altered sensations | Specific treatments based on the disturbance |
Post-Operative Complications of Brain Tumor Surgery
The time after brain tumor surgery is very important. Complications like cerebral edema, seizures, and cerebrospinal fluid leaks can happen. It’s key to manage these well to help patients get better.
Brain Swelling (Cerebral Edema)
Cerebral edema, or brain swelling, is a common issue after surgery. It happens when too much fluid builds up in the brain. This can cause the brain to press too hard on itself.
- Symptoms: Headache, nausea, vomiting, and changes in how you think or feel.
- Management: Doctors often use corticosteroids to shrink the swelling. In serious cases, they might need to drain fluid from the brain.
Seizures and Seizure Management
Seizures can happen after brain tumor surgery, mainly if the tumor was near the brain’s outer layer.
Seizure Management: Doctors usually give antiepileptic drugs (AEDs) to stop seizures. The type of AED and how long you take it depends on your situation.
Cerebrospinal Fluid Leaks
A cerebrospinal fluid (CSF) leak happens when the dura mater gets damaged. This lets CSF leak out. It can cause infections and other problems.
- Symptoms: Clear fluid coming from the surgery site, headache, and fever.
- Management: First, doctors might tell you to rest and drink lots of water. If the leak doesn’t stop, surgery might be needed.
Blood Clots and Deep Vein Thrombosis
People who have brain tumor surgery are at risk for blood clots. This includes deep vein thrombosis (DVT) and pulmonary embolism.
Prevention: To lower the risk of DVT, doctors use compression stockings and medicines that prevent blood clotting.
Brain Tumor Surgery Recovery Risks
Understanding the recovery process after brain tumor surgery is key for patients. It helps them face the risks and challenges. The journey is complex, with different stages and complications.
Immediate Post-Operative Period (First Week)
The first week is critical after surgery. Patients are watched closely for complications like swelling, infection, or bleeding. These risks are managed in a special intensive care unit.
- Close monitoring of vital signs and neurological status
- Management of pain and discomfort
- Prevention and treatment of complications such as seizures or cerebral edema
Short-Term Recovery Challenges (First Month)
In the first month, patients face many challenges. They start to feel better but may feel tired, have headaches, or experience neurological issues.
The first month after surgery is a period of adjustment. Patients need to be patient and work closely with their healthcare team to manage symptoms and address any concerns.
Long-Term Recovery Timeline and Expectations
The long-term recovery can take months to a year or more. It depends on the patient’s condition and the surgery’s extent. Patients will slowly regain strength and cognitive functions, but recovery speeds vary.
- Follow-up appointments to monitor recovery and adjust treatment plans as necessary
- Rehabilitation programs to improve cognitive and physical functions
- Ongoing support for managing late effects or complications
Risk of Tumor Recurrence
One big worry after surgery is the risk of tumor coming back. This risk depends on the tumor type, how much was removed, and genetic factors.
Monitoring for recurrence is key. It involves regular imaging and clinical checks. Early detection helps in better treatment outcomes.
Major Risks of Brain Tumor Surgery Based on Tumor Type
The risks of brain tumor surgery change a lot based on the tumor type. Each tumor is different, affecting how hard surgery is and how risky it is. Knowing these risks helps both patients and doctors make better choices about treatment.
Meningioma Surgery Risks
Meningiomas are usually not cancerous and grow from the meninges. These are the protective layers around the brain and spinal cord. Even though they’re often not cancerous, their location can make surgery tricky. Surgery for meningiomas can be complicated by their proximity to critical brain structures, such as major blood vessels and nerves. This can lead to problems with brain function after surgery.
Glioma and Glioblastoma Surgery Risks
Gliomas, including glioblastoma, start in the brain’s glial tissue. They can grow deep into the brain, making them hard to remove. Glioblastoma, being the most aggressive form, poses significant risks due to its infiltrative nature, often making complete removal difficult without damaging surrounding brain tissue. Risks include neurological impairment and the chance of the tumor coming back.
Acoustic Neuroma Surgery Risks
Acoustic neuromas are benign tumors on the nerve from the inner ear to the brain. They can affect hearing and balance. Surgery risks include damage to the facial nerve, leading to facial weakness or paralysis, and hearing loss. The delicate nature of the structures involved requires precise surgical techniques to minimize these risks.
Pituitary Tumor Surgery Risks
Pituitary tumors happen in the pituitary gland, a key gland at the brain’s base. Surgical risks include hormonal imbalances from gland damage, visual problems from optic nerve injury, and cerebrospinal fluid leaks. The complexity of pituitary surgery is heightened by the gland’s proximity to vital structures, needing careful planning and execution.
In conclusion, the type of brain tumor greatly affects the risks of surgery. It’s key to understand these risks to manage patient hopes and improve surgery results.
Risk Factors That Increase the Danger Level of Brain Tumor Surgery
It’s important to know the risks of brain tumor surgery. These risks depend on the patient and the tumor. Certain factors can make the surgery more dangerous.
Tumor Location and Proximity to Critical Brain Areas
The tumor’s location is a big factor in surgery risks. Tumors near important brain areas, like those for speech or movement, are riskier. Advanced planning and techniques are key to reducing these risks.
Tumor Size and Invasiveness
The size and how invasive a tumor is also matter. Big tumors or those that spread into the brain are harder to remove. Using new imaging and planning is important to tackle these issues.
Patient Age and Overall Health Status
Age and health also affect surgery risks. Older patients or those with health problems face higher risks. A detailed check before surgery is needed to manage these risks.
Previous Brain Treatments or Surgeries
Patients with past brain surgeries or treatments may face more risks. Changes in the brain or scar tissue can make surgery harder. Looking at the patient’s medical history is key to planning the surgery.
Knowing these risks helps neurosurgeons and patients prepare for brain tumor surgery. This can lead to better results and lower risks.
How Neurosurgeons Work to Minimize Brain Surgery Risks
Neurosurgeons use many strategies to lower risks in brain tumor surgery. They combine experience, a team effort, and the latest technology. This helps reduce problems with these complex surgeries.
Importance of Surgeon Experience and Specialization
The skills and focus of neurosurgeons are key in minimizing brain surgery risks. Those who do many brain tumor surgeries often get better results. They know different tumors and where they are. Keeping up with new techniques is also important for top care.
It’s not just about how many surgeries a surgeon has done. It’s also about handling surprises well. Expert neurosurgeons can make fast, important decisions that help patients.
Multidisciplinary Approach to Complex Cases
A multidisciplinary approach to brain tumor surgery means a team works together. This team includes neurosurgeons, oncologists, radiologists, and more. They plan a full treatment plan for each patient, from start to finish.
- Pre-surgery planning uses detailed images and tests.
- During surgery, anesthesiologists and nurses help.
- After surgery, patients get rehab and check-ups.
Technological Support and Specialized Equipment
Advanced technology and special tools are critical in minimizing brain surgery risks. Tools like intraoperative MRI and navigation systems help remove tumors safely. We keep our tools up to date for the best results.
New technology also helps us watch patients closely during and after surgery. This way, we can quickly find and fix any problems.
Modern Advances Improving the Safety of Brain Tumor Surgery
The field of brain tumor surgery has seen big changes with new technologies. These changes have led to better results and safer surgeries for patients.
Intraoperative Imaging and Navigation Systems
New imaging and navigation systems have changed brain tumor surgery. They let surgeons see the tumor and brain in real-time. This makes surgeries more precise and safe.
Intraoperative MRI and CT scans give surgeons important info during surgery. They help check how much tumor is removed and make needed changes.
Navigation systems work with pre-op images for even more accurate surgeries. Advanced neuronavigation techniques help plan and do complex surgeries. This lowers the risk of problems and improves results for patients.
Functional Mapping During Surgery
Functional mapping is a key improvement in brain tumor surgery. It helps keep important brain functions safe during surgery. Awake craniotomy and electrocorticography let surgeons map brain functions in real-time. This reduces the chance of problems after surgery.
This method lets surgeons plan their surgery based on each patient’s brain. It helps remove tumors while keeping brain functions safe.
Robotic Assistance and Precision Tools
Robotic systems and precise tools have made brain tumor surgery safer and more precise. Robotic surgical systems give clear views, precise tools, and better control. This makes it possible to do more complex surgeries with accuracy.
These tools and technologies have helped neurosurgeons do better work. They can now tackle tough cases with more confidence and better results for patients.
Brain Tumor Surgery Outcomes: Historical vs. Current
Looking at old and new results in brain tumor surgery shows big improvements. More patients are living longer, with fewer problems and better quality of life. Better techniques, imaging, and care before and after surgery have all helped.
As we keep exploring new ways in brain tumor surgery, it’s clear that modern tech and new methods are key. They will keep shaping the future of neurosurgery.
Comparing Brain Tumor Surgery Risks to Alternative Treatments
It’s important to weigh the risks of brain tumor surgery against other treatments. Knowing the risks of each option helps patients make informed choices.
Radiation Therapy Risks and Side Effects
Radiation therapy is a common treatment for brain tumors. It can cause fatigue, hair loss, and damage to brain tissue. “Radiation therapy is a double-edged sword; while it can be effective in treating brain tumors, it also poses significant risks that need to be carefully managed,” says a leading neurosurgeon.
The side effects of radiation therapy depend on the dose and type. Techniques like stereotactic radiosurgery try to protect the brain. But, risks are always present.
Chemotherapy Complications
Chemotherapy is used for brain tumors, alone or with surgery and radiation. It can cause nausea, vomiting, and increase infection risk. The blood-brain barrier limits drug delivery to tumors.
Despite these challenges, chemotherapy is a key treatment for some brain tumors. The choice of drugs and how they are given can affect risks.
Watchful Waiting Approach: When Observation is Preferred
For slow-growing or benign tumors, watchful waiting might be advised. This means regular checks without immediate treatment.
This method is good for tumors not causing symptoms. But, it requires close monitoring for any changes that might need treatment.
Combination Therapy Considerations
Many treatments combine surgery, radiation, and chemotherapy. This approach can be effective but increases risks.
Good planning and teamwork are key to reduce risks. “A tailored approach to treatment, considering the unique characteristics of the patient’s tumor and overall health, is key to achieving the best outcomes,” emphasizes a specialist.
Special Considerations for Different Patient Populations
Different patient groups face unique challenges during brain tumor surgery. The surgery’s complexity and the patient’s health play big roles in the outcome.
Pediatric Brain Tumor Surgery Risks
Pediatric patients need special care because their brains are developing. They might face long-term cognitive and developmental delays. We must think carefully about the surgery’s benefits and risks.
- Cognitive and developmental delays
- Emotional and psychological impacts
- Potential for long-term neurological deficits
To lessen these risks, pediatric neurosurgeons use advanced methods. They work with a team to give the best care.
Elderly Patients and Increased Complications
Elderly patients face more risks during and after surgery. This is because of health issues like heart disease and weaker bodies. It’s important to evaluate them well before surgery to prepare them as much as possible.
- Preoperative assessment to manage comorbidities
- Careful monitoring during surgery
- Postoperative care to prevent complications
Knowing these risks helps us care for elderly patients better during surgery.
Patients with Comorbidities
Patients with health issues like diabetes or high blood pressure need careful management. Managing these conditions well is key to avoiding complications.
We team up with patients and their doctors to get them ready for surgery. This way, we aim for the best results.
Making Informed Decisions About Brain Tumor Surgery
Understanding brain tumor surgery is key to making smart choices. It’s important to know all you can about this medical process. This way, you can make decisions that are best for your health.
Essential Questions to Ask Your Neurosurgeon
When thinking about brain tumor surgery, it’s vital to ask the right questions. Find out about the neurosurgeon’s experience with similar cases. Also, ask about the surgical approach and any risks and complications.
Don’t forget to ask about the expected outcomes and the recovery process. This will help you understand what to expect fully.
The Value of Second Opinions
Getting a second opinion can offer new insights and peace of mind. It lets you confirm your diagnosis and explore other treatment options. We suggest getting a second opinion from specialists for a fresh look at your case.
Understanding the Informed Consent Process
The informed consent process is very important in brain tumor surgery. It’s a detailed talk between you and the neurosurgeon about the surgery. This includes its risks, benefits, and other options. It’s key to understanding this to make a well-informed decision.
Balancing Quality of Life with Survival Goals
When deciding on brain tumor surgery, you must weigh your quality of life against your survival goals. Think about how the surgery might affect your daily life and well-being. We help you understand your priorities and plan a treatment that fits your needs.
Conclusion: Navigating the Serious Nature of Brain Tumor Surgery
Brain tumor surgery is a complex and serious procedure. It carries various risks and complications. We have explored the different types of brain tumors, surgical procedures, and the associated risks in this article.
Understanding these factors is key for patients to make informed decisions about their care. Navigating brain tumor surgery requires a balanced approach. This approach considers the benefits of surgery against the risks involved.
By being aware of the possible complications and working closely with a skilled neurosurgeon, patients can improve their outcomes. This can also enhance their quality of life.
As we conclude our discussion on brain tumor surgery, it’s clear that understanding the risks and benefits is essential. We hope to empower individuals to navigate this challenging journey with confidence and clarity.
FAQ
How serious is brain tumor surgery?
Brain tumor surgery is a serious and complex procedure. It carries risks like neurological deficits, infection, and even death. The severity of these risks depends on the tumor type, location, and patient health.
What are the risks associated with brain tumor surgery?
Risks include immediate surgical complications, neurological deficits, and infection. Blood clots and cerebrospinal fluid leaks are also possible. Long-term risks include cognitive changes and motor function impairments.
How dangerous is brain tumor surgery?
Brain tumor surgery is considered high-risk. This is because of the delicate nature of brain tissue and the chance of serious complications. Advances in surgical techniques and technology have improved outcomes, though.
What are the chances of dying from brain tumor surgery?
Mortality rates vary based on tumor type, patient age, and overall health. Generally, mortality rates are 1-5% for elective procedures. Emergency surgeries or complex cases may have higher rates.
What are the possible side effects of brain tumor surgery?
Side effects may include motor function impairments and speech and language deficits. Cognitive changes, sensory disturbances, and emotional changes are also possible. The severity and likelihood depend on the tumor location and individual patient factors.
How can risks be minimized during brain tumor surgery?
Risks can be minimized through careful pre-surgical planning and precise surgical techniques. Advanced technology like intraoperative imaging and functional mapping helps. A multidisciplinary approach and experienced surgeons also contribute to better outcomes.
Are there alternative treatments to brain tumor surgery?
Yes, alternative treatments include radiation therapy, chemotherapy, and watchful waiting. The choice of treatment depends on the tumor type, size, location, and patient health. Combination therapy is also considered in some cases.
How does the type of brain tumor affect surgery risks?
Different types of brain tumors have varying risks associated with surgery. This is due to their unique characteristics, locations, and growth patterns. For example, meningioma, glioma, acoustic neuroma, and pituitary tumors have different risks.
What are the special considerations for different patient populations undergoing brain tumor surgery?
Pediatric, elderly, and patients with comorbidities require special considerations. This is because of their unique physiological characteristics, health status, and increased risk of complications.
How can patients make informed decisions about brain tumor surgery?
Patients can make informed decisions by asking essential questions and seeking second opinions. Understanding the informed consent process is also important. Balancing quality of life with survival goals is key.
References
JAMA Network. Evidence-Based Medical Insight. Retrieved from https://jamanetwork.com/journals/jama/fullarticle/333878