Last Updated on December 1, 2025 by Bilal Hasdemir
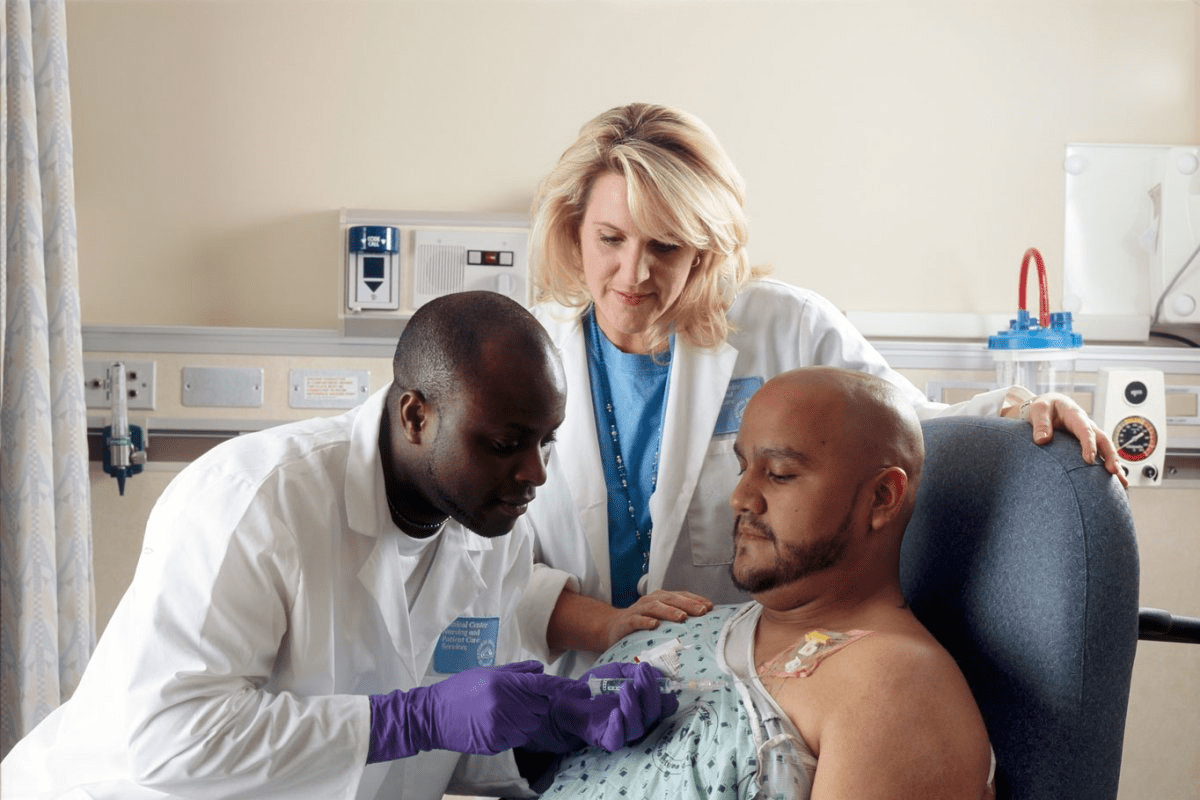
Quinn Halstead’s story shows how vital successful tumor resection is. He was diagnosed with a life-altering condition. His journey shows the challenges and complexities of brain surgery recovery brain tumor surgery success.
The success of these surgeries depends on many things. This includes the type and where the tumor is. It’s important for both patients and doctors to understand these factors.
Key Takeaways
- The success of tumor removal surgeries depends on several factors.
- The type and location of the tumor are crucial factors in determining the surgical outcome.
- Understanding these factors is key to improving surgical outcomes.
- Successful surgeries can significantly impact a patient’s quality of life.
- Advancements in medical technology are continually improving brain surgery recovery rates.
Understanding Brain Tumors and Their Classification
Brain tumors are complex and varied. They need a detailed understanding of their classification for effective treatment. The variety in brain tumors calls for a thorough approach to diagnosis and treatment. This highlights the critical role of accurate classification.
Primary vs. Secondary Brain Tumors
Brain tumors can be primary or secondary. Primary tumors start in the brain. Secondary tumors spread from other parts of the body. Knowing this difference is key for choosing the right treatment, like benign brain tumor surgery or malignant tumor removal.
Benign vs. Malignant Tumors
The type of brain tumor, whether benign or malignant, greatly affects treatment choices. Benign tumors are less aggressive and might only need surgery. Malignant tumors, on the other hand, require a more detailed treatment plan, including surgery, radiation, and chemotherapy.
WHO Grading System
The World Health Organization (WHO) grading system classifies brain tumors by their aggressiveness and cell type. This tumor classification ranges from Grade I (least aggressive) to Grade IV (most aggressive). It helps doctors predict outcomes and choose the best treatments.
When Is Brain Tumor Surgery Necessary?
Brain tumor surgery is needed based on several factors. These include the type of tumor and the symptoms it causes. Surgery is often considered when symptoms are severe or if the tumor is likely to be cancerous.
Diagnostic Criteria for Surgical Intervention
Diagnostic criteria are key in deciding if surgery is needed. They look at the tumor’s size, where it is, and what it looks like under a microscope. MRI and CT scans help doctors understand these details and make decisions about surgery.
Alternative Treatment Options
There are other treatments to consider too. These include radiation therapy and chemotherapy. The choice depends on the tumor type, the patient’s health, and other factors.
Risk-Benefit Assessment
It’s important to weigh the risks and benefits of surgery. Doctors look at the possible complications and how they might affect the brain. They also consider how surgery could improve survival and quality of life.
| Factors Influencing Surgical Decision | Description |
| Tumor Size and Location | Larger tumors or those in critical areas may require surgery. |
| Tumor Type and Histology | Malignant tumors often necessitate surgical intervention. |
| Patient’s Overall Health | Patients with good overall health are typically better candidates for surgery. |
Brain Tumor Surgery Success: Overall Statistics

It’s key for patients and doctors to know the success rates of brain tumor surgery. Studies have given us insights into survival rates and what makes surgery successful.
Survival Rate Metrics
Survival rates after surgery depend a lot on the tumor type and grade. For example, meningioma resection often has high success rates because meningiomas are usually not cancerous. On the other hand, glioblastoma surgery success rates are lower because glioblastomas are very aggressive.
- Overall 5-year survival rate for all brain tumors: 35-40%
- Meningioma 5-year survival rate: 70-90%
- Glioblastoma 5-year survival rate: 5-10%
Historical Trends in Outcomes
Over time, better surgery techniques, imaging, and treatments have led to better results. Studies show that survival rates for some brain tumors have gone up.
U.S. National Statistics
In the U.S., national data gives a broad view of brain tumor surgery results. Recent numbers show that survival rates for brain tumor patients are getting better.
- Improved surgical techniques and technology
- Increased use of adjuvant therapies like radiation and chemotherapy
- Better patient selection and preoperative planning
These stats highlight the need for ongoing research and better treatment methods for brain tumors.
Success Rates by Tumor Type
Brain tumor surgery results vary based on the tumor type. Each tumor type has its own level of complexity and challenges. This affects how well the surgery can remove the tumor.
Meningioma Resection Outcomes
Meningiomas are usually benign tumors from the meninges. These are protective membranes around the brain and spinal cord. Most meningiomas can be removed successfully, with a high rate of complete removal.
Studies show that patients with meningiomas have a good survival rate. This is true when the tumor is fully removed.
Glioblastoma Surgery Success
Glioblastoma is a more aggressive and malignant brain tumor. Despite better surgical techniques, glioblastoma patients face a tough prognosis. Success in surgery is measured by how much of the tumor is removed and the patient’s survival.
Recent studies suggest that removing as much of the tumor as possible can improve survival. But, the success rate is lower than for less aggressive tumors.
Pituitary Tumor Removal
Pituitary tumors are often benign but pose unique challenges due to their location. Advances in endoscopic techniques have boosted the success rate of removing these tumors. Many patients see significant symptom improvement or complete resolution.
Hormonal balance and preserving pituitary function are key signs of a successful surgery.
Acoustic Neuroma Outcomes
Acoustic neuromas are benign tumors affecting the vestibulocochlear nerve. Surgery aims to save hearing and facial nerve function while removing the tumor. The success rate for acoustic neuroma surgery is high, thanks to better microsurgical techniques.
The choice between surgery, observation, or radiation therapy depends on several factors. These include tumor size, patient age, and hearing status.
| Tumor Type | Surgical Success Rate | 5-Year Survival Rate |
| Meningioma | 85-95% | 70-90% |
| Glioblastoma | 50-70% | 5-10% |
| Pituitary Tumor | 80-90% | 90-97% |
| Acoustic Neuroma | 90-95% | 95-100% |
The table above shows the surgical success rates and 5-year survival rates for different brain tumors. These numbers highlight how outcomes vary by tumor type. They also stress the need for personalized treatment plans.
Complete vs. Partial Resection: Impact on Outcomes
The degree to which a brain tumor is resected greatly affects surgical success. The difference between complete and partial resection has a big impact on patient outcomes.
Gross Total Resection Benefits
Gross total resection means removing the whole tumor. This approach leads to better survival rates and quality of life. Research shows that patients with gross total resection have lower recurrence rates and live longer than those with partial resection.
Benefits of Gross Total Resection:
- Improved survival rates
- Lower recurrence rates
- Better quality of life
Partial Resection Considerations
Partial resection is sometimes needed due to tumor location or brain structure concerns. It’s important to consider the benefits and risks, like tumor regrowth.
Considerations for Partial Resection:
- Tumor location and accessibility
- Proximity to critical brain structures
- Potential for tumor regrowth
Extent of Resection and Survival
The extent of resection is linked to survival. Studies show that the more of the tumor removed, the better the survival chances.
| Extent of Resection | Survival Rate |
| Gross Total Resection | Higher |
| Partial Resection | Lower |
In conclusion, the extent of resection is key in brain tumor surgery outcomes. When possible, achieving gross total resection leads to better results.
How Tumor Location Affects Surgical Success
The place where a tumor is found greatly affects how well brain tumor surgery goes. It changes the surgery method, risks, and how well the patient recovers. The brain’s complex layout makes the tumor’s spot very important.
Accessible vs. Deep-seated Tumors
Brain tumors are either easy to get to or hard to reach. Accessible tumors are near the brain’s surface and are simpler to remove. On the other hand, deep-seated tumors are buried deep in the brain. They are harder to get to without harming other brain parts.
Eloquent Brain Areas
Tumors in eloquent brain areas are tricky to deal with. These areas handle important tasks like speaking, moving, and feeling. Surgeons face a big challenge here. They must remove the tumor carefully to avoid harming these vital spots. They might use awake craniotomy to watch the patient’s brain functions during surgery.
Brainstem and Critical Structure Proximity
Tumors near the brainstem are extra tough. The brainstem controls basic life functions like breathing and heart rate. Surgery here needs to be very precise and is riskier. The close location to important structures means doctors must plan carefully and weigh the risks and benefits.
| Tumor Location | Surgical Challenges | Potential Outcomes |
| Accessible Tumors | Easier to access, less risk of damaging surrounding tissue | Higher success rate for complete removal |
| Deep-seated Tumors | More challenging to access, higher risk of complications | Variable outcomes, partial removal possible |
| Tumors in Eloquent Brain Areas | Risk of damaging critical brain functions | Careful surgical planning needed to avoid deficits |
Knowing how tumor location affects surgery is key for doctors and patients. By understanding the challenges of each tumor’s location, doctors can plan better treatments. This helps improve how well patients do after surgery.
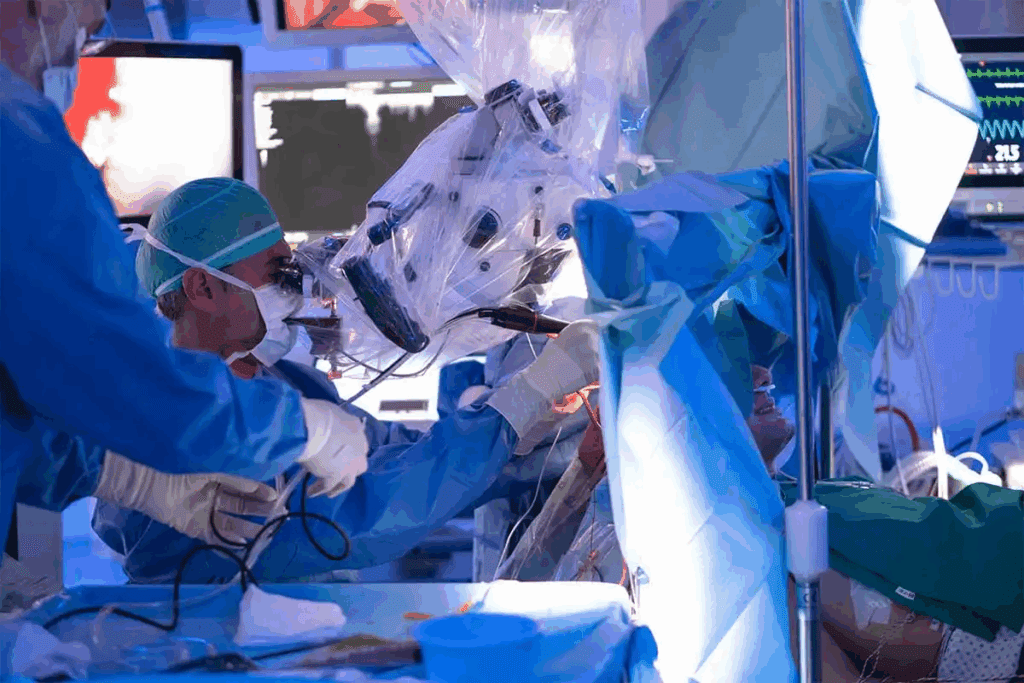
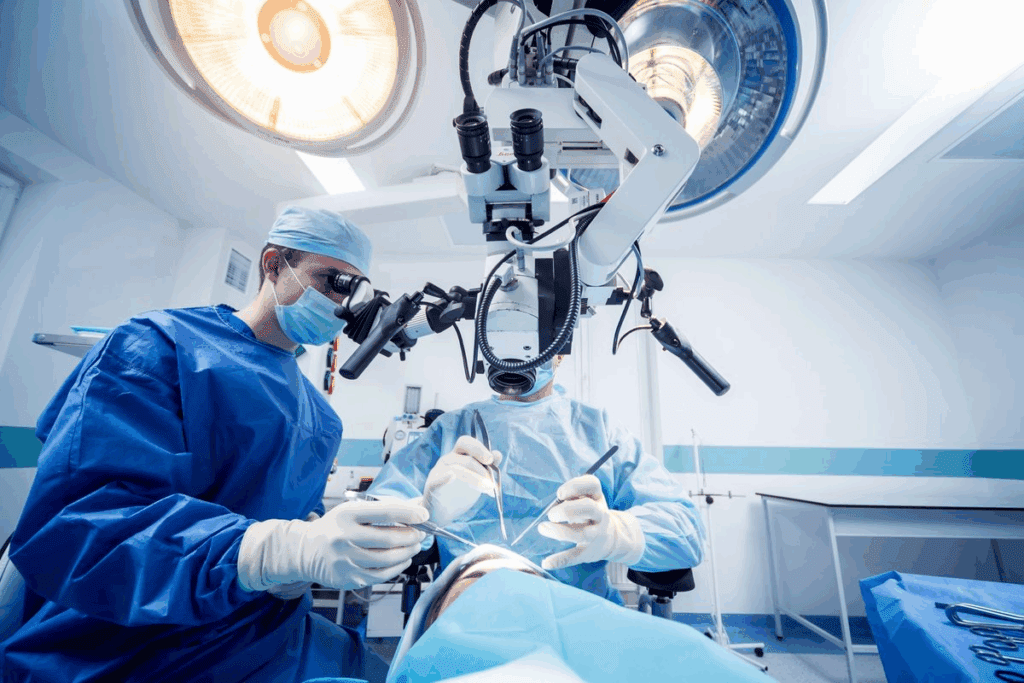
Advanced Surgical Techniques Improving Outcomes
New surgical methods have changed brain tumor treatment. These advancements make surgeries more precise and effective. This leads to better results for patients.
Awake Craniotomy Benefits
Awake craniotomy keeps the patient awake during surgery. This lets doctors check brain function as they work. It’s good because it lowers the chance of brain damage and improves results for tumors in key brain areas.
Minimally Invasive Brain Surgery
Minimally invasive surgery uses small cuts and less brain disruption. It means shorter recovery times and fewer complications. It’s great for tumors that are hard to reach or in sensitive spots.
Stereotactic Surgery Success
Stereotactic surgery uses a 3D system to find targets in the brain. It’s very accurate and used for biopsies and treatments. Its success comes from accurately targeting tumors with little harm to the brain.
Laser Interstitial Thermal Therapy
Laser interstitial thermal therapy (LITT) uses laser heat to kill tumor cells. It’s good for tumors deep inside or hard to get to. It’s a minimally invasive method with quick recovery.
These new surgical methods have greatly improved brain tumor surgery. They make surgeries more precise, reduce recovery times, and lower risks. These advancements are changing how we treat brain tumors.
Technological Innovations in Brain Tumor Surgery
Recent years have brought big changes to brain tumor surgery. These changes have made surgeries more precise and successful. They have given neurosurgeons new tools to help patients.
Intraoperative MRI and Imaging
Intraoperative MRI (iMRI) has changed brain tumor surgery a lot. It lets surgeons see the tumor in real time during surgery. This helps them know how much of the tumor they’ve removed and make changes as needed.
Benefits of Intraoperative MRI:
- Enhanced visualization of tumor boundaries
- Real-time assessment of surgical progress
- Improved accuracy in tumor resection
Fluorescence-Guided Surgery
Fluorescence-guided surgery uses special dyes to light up tumors. This makes it easier for surgeons to see and remove tumors. It’s very helpful for surgeries on gliomas and other tumors that spread.
Key advantages include:
- Increased precision in tumor removal
- Reduced risk of damaging surrounding brain tissue
- Potential for more complete resections
Neuronavigation Systems
Neuronavigation systems create a 3D map of the brain. They help surgeons plan and navigate during surgery. These systems are great for dealing with the brain’s complex layout.
| Technological Innovation | Primary Benefit | Clinical Impact |
| Intraoperative MRI | Real-time imaging | Improved tumor resection rates |
| Fluorescence-Guided Surgery | Enhanced tumor visualization | Increased precision in tumor removal |
| Neuronavigation Systems | 3D brain mapping | Better surgical planning and navigation |
In conclusion, new technologies like intraoperative MRI, fluorescence-guided surgery, and neuronavigation systems have greatly improved brain tumor surgery. They have made surgeries more precise and successful. These advancements mark a new era in neurosurgery.
Common Complications of Brain Tumor Surgery
Brain tumor surgery is often lifesaving but comes with risks. These complications can affect how well a patient does after surgery. Knowing about these risks helps manage what to expect and improve care after surgery.
Immediate Surgical Complications
Right after surgery, patients might face bleeding, infection, and cerebral edema. Bleeding can happen during or after surgery and might raise pressure inside the skull. Infection is rare but can happen and might need antibiotics or more surgery. Swelling of the brain, or cerebral edema, can also happen and might cause problems with brain function.
Management strategies for these issues include watching patients closely in intensive care. Doctors might use steroids to reduce swelling and antibiotics to fight infections.
| Complication | Description | Management |
| Bleeding | Hemorrhage during or after surgery | Close monitoring, possible surgery |
| Infection | Bacterial or other infections after surgery | Antibiotics, possible more surgery |
| Cerebral Edema | Swelling of the brain from surgery | Stroids, monitoring |
Long-term Complications
Long-term issues can really affect a patient’s life. These might include cognitive impairments, seizures, and neurological deficits. Cognitive problems can be anything from memory loss to trouble focusing. Seizures are another risk that doctors often treat with medication.
Neurological problems depend on where the tumor was and how much of it was removed. Sometimes, these issues can be helped with therapy like physical, occupational, and speech therapy.
It’s key to know about both immediate and long-term risks for patients having brain tumor surgery. This knowledge helps doctors manage what patients can expect and work to improve their recovery.
Brain Surgery Recovery Timeline
The journey to recovery after brain surgery is tough, but knowing what to expect helps. The brain surgery recovery time varies a lot. It depends on the surgery type, the patient’s health, and the tumor’s details.
Hospital Stay and Immediate Recovery
Patients usually stay in the hospital for a few days to a week after surgery. Medical staff watch them closely, managing pain and looking for complications. Right after surgery, patients need to rest and move slowly to avoid blood clots.
Short-term Recovery (First 3 Months)
In the first three months, patients might feel tired, have headaches, and notice changes in thinking. Short-term recovery is key. Patients need to rest but also start moving more slowly. Regular check-ups with doctors are important to track progress and solve any issues.
Long-term Recovery and Rehabilitation
Long-term recovery can last more than three months, sometimes up to a year or more. Rehabilitation is very important in this phase. It helps patients get back lost functions and adjust to any lasting changes. They might need physical, occupational, and speech therapy, depending on the surgery’s effects.
Return to Work and Normal Activities
When patients can go back to work and normal activities varies a lot. It depends on their job, the surgery’s extent, and their health. It’s important for patients to work with their healthcare team to find the right time to start again.
Functional Outcomes After Brain Tumor Removal
Removing a brain tumor can greatly change a patient’s life. How well a patient does after surgery varies a lot. It’s not just about removing the tumor. It’s also about how well the patient recovers and gets their skills back.
Cognitive Function Assessment
Cognitive function is key in recovery. Tests check memory, attention, and problem-solving. ” It helps patients get back lost skills and adjust to changes.
Motor Skills and Mobility
Brain tumor surgery can greatly affect motor skills and mobility. Physical therapy is key in helping patients regain strength and coordination. Recovery varies, with some getting full mobility and others needing ongoing therapy.
Speech and Language Outcomes
Tumors near speech and language areas can impact these skills. Speech therapy is often needed to help patients communicate again. Recovery varies, with some fully recovering and others facing lasting challenges.
Seizure Control Success
Seizure control is another critical outcome after surgery. Success in controlling seizures, through medication and therapy, greatly improves life quality. Effective control lets patients live more confidently and independently.
The wide range of outcomes after brain tumor surgery highlights the need for personalized care. Understanding what affects these outcomes helps healthcare providers support patients better during recovery.
Quality of Life Following Brain Tumor Surgery
The quality of life after brain tumor surgery is complex. It involves many aspects of a patient’s well-being. This includes the surgery’s success, the patient’s health, and any supportive care they receive.
Patient-Reported Outcome Measures
Patient-reported outcome measures (PROMs) are key in checking the quality of life after surgery. They give insights into symptoms, function, and overall life quality from the patient’s view.
PROMs use standardized questionnaires. These ask patients about their health. They cover physical function, emotional well-being, and social relationships.
Psychological and Emotional Impact
The surgery’s psychological and emotional effects can be big. Patients might feel anxious, depressed, or have cognitive changes.
A study found that those with psychological support did better in life quality. This was compared to those without support.
“The psychological care of patients with brain tumors is as important as the surgical treatment itself.”
A leading neurosurgeon
Social Reintegration Challenges
Getting back to normal after surgery is tough. Patients struggle to return to work and social activities.
Support from family, friends, and healthcare is key. It helps with successful reintegration.
Supportive Care Needs
Supportive care is vital after surgery. It includes rehabilitation, psychological support, and symptom management.
| Supportive Care Needs | Description | Benefits |
| Rehabilitation | Helps patients regain physical and cognitive functions. | Improves functional outcomes and quality of life. |
| Psychological Support | Addresses emotional and psychological challenges. | Enhances mental well-being and coping strategies. |
| Symptom Management | Manages symptoms such as pain, nausea, and fatigue. | Reduces symptom burden and improves comfort. |
In conclusion, the quality of life after brain tumor surgery is complex. Understanding and addressing these factors through care can greatly improve outcomes.
Adjuvant Therapies Enhancing Surgical Outcomes
Adjuvant therapies are key in improving results for brain tumor surgery patients. They work alongside surgery to target any leftover tumor cells. This helps prevent the tumor from coming back and boosts survival chances.
Adjuvant therapies are now a mainstay in treating brain tumors. By mixing surgery with other treatments, doctors can give patients a more complete care plan.
Radiation Therapy Approaches
Radiation therapy is a common adjuvant treatment to kill any leftover tumor cells after surgery. There are several ways to do radiation therapy, including:
- External Beam Radiation Therapy (EBRT)
- Stereotactic Radiosurgery (SRS)
- Brachytherapy
Each method has its own benefits. The choice depends on the tumor’s type, size, and location.
Chemotherapy Protocols
Chemotherapy is another adjuvant therapy for brain tumors. The type of chemotherapy depends on the tumor’s type and grade. Common chemotherapy agents for brain tumors include temozolomide and carmustine.
| Chemotherapy Agent | Tumor Type | Common Usage |
| Temozolomide | Glioblastoma | Concurrent with radiation therapy |
| Carmustine | High-grade gliomas | Implantable wafer during surgery |
Targeted Molecular Therapies
Targeted molecular therapies aim to target specific molecular mechanisms in tumor growth. They show promise in treating certain brain tumors, like those with specific genetic mutations.
Example: Bevacizumab is a targeted therapy that stops tumors from making their own blood supply.
Immunotherapy Advances
Immunotherapy is a promising area in brain tumor treatment. It uses the body’s immune system to fight and destroy tumor cells more effectively.
Current research is looking into different immunotherapy methods, like checkpoint inhibitors and CAR-T cell therapy.
Combining adjuvant therapies with surgery has greatly improved outcomes for brain tumor patients. Ongoing research and new advancements in these therapies are continually improving patient care and survival rates.
Recurrence Risk After Brain Tumor Surgery
Knowing the risk factors for brain tumor recurrence after surgery is key. It helps in planning treatment and improving patient outcomes.
Predicting Recurrence
Several factors can predict if a brain tumor will come back. These include the tumor’s type and grade, how much of it was removed, and the patient’s health. High-grade tumors are more likely to come back than low-grade ones. How well the tumor was removed during surgery also matters a lot.
Surveillance Protocols
Regular checks and monitoring are vital for catching recurrence early. This usually means MRI scans and doctor visits. How often you need these checks depends on the tumor type and your health.
Managing Recurrent Tumors
When a tumor comes back, treatment choices vary. They depend on the tumor’s type, where it is, and past treatments. Treatments might include repeated surgery, radiation therapy, or chemotherapy. The right treatment is chosen based on your health and condition.
Impact on Long-term Survival
Brain tumor recurrence can greatly affect survival chances. Catching it early and managing it well are key to better outcomes. A detailed follow-up care plan is important for managing risk and improving survival chances.
| Factor | Influence on Recurrence |
| Tumor Type and Grade | High-grade tumors have a higher recurrence risk |
| Extent of Resection | Complete resection reduces recurrence risk |
| Patient’s Overall Health | Poor health may increase recurrence risk |
Conclusion: The Future of Brain Tumor Treatment
The field of brain tumor treatment is changing fast. This is thanks to new surgery methods, tech advancements, and other treatments. The success of removing tumors depends on several things like the tumor’s type, where it is, and how much is removed.
New surgery techniques, like awake craniotomy and small incision brain surgery, are making a big difference. Tools like intraoperative MRI and fluorescence-guided surgery help doctors remove tumors more accurately.
The future looks bright for brain tumor treatment. Ongoing research and new ideas will likely make surgeries even better. As we go forward, combining new tech and treatments will be key. This will help improve life for those with brain tumors.
FAQ
What is the overall success rate of brain tumor removal surgeries?
The success rate of brain tumor surgeries depends on several factors. These include the tumor’s type and location, and the patient’s health. Surgery is considered successful if the tumor is removed and the patient has few complications.
How does the type of brain tumor affect the success of surgery?
The type of brain tumor greatly affects surgery success. For example, benign tumors like meningiomas have a higher success rate than malignant ones like glioblastomas. Knowing the tumor type is key to predicting outcomes.
What is the difference between gross total resection and partial resection?
Gross total resection means removing the whole tumor. Partial resection means removing only part of it. Removing the whole tumor usually leads to better outcomes and higher survival rates.
How does the location of the brain tumor impact surgical success?
The tumor’s location is very important for surgery success. Tumors in easy-to-reach areas are simpler to remove. But, tumors in hard-to-reach or important brain areas are more challenging.
What are the benefits of advanced surgical techniques like awake craniotomy and minimally invasive brain surgery?
Advanced techniques like awake craniotomy and minimally invasive surgery have many benefits. They reduce complications, damage to brain tissue, and recovery time.
What are the common complications associated with brain tumor surgery?
Common complications include infection, bleeding, stroke, and brain tissue damage. These can affect surgery success.
What is the typical recovery timeline after brain tumor surgery?
Recovery time varies based on the surgery and the patient. Patients usually spend days in the hospital and weeks or months at home recovering.
How do adjuvant therapies like radiation and chemotherapy enhance surgical outcomes?
Therapies like radiation and chemotherapy kill remaining tumor cells. This reduces recurrence risk and improves survival rates.
What is the risk of recurrence after brain tumor surgery?
Recurrence risk depends on the tumor type, grade, and how much was removed. Regular checks are key to catching recurrence early.
How do patient-reported outcome measures impact the assessment of quality of life after brain tumor surgery?
Patient reports give insights into life quality after surgery. They cover physical, emotional, and social well-being.
What is the role of supportive care in the management of brain tumor patients?
Supportive care addresses physical, emotional, and social needs. It improves life quality and helps patients deal with treatment and recovery challenges.
How do technological innovations like intraoperative MRI and neuronavigation systems improve surgical outcomes?
Innovations like intraoperative MRI and neuronavigation systems make surgery safer and more precise. They help remove tumors more accurately and reduce complications.
What are the benefits of laser interstitial thermal therapy in brain tumor treatment?
Laser interstitial thermal therapy uses heat to kill tumor cells. It’s a promising option for some brain tumors.
How does the extent of resection influence survival rates in brain tumor patients?
How much of the tumor is removed greatly affects survival rates. Removing the whole tumor usually leads to better outcomes than removing only part of it.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4252466/