Last Updated on November 26, 2025 by Bilal Hasdemir

Knowing about airway management in surgeries is key for patient safety. A breathing tube is often used to keep the airway open. This makes sure patients can breathe safely and get the anesthesia they need.
Breathing tube during surgery is an important part of many operations. Intubation means putting a tube into the airway to help with breathing and giving medicines. It’s very important in surgical procedures. It keeps patients safe and comfortable.
Key Takeaways
- Airway management is key during surgeries.
- Intubation keeps a patient’s airway open during surgery.
- Anesthesia is safely given through the breathing tube.
- Patient safety and comfort are top priorities during intubation.
- Learning about intubation can ease patient worries.
The Critical Role of Airway Management in Surgical Procedures

Effective airway management is key during surgery to keep patients safe and ensure good results. It makes sure air can flow freely between the lungs and the outside world. This is vital for getting enough oxygen and breathing well.
Why Protecting the Airway Matters During Anesthesia
Keeping the airway safe during anesthesia is very important. Anesthetics can make breathing harder, leading to poor ventilation. Intubation, or putting in a breathing tube, is often used. It helps control breathing and keeps food from getting into the lungs.
“The primary goal of airway management is to maintain a patent airway, ensuring adequate oxygenation and ventilation throughout the surgical process.” – Expert in Anesthesiology
Evolution of Airway Management Techniques
Airway management has changed a lot over time. New technology and better understanding of airways have helped. Now, we use video laryngoscopy and other tools to make intubation safer and easier.
| Technique | Description | Advantages |
| Direct Laryngoscopy | Traditional method using a laryngoscope to visualize the vocal cords. | Well-established technique, widely available. |
| Video Laryngoscopy | Uses a camera to provide a better view of the airway. | Improved visualization, easier intubation in difficult airways. |
| Fiberoptic Intubation | Flexible scope used to navigate through the airway. | Useful in patients with difficult airways, allows for awake intubation. |
New airway management methods have made surgeries safer. They lower the risks of intubation and improve patient care.
Breathing Tube During Surgery: Process and Equipment

During surgery, managing a patient’s airway is key. This is often done with a breathing tube. It’s vital for the patient’s safety and comfort.
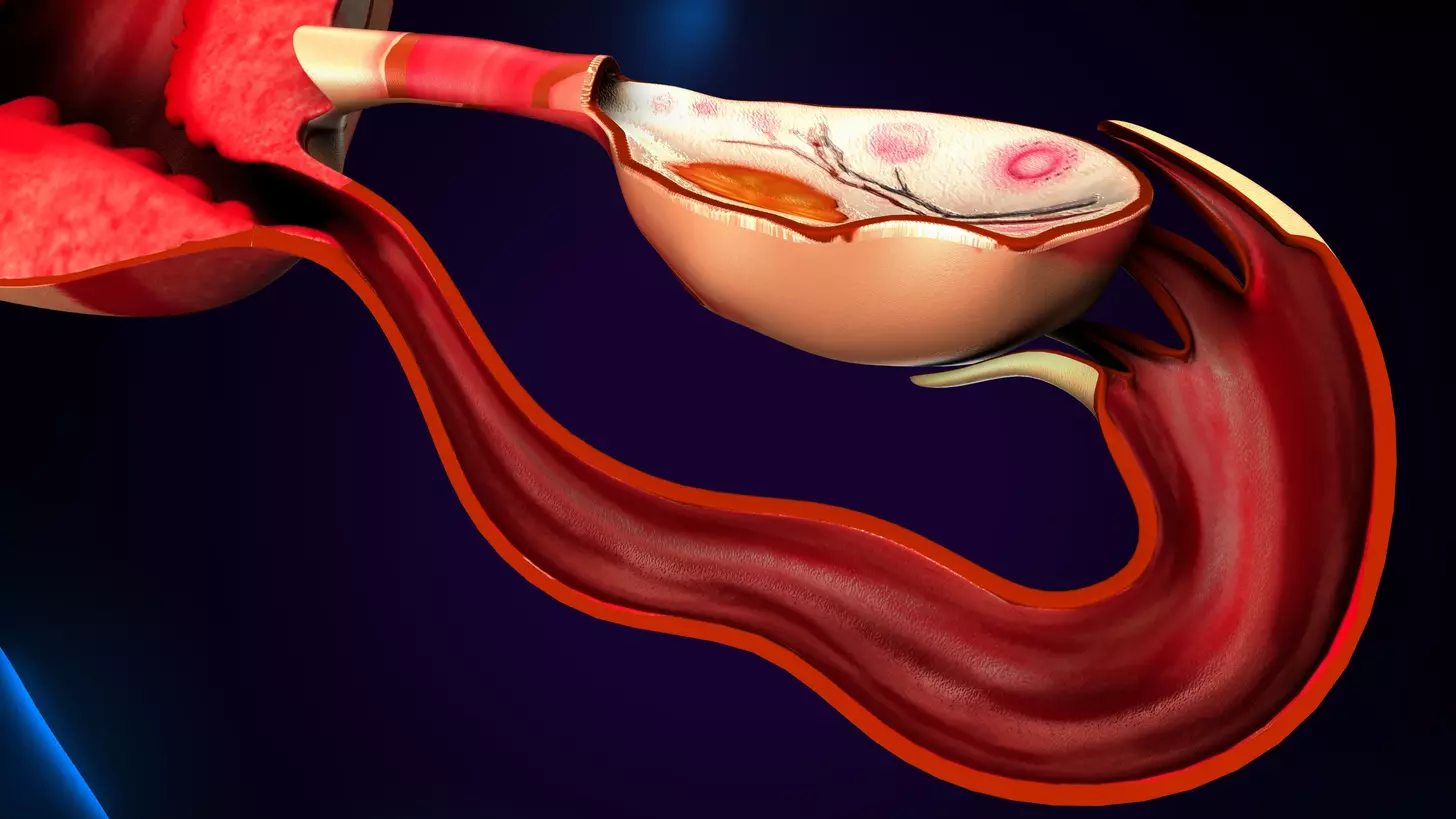
Types of Endotracheal Tubes and Their Functions
There are many types of endotracheal tubes, each for different needs. The cuffed endotracheal tube has a cuff to stop leaks and prevent aspiration. Uncuffed tubes are used in kids because of their smaller airways.
Choosing the right tube depends on the patient’s age, size, and surgery type. It’s connected to a ventilator or manual resuscitator to help with breathing.
Placement and Positioning of Breathing Tubes
Putting the tube in the right place is very important. It’s done through the mouth or nose, under direct laryngoscopy. Then, it’s checked with clinical assessment and a chest X-ray.
It’s important to place the tube correctly. Too far can cause endobronchial intubation. Too little can lead to accidental removal.
Monitoring Systems for Ensuring Proper Tube Function
Several systems are used to check if the tube is working right. Capnography checks CO2 levels, and pulse oximetry watches oxygen levels. These help spot any problems early.
| Monitoring System | Purpose |
| Capnography | Measures CO2 levels in the breath to confirm tube placement and ventilation |
| Pulse Oximetry | Monitors oxygen saturation to ensure adequate ventilation |
The Intubation Procedure Explained Step by Step
Intubation is a key step in surgery that keeps patients safe. It’s a detailed process that needs careful planning and precise actions.
Pre-Intubation Assessment and Preparation
First, doctors check the patient’s airway and health history. They also make sure the patient has enough oxygen. This is called preoxygenation.
Next, they give the patient rapid-sequence induction medications to relax them. They also apply cricoid pressure to prevent stomach contents from entering the lungs.
The Technical Process of Inserting an Endotracheal Tube
To insert the tube, doctors use a laryngoscope. This tool lets them see the vocal cords and trachea. They then guide the tube through the vocal cords into the trachea.
Confirmation of Proper Tube Placement
After the tube is in, doctors check its position. They use capnography to see if the tube is in the right place. This method checks the carbon dioxide levels in the breath.
| Step | Description | Purpose |
| Preoxygenation | Giving 100% oxygen | Increase oxygen reserves |
| Administration of rapid-sequence induction medications | Relaxation and facilitation of tube insertion | Enable safe intubation |
| Cricoid pressure application | Pressure on the cricoid cartilage | Minimize gastric aspiration risk |
| Laryngoscopy and tube insertion | Visualization and tube placement | Accurate tube placement |
| Confirmation of tube placement | Clinical assessment and capnography | Ensure correct tube position |
By following these steps, doctors can make sure intubation is safe and effective. This is very important for patient safety during surgery.
Do You Get Intubated for All Surgeries?
Not all surgeries need intubation. Intubation is when a breathing tube is put in. It’s key for safety in many operations. But, not every surgery needs this level of care.
Surgeries That Typically Require Intubation
Some surgeries often need intubation. This is because of the surgery’s nature or the patient’s health. These include:
- Major abdominal surgeries: These operations in the belly need intubation for airway management and breathing.
- Cardiothoracic surgeries: Heart and lung surgeries need precise breathing control, making intubation a must.
- Neurosurgeries: Brain surgeries require careful airway management to keep brain pressure stable.
- Prolonged surgeries: Long surgeries may need intubation to keep the airway safe for hours.
Alternative Airway Management for Minor Procedures
Not every surgery needs intubation. For smaller or less invasive surgeries, other airway management options are used. These include:
- Supraglottic airway devices: These devices sit above the glottis and offer a secure airway without endotracheal intubation.
- Local or regional anesthesia: Some surgeries can be done with local or regional anesthesia, avoiding general anesthesia and intubation.
- Conscious sedation: Patients might get sedation to relax during the surgery, keeping their breathing natural.
It’s important to know the specific needs of each surgery and patient. While intubation is common in many surgeries, other methods are better for less invasive or minor procedures.
Consciousness During Intubation: Are Patients Awake?
Intubation is a procedure to secure a patient’s airway. It raises questions about the patient’s consciousness. Whether to sedate or keep a patient awake depends on several factors. These include the surgery type, the patient’s health, and the anesthesiologist’s judgment.
Standard Protocol for Sedation Before Tube Placement
Most patients are sedated before intubation to reduce discomfort and anxiety. The standard sedation protocol uses a mix of medications. These include:
- Sedatives to relax the patient and lower anxiety
- Analgesics to lessen pain during the procedure
- Neuromuscular blocking agents to make tube insertion easier
The choice of medication and dosage varies. It depends on the patient’s health, age, and the surgery type.
Circumstances When Awake Intubation May Be Necessary
While sedation is common, awake intubation is sometimes needed. This is true when:
- The patient’s airway is hard to manage, and sedation could worsen it.
- The patient is at high risk of aspiration, and being awake keeps airway reflexes strong.
- Specific medical conditions require the patient to be awake to check neurological function during the procedure.
Awake intubation uses local anesthesia to numb the airway. Sometimes, mild sedation is used to comfort the patient without risking their airway.
Knowing about intubation and sedation can ease patients’ worries about surgery. While most patients are sedated, the choice depends on their needs and medical situation.
Duration Considerations: How Long Can a Person Be Intubated?
Knowing how long someone can be intubated is key for good patient care. The time varies based on the surgery type, patient health, and where they are being treated.
Typical Intubation Timeframes for Routine Surgeries
For most surgeries, intubation lasts a few hours to a day. This helps keep the airway safe during the surgery. It also supports the patient’s breathing until they wake up from anesthesia.
Several factors affect how long someone is intubated for routine surgeries:
- The surgery’s complexity and length
- The patient’s health and any past medical issues
- The type of anesthesia and how the patient reacts to it
Extended Intubation in Critical Care Settings
In critical care, intubation can last days or weeks. Patients in ICUs often need this because of serious illnesses or injuries. These can include respiratory failure, major trauma, or complications after surgery.
Extended intubation in these cases is managed with care. This includes:
- Checking the patient’s breathing and overall health regularly
- Changing the ventilator settings as needed
- Managing sedation to keep the patient comfortable with the tube
When and Why Doctors Transition to Tracheostomy
For patients needing ventilation for a long time, a tracheostomy might be considered. This surgery creates a direct airway through the neck. It makes ventilation more stable and comfortable.
Doctors usually suggest a tracheostomy when ventilation is expected to last more than 7-14 days. It has many benefits, such as:
- Less need for sedation because the tube is more comfortable
- Easier transition off the ventilator
- Improved mobility and communication
The choice to intubate for a long time or to have a tracheostomy depends on the patient’s needs. Healthcare providers watch patients closely to decide the best airway management.
The Patient Experience: Is Intubation Painful?
Patients often ask if intubation hurts and what it feels like. Intubation is when a breathing tube is put into the airway to help with breathing during surgery. Sedation and anesthesia help make it less uncomfortable.
Sensations During the Intubation Process
Patients are usually sedated to lessen discomfort and worry. The sedation helps them not feel pain when the tube is put in. Sedation plans can change based on the patient’s health and the surgery type. Some might feel pressure or discomfort, but real pain is rare because of the sedatives.
Common Post-Extubation Symptoms and Recovery
After surgery, when the tube is taken out, patients might feel some soreness. They might have a sore throat, hoarseness, or trouble swallowing. These symptoms usually get better in a few days. Doctors help manage these symptoms and guide the recovery.
It’s important to take care of patients after the tube is removed. They should rest their voice, drink plenty of water, and follow their doctor’s advice.
Intubation vs. Ventilation: Understanding the Difference
Intubation and ventilation are two different medical actions. Intubation means putting a breathing tube into a patient’s airway. Ventilation uses a machine to help or take over a patient’s breathing.
Intubation as an Access Procedure
Intubation is a key step to get to a patient’s airway. It’s vital during surgeries under general anesthesia. It makes sure the patient can breathe safely.
The breathing tube, or endotracheal tube, goes through the mouth or nose into the trachea. This creates a direct path for air to reach the lungs.
Doctors, like anesthesiologists or critical care physicians, do the intubation. They use tools like laryngoscopes to see the airway and place the tube correctly.
How Mechanical Ventilators Work with Breathing Tubes
After intubation, a mechanical ventilator helps with breathing. It’s connected to the tube and sends air and oxygen into the lungs. The ventilator can be adjusted to meet the patient’s needs.
It can do all the breathing work or just help when needed. Mechanical ventilators are lifesavers in many critical situations. They’re used in respiratory failure, severe trauma, or during complex surgeries.
Knowing how intubation and ventilation work helps us understand the care given to patients in these situations.
Medical Reasons for Intubating a Patient
Doctors use intubation to manage airways in many situations. It’s a key part of a patient’s care plan, tailored to their needs.
Surgical Indications for Airway Protection
Intubation is often needed to protect the airway during surgery. General anesthesia can relax muscles, including those that keep the airway open. Intubation ensures a secure airway, allowing for controlled ventilation and reducing the risk of aspiration.
- Major surgeries that require general anesthesia
- Procedures that last for an extended duration
- Surgeries involving the head, neck, or upper torso
Respiratory Failure and Ventilatory Support
In cases of respiratory failure, intubation is key for ventilatory support. This happens when the lungs can’t remove gases or provide oxygen. Intubation helps deliver oxygen and remove carbon dioxide, supporting the patient’s breathing until they can breathe on their own.
The decision to intubate for respiratory failure is based on clinical assessment, including:
- Arterial blood gas analysis
- Respiratory rate and effort
- Level of consciousness and ability to protect the airway
Emergency Situations Requiring Immediate Intubation
Emergency situations, like severe trauma, cardiac arrest, or acute airway obstruction, may need immediate intubation. Securing the airway is critical to ensure adequate oxygenation and ventilation. Rapid sequence intubation is often used in emergency settings to quickly establish a secure airway.
Some emergency conditions that may require intubation include:
- Severe facial or neck trauma
- Anaphylaxis causing airway compromise
- Cardiac arrest requiring CPR
Risks and Complications Associated with Intubation
Intubation is a lifesaving procedure but comes with risks. It can have adverse effects that healthcare providers must manage. These risks are part of the procedure’s nature.
Common Minor Complications and Their Management
Minor issues like sore throat, mild hoarseness, and swallowing discomfort can happen. These usually get better in a few days after the tube is removed. Doctors often use throat lozenges or pain meds to help.
Lip or oral trauma can also occur. It’s usually treated with local care and takes a few days to heal.
Serious but Rare Complications to Be Aware Of
Though rare, serious complications can have big effects. Vocal cord damage or paralysis is one. It might need speech therapy or surgery to fix.
Esophageal intubation is another serious issue. It happens when the tube goes into the esophagus instead of the trachea. This is a medical emergency that needs quick action.
Risk Factors That Increase Complication Rates
Some patient factors can raise the risk of complications. For example, those with difficult airway anatomy or who are obese might face higher risks.
Prolonged intubation can also lead to issues like vocal cord damage or tracheal stenosis. Doctors must consider these risks when deciding how long to intubate. They might choose a tracheostomy instead in some cases.
It’s key for both healthcare providers and patients to know about these risks. This knowledge helps doctors take steps to reduce these risks and give the best care possible.
Conclusion: The Essential Nature of Intubation in Modern Medicine
Intubation is a key part of modern medicine. It protects the airway and helps with breathing when needed. This is very important for patients during surgery and in critical care.
Airway management is a big part of medical care. Intubation is a big part of this. Knowing why patients are intubated helps doctors take better care of them.
Intubation has changed how we care for patients in surgery and intensive care. It’s a vital tool for keeping airways safe and helping with breathing.
In short, intubation is very important in modern medicine. It helps manage airways and care for patients. Its use will keep on being key for the best patient outcomes.
FAQ
Are you intubated during surgery?
Not all surgeries need intubation. But many do, like those with general anesthesia or needing airway protection.
Do you get intubated for surgery?
Yes, many surgeries need intubation. This is because it keeps the airway safe and helps control breathing.
How long can someone be intubated?
How long someone is intubated varies. It can be a few hours or even days, depending on their health and surgery type.
Are you awake when intubated?
Usually, patients are sedated before intubation. This makes them comfortable and less aware of pain.
Is intubation painful?
Intubation itself isn’t painful because of sedation and sometimes muscle relaxants. But, some discomfort might happen after.
Do they intubate you for surgery?
Yes, many surgeries require intubation. This is to keep the airway safe and help with breathing.
How long can a person be intubated?
Intubation time varies based on health and reason. In some cases, it can last weeks or longer in critical care.
Is intubation the same as ventilation?
No, intubation is putting in a breathing tube. Ventilation is using a machine to help or take over breathing.
Why do they intubate someone?
Intubation protects the airway and helps with breathing. It’s often needed during surgery or when someone can’t breathe well.
What are the risks associated with intubation?
Risks include minor issues like a sore throat. But, serious but rare problems like vocal cord damage or lung injury can also happen.
Can you be awake while intubated?
Being awake and intubated is possible in some cases. But, most patients are sedated during the process.
How long can one be intubated?
Intubation time can vary a lot. It can be just a few hours for some surgeries or much longer in critical care.
What happens if someone is intubated and sedated?
When someone is intubated and sedated, they breathe with a machine. They’re also under sedatives to reduce discomfort and anxiety.
Why is intubation necessary?
Intubation is needed to keep the airway safe and ensure good breathing. It’s also important to prevent aspiration, which is more common with general anesthesia or in serious illnesses.
References
- Park, S., et al. (2024). Associations of cholecystectomy with metabolic health: A large population-based retrospective cohort study. Scientific Reports, 14, 12345. Retrieved from