Last Updated on October 31, 2025 by
Understanding carcinoma in situ is key for those facing a cancer diagnosis. Carcinoma in situ, or CA in situ, is a stage 0 cancer. It means there are abnormal cells that haven’t spread and are in their original place. What CA in situ means in a cancer diagnosis: a very early, highly curable stage where cancer cells are non-invasive.
Getting a diagnosis of carcinoma in situ is a big moment. It shows that the abnormal cells are only in one place. This makes it a cancer type that can be treated well. Early action can lead to a full recovery, giving hope and effective treatments.
Understanding What CA in Situ Means in Cancer Terminology
The term ‘in situ’ means ‘in its place’ in Latin. In cancer terms, it means abnormal cells stay in their original spot. Knowing this is key to understanding CA in situ and how it differs from invasive cancer.
The term ‘carcinoma in situ’ (CA in situ) comes from Latin. ‘Carcinoma’ means cancer, and ‘in situ’ means in its original place. It describes a cancer that only exists in the cells where it began and hasn’t spread.
In situ carcinoma is a big deal in cancer research. It’s a stage where cancer might be curable if caught early. The term is widely used in medical texts to talk about this cancer stage.
In oncology, carcinoma in situ is a cancer that stays in the top layer of cells. It doesn’t go past the basement membrane or deeper tissues. This definition is important because it shows CA in situ is different from invasive cancer.
The medical definition of CA in situ shows it’s a good time for early treatment. Because these cells are in their original spot, treatments can be more focused. This might mean less harm compared to treatments for invasive cancers.

Knowing the biological traits of carcinoma in situ is key for early detection and treatment. Carcinoma in situ is a neoplasm that hasn’t invaded nearby tissues. It’s a critical stage in cancer development.
Dysplasia is a term for abnormal cell development. It’s a key feature of carcinoma in situ. Dysplasia can range from mild to severe, showing a gradual move towards cancer.
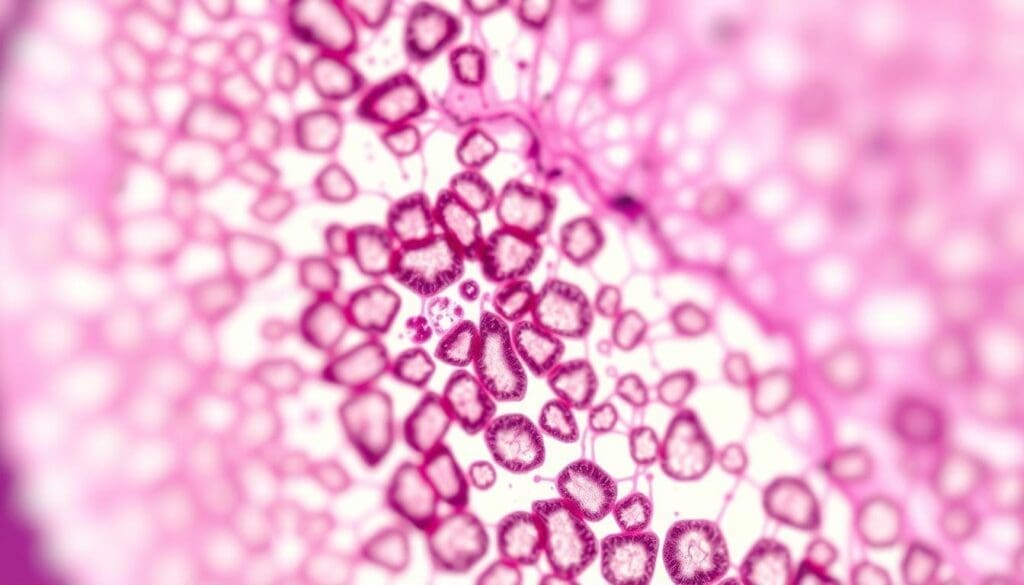
Cells with dysplasia change in size, shape, and organization. These changes can be seen under a microscope. They show the cells’ risk of becoming cancerous, but they stay in their place.
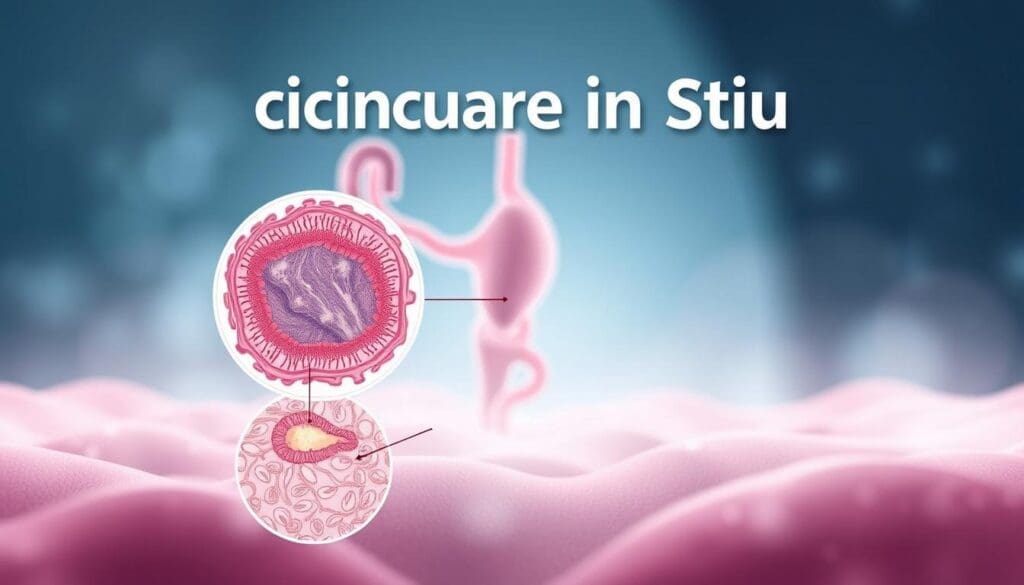
The basement membrane is a thin tissue layer between epithelial cells and the stroma. In carcinoma in situ, the abnormal cells haven’t crossed this boundary. This is different from invasive cancer, where the boundary is broken.
The basement membrane acts as a barrier. It keeps the dysplastic cells from spreading. This is why it’s important for diagnosing and staging carcinoma in situ.
Telling normal, precancerous, and cancerous cells apart is essential for diagnosis and treatment. Normal cells look and work the same. Precancerous cells, like those in dysplasia, show signs of trouble but can get worse if not treated.
Cancerous cells grow out of control and lose their normal shape. They can also spread to other areas. Carcinoma in situ shows cancerous traits but can’t spread yet.
Studying carcinoma in situ helps us understand how to diagnose and treat it better.
Stage 0 Cancer: Where CA in Situ Fits in Cancer Staging
Knowing how cancer is staged is key for understanding treatment options. It helps doctors figure out how far the cancer has spread. This is important for choosing the right treatment.
The TNM Classification System is a common way to stage cancer. It looks at three main things: the tumor’s size, nearby lymph nodes, and if the cancer has spread to other parts of the body.
The TNM system helps doctors talk about cancer in a standard way. It makes it easier to decide on the best treatment for a patient.
| TNM Component | Description | CA in Situ Designation |
| T (Tumor) | Size and extent of the primary tumor | Tis (Tumor in situ) |
| N (Node) | Involvement of nearby lymph nodes | N0 (No lymph node involvement) |
| M (Metastasis) | Presence of distant metastasis | M0 (No distant metastasis) |
Carcinoma in situ is called Tis, N0, M0 because it’s a tumor that hasn’t spread. It’s not in surrounding tissues or lymph nodes. This means it’s stage 0, or non-invasive.
Stage 0 cancer, or CA in situ, is a very early stage. It’s important for both patients and doctors to understand this. It helps in making treatment plans.
Using the TNM system helps doctors give better care. Knowing CA in situ is Tis, N0, M0 helps in planning treatments. It shows it’s a non-invasive cancer.
It’s important to know about the different types of carcinoma in situ. This knowledge helps doctors diagnose and plan treatments better. Carcinoma in situ (CA in situ) is a type of cancer that stays in one place and doesn’t spread.
Ductal carcinoma in situ (DCIS) happens in the milk ducts of the breast. It’s when abnormal cells are found but haven’t spread. Doctors often find it during mammograms, making it a non-invasive form of breast cancer.
Lobular carcinoma in situ (LCIS) affects the lobules of the breast, where milk is made. It’s not a true cancer but shows a higher risk of getting breast cancer.
Cervical carcinoma in situ means abnormal cells on the cervix’s surface haven’t spread. It’s a warning sign that can turn into invasive cervical cancer if not treated.
Squamous cell carcinoma in situ is when abnormal squamous cells stay in the top layer of skin or mucous membranes. It’s a pre-cancerous condition that can become invasive if not treated.
| Type of CA in Situ | Location | Characteristics |
| Ductal Carcinoma in Situ (DCIS) | Breast milk ducts | Abnormal cells confined to ducts, non-invasive |
| Lobular Carcinoma in Situ (LCIS) | Breast lobules | Increased risk of breast cancer, not invasive |
| Cervical Carcinoma in Situ | Cervix surface | Pre-cancerous condition, potentially invasive |
| Squamous Cell Carcinoma in Situ | Skin, mucous membranes | Abnormal squamous cells, confined to epithelial layer |
Diagnosing carcinoma in situ (CA in situ) needs advanced techniques. It’s key to find the right treatment and improve patient care.
Imaging is key in finding CA in situ. Common methods include:
Biopsy is vital for CA in situ diagnosis. It takes tissue samples for detailed checks.
There are several biopsy types, such as:
Each is chosen based on the CA in situ’s location and type.
Histopathological examination is the top method for CA in situ diagnosis. It looks at the biopsy sample under a microscope for cell changes.
“The histopathological examination provides detailed information about the cellular architecture and helps differentiate between benign, pre-cancerous, and cancerous lesions.”
– Expert Opinion
Molecular and genetic tests offer more info on CA in situ. They help find specific genetic mutations or markers.
| Test Type | Purpose | Benefits |
| Genetic Mutation Analysis | Identify specific mutations associated with CA in situ | Helps in risk assessment and treatment planning |
| Molecular Marker Testing | Detect markers associated with CA in situ | Aids in diagnosis and prognosis |
Using these methods, doctors can accurately diagnose CA in situ. This helps in creating a good treatment plan.
Risk Factors Associated with Developing Carcinoma in Situ
The growth of carcinoma in situ is shaped by genetic, environmental, and lifestyle factors. Knowing these risks is key for stopping cancer before it starts. We’ll look at how these elements lead to CA in situ.
Genetics are a big deal in carcinoma in situ. People with a family history of cancer are more at risk. Certain genes, like BRCA1 and BRCA2 for breast cancer, raise the risk a lot. Genetic tests can spot high-risk people early, helping them get help sooner.
Environmental factors also play a part in carcinoma in situ risk. Some chemicals and radiation can lead to cancer. For example, asbestos raises the risk of mesothelioma, a lung cancer. Radiation from treatments or accidents also ups cancer risk.
Lifestyle choices matter a lot for carcinoma in situ risk. Smoking, diet, and exercise level all affect cancer risk. Eating too much processed food and not enough fruits and veggies can raise risk. But, eating well and staying active can lower it. Quitting tobacco and drinking less alcohol are also key.
Knowing these risk factors helps people take steps to lower their chance of getting carcinoma in situ. Early detection and prevention can greatly improve patient outcomes.
Managing carcinoma in situ needs a deep understanding of treatment options. Decisions depend on the type and location of the carcinoma, the patient’s health, and personal choices.
Surgery is a common treatment for carcinoma in situ. It aims to remove abnormal cells and some healthy tissue. This ensures all cancerous cells are gone.
Lumpectomy and mastectomy are surgical choices. Lumpectomy removes the affected area and some healthy tissue. Mastectomy removes the whole breast.
Radiation therapy is used after surgery to kill any remaining cancer cells. It lowers the chance of cancer coming back.
External beam radiation therapy is a common type. It uses a machine outside the body to direct beams of radiation to the affected area.
For some types of carcinoma in situ, like ductal carcinoma in situ (DCIS) that is hormone-receptor-positive, hormonal therapy is recommended. Medications like tamoxifen can lower the risk of invasive cancer.
In some cases, a watchful waiting approach is used. This is when the risks of treatment are greater than the benefits. It involves regular check-ups and tests to monitor the patient’s condition.
It’s important to understand the treatments for carcinoma in situ. We work with patients to find the best treatment plan for their situation and needs.
Prognosis and Survival Rates for Patients with CA in Situ
Knowing the prognosis for carcinoma in situ is key for patients. It helps them understand their situation and make smart choices about their health. The good news is that CA in situ has a high survival rate thanks to early detection and effective treatments.
For patients with CA in situ, the outlook is bright. Almost everyone with ductal carcinoma in situ (DCIS) is alive 20 years after diagnosis. The treatment’s success for DCIS is high. Studies show that survival rates for cancer patients with CA in situ are much better than those with invasive cancer.
Several things can change a CA in situ patient’s prognosis. These include the type of CA in situ, the tumor’s size and location, and the patient’s health. Also, the treatment’s success is key. We will work with patients to understand these factors and create a treatment plan just for them.
Even with a good prognosis, there’s always a chance of recurrence. Risks include genetic mutations, the initial treatment’s success, and lifestyle choices. Regular check-ups and screenings are vital to catch any recurrence early.
By knowing the recurrence risks and what affects prognosis, patients with CA in situ can manage their treatment better. We aim to give our patients the best care and support for the best outcomes.
The Progression from CA in Situ to Invasive Cancer
Exploring the journey from carcinoma in situ (CIS) to invasive cancer is key. CIS is a stage where abnormal cells are stuck in one place. It’s important to understand how CIS can turn into invasive cancer for better treatment plans.
The time it takes for CIS to turn into invasive cancer varies. It depends on the type of CIS, genetics, and environment. Not all CIS will become invasive cancer, but most are at risk.
| Type of CIS | Average Time to Progression | Probability of Progression |
| Ductal Carcinoma in Situ (DCIS) | 5-10 years | 20-50% |
| Lobular Carcinoma in Situ (LCIS) | 10-15 years | 10-30% |
| Cervical Carcinoma in Situ | 5-15 years | 30-50% |
The move from CIS to invasive cancer is complex. It involves genetic and epigenetic changes. These changes help cancer cells spread and grow.
Molecular Alterations: Genes like TP53 and BRCA1/2 are important. So are epigenetic changes like DNA methylation and histone modification.
Spotting early signs of CIS turning into invasive cancer is vital. Look out for changes in size, pain, or unusual discharge. Regular check-ups are key to catching these signs early.
Surveillance Strategies: Imaging, biopsies, and molecular tests help track CIS. Patients with CIS should stick to follow-up plans for early detection.
To lower the risk of carcinoma in situ, it’s key to follow screening guidelines and live a healthy lifestyle. Early detection and management of CA in situ depend on these preventive steps.
Screening for CA in situ changes with age and risk. For example, women should get Pap smears for cervical cancer screening starting at 21. Mammograms for breast cancer screening are advised to start at 40 or sooner if risk is high.
Here are the recommended screening tests by age:
| Age Group | Recommended Screening |
| 21-29 years | Pap smear every 3 years |
| 40-49 years | Mammography every year or as recommended based on risk |
| 50+ years | Continue mammography and consider other screenings based on risk factors |
Those with a family history of cancer or certain genetic mutations (like BRCA1 and BRCA2 for breast cancer) are at higher risk. For them, we suggest more frequent and earlier screenings.
Lifestyle Modifications for Prevention
Changing your lifestyle can greatly reduce CA in situ risk. We suggest:
By taking these preventive steps and following screening guidelines, you can lower your risk of CA in situ. This improves your overall health.
Psychological Impact of a CA in Situ Diagnosis
A CA in situ diagnosis can be tough for patients. It makes them think about having a “pre-cancer” and what to do next. The term “carcinoma in situ” can be scary because it means it’s not yet cancer but could become invasive.
Dealing with a “pre-cancer” label can be hard. Patients might worry about their condition turning into invasive cancer. They also worry because they don’t know for sure if it will. Some feel relieved it’s not invasive, while others worry it could get worse.
The way a CA in situ diagnosis affects people can differ a lot. Things like their past with cancer, family history, and mental health play a big role. These factors help decide how they handle the news.
Choosing a treatment for CA in situ is a big deal. Patients have to pick between surgery, radiation, or just watching it. The right choice depends on the CA in situ’s type and location, the patient’s health, and what they prefer. It’s tough because they have to think about the good and bad of each option.
We help our patients make these tough choices. We give them all the info and advice they need to decide what’s best for them.
Support is key for those dealing with a CA in situ diagnosis. Having counseling, support groups, and educational resources can really help. These can offer emotional support, help understand the diagnosis and treatment, and connect with others facing the same issues.
We provide these resources to help our patients deal with the emotional side of a CA in situ diagnosis. We want them to make informed choices about their care.
Conclusion: The Importance of Early Detection and Proper Management of CA in Situ
Early detection and proper management of carcinoma in situ (CA in situ) are key to stopping cancer from spreading. Thanks to new detection methods, many cancers are caught early. This greatly improves how well patients do.
It’s important for both healthcare providers and patients to understand CA in situ. Finding CA in situ early is very important. It lets doctors act fast to stop cancer from becoming worse.
Managing CA in situ right involves many steps. These include surgery, radiation, and watching closely, among others. With the right plan, doctors can lower the chance of cancer getting worse. This helps patients live better.
We need to keep talking about CA in situ. This helps patients and doctors make smart choices about tests and treatments. By focusing on early detection and good management, we can make cancer care better for everyone.
CA in situ, or carcinoma in situ, means abnormal cells are stuck in one place. They haven’t spread to other tissues yet. It’s seen as an early cancer or a condition that might turn into cancer.
CA in situ cells stay in their original spot. Invasive cancer cells break through their original site. This lets them spread to other parts of the body.
There are several types, like ductal carcinoma in situ (DCIS) and lobular carcinoma in situ (LCIS). There’s also cervical carcinoma in situ and squamous cell carcinoma in situ. Each type has its own traits and what it means for treatment.
Doctors use many ways to find CA in situ. They might use imaging, biopsies, and tests to see if cells are abnormal. They also check the cells’ nature.
Some risks include genes, environment, and lifestyle. These can help CA in situ grow. Knowing these can help prevent and catch it early.
Doctors have several ways to treat CA in situ. They might use surgery, radiation, medicine, or watchful waiting. The choice depends on the type, where it is, and the patient.
Most people with CA in situ have a good chance of survival. But, it depends on the type, treatment, and the patient’s health. It’s also important to think about the risk of it coming back.
Yes, CA in situ can turn into invasive cancer if not treated. Knowing the risk and how long it takes is key for care.
To lower the risk, follow screening guidelines and make healthy lifestyle choices. These steps can help find it early and prevent it.
Getting a CA in situ diagnosis can be tough. It can make people worry about being “pre-cancer.” They might struggle with decisions and need support to deal with their feelings.
Finding and treating CA in situ early is key. It stops it from becoming invasive, makes treatment easier, and improves life quality and outcomes.
World Health Organization. (2025). What Does CA in Situ Mean in Cancer. Retrieved from https://www.who.int/news-room/fact-sheets/detail/cancer
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!