Last Updated on November 26, 2025 by Bilal Hasdemir
Thyroid nodules are found in up to 25% of CT scans. The presence of calcification on thyroid nodules is key in assessing cancer risk. Knowing about thyroid calcification is vital for correct diagnosis and treatment.
Liv Hospital is dedicated to top-notch care and patient-focused care. We explore what you need to know about thyroid calcifications. We’ll cover the causes, diagnosis, and treatment of calcified nodule in thyroid gland based on the latest research and clinical findings.What is a calcified nodule in thyroid gland? Get 7 key facts about thyroid calcification, cancer risks, and what to do next.
Key Takeaways
- Thyroid nodules are common and can be found in a significant portion of the population.
- The presence of calcification is a critical factor in assessing the risk associated with thyroid nodules.
- Understanding thyroid calcification is essential for proper diagnosis and treatment.
- Liv Hospital is committed to providing world-class care and patient-centered protocols.
- The latest research and clinical findings guide our understanding of thyroid calcification.
What Is Thyroid Calcification?

Calcification in the thyroid gland means calcium salts build up in the thyroid tissue. This is something to watch closely. It can happen for many reasons, from harmless changes to serious problems.
Definition and Formation Process
Thyroid calcification happens when calcium and other minerals settle in the thyroid tissue. It starts when thyroid cells change and calcium salts form. This usually happens because of long-term inflammation, cell damage, or cancer.
The reasons for thyroid calcification are complex. Chronic thyroiditis, like Hashimoto’s, can cause it because of ongoing inflammation. Also, thyroid nodules, whether they’re harmless or cancerous, can calcify.
Difference Between Normal and Abnormal Calcification
Calcification can happen in both healthy and unhealthy thyroid tissues. But, the type and where it happens can tell us if it’s okay or not.
| Characteristics | Normal/ Benign Calcification | Abnormal/ Suspicious Calcification |
| Location | Often in long-standing nodules or as part of aging process | Typically associated with thyroid nodules or tumors |
| Pattern | Coarse or peripheral calcification | Microcalcifications or speckled patterns |
| Clinical Significance | Generally benign, may not require intervention | May indicate malignancy, requires further evaluation |
Knowing the difference between normal and abnormal calcification is key. It helps doctors diagnose and treat thyroid problems correctly.
Types of Calcification in Thyroid Nodules
It’s important to know about the different types of calcification in thyroid nodules. This knowledge helps doctors diagnose and plan treatment correctly. Each type of calcification has its own meaning for health.
Coarse or Macrocalcifications
Coarse or macrocalcifications are big and usually mean the nodule is benign. They show up in nodules that have been there for a long time. This is a sign of degeneration.
Microcalcifications in Thyroid Nodules
Microcalcifications are small and point to papillary thyroid carcinoma. They often come with psammoma bodies, a sign of this cancer. Finding microcalcifications in a nodule means it needs more tests.
Peripheral (Rim) Calcifications
Peripheral or rim calcifications are at the edge of a nodule. They can be in both good and bad nodules. But, a full rim usually means it’s benign.
Speckled Calcification Patterns
Speckled calcification patterns are small dots of calcification inside a nodule. They can show up in many thyroid issues, both good and bad.
| Type of Calcification | Characteristics | Clinical Implication |
| Coarse/Macrocalcifications | Large, degenerative calcifications | Often benign |
| Microcalcifications | Tiny, associated with psammoma bodies | Highly suggestive of papillary thyroid carcinoma |
| Peripheral/Rim Calcifications | Calcification at the periphery of the nodule | Can be benign or malignant; complete rim more likely benign |
| Speckled Calcification | Scattered, punctate calcifications | Seen in various thyroid pathologies |
The type of calcification in a thyroid nodule tells a lot about it. Knowing these types helps doctors make the right diagnosis and treatment plan.
Prevalence of Calcified Nodules in Thyroid Gland
It’s important to know how common calcified nodules are in the thyroid gland. This helps us understand the risks and how to manage thyroid issues. Many thyroid gland exams find these nodules.
Epidemiological Statistics
Research shows that thyroid nodules and calcification vary a lot among different groups. Epidemiological research points out that nodules are more common where iodine is scarce. The amount of calcification in these nodules also changes a lot.
- About 30% of thyroid nodules have calcification, a study found.
- Calcification often means a higher chance of cancer.
- More people are getting thyroid calcification, studies say.
Age and Gender Distribution
Calcified thyroid nodules are not spread evenly by age and gender. Here’s what research shows:
- More thyroid nodules and calcification happen as people get older.
- Women are more likely to get thyroid nodules, including calcified ones.
- The risk of cancer in calcified nodules also goes up with age.
Geographic and Ethnic Variations
Where you live and your ethnicity affect the prevalence of calcified thyroid nodules. Different populations have different rates of calcification. This is due to genetics, environment, and diet.
| Population | Prevalence of Thyroid Calcification |
| Population A | 25% |
| Population B | 40% |
These differences highlight the need to look at demographic factors when dealing with thyroid calcification.
Key Fact #1: Calcification as a Marker for Malignancy
Calcified nodules in the thyroid gland worry doctors because they might be linked to cancer. Studies have found calcification in thyroid nodules. This has led to looking into its role as a cancer marker.
Statistical Correlation with Cancer
Research shows that microcalcifications are linked to a higher risk of thyroid cancer. Studies found that microcalcifications in nodules are a strong sign of cancer.
- Microcalcifications are small, punctate calcifications often associated with psammoma bodies in papillary thyroid carcinoma.
- The presence of microcalcifications within a thyroid nodule increases the suspicion of malignancy.
- Macrocalcifications, on the other hand, are larger and more coarse, often found in benign nodules.
Solitary Nodules with Calcification
Solitary thyroid nodules with calcification are a big worry because they might be cancerous. Doctors look at the type of calcification and other ultrasound features to assess the risk.
It’s important to tell apart benign and malignant calcifications to decide the right treatment.
Risk Assessment Based on Calcification Type
The type of calcification in a nodule greatly affects the cancer risk. Microcalcifications are seen as a high-risk sign, while macrocalcifications are linked to a lower risk.
| Calcification Type | Risk Level |
| Microcalcifications | High |
| Macrocalcifications | Low to Moderate |
Knowing the meaning of different calcification types is key for accurate risk assessment and planning treatment.
Key Fact #2: Microcalcifications and Papillary Thyroid Carcinoma
Microcalcifications in thyroid nodules are linked to a higher risk of papillary thyroid carcinoma. This link is key for early detection and treatment of thyroid cancer.
Pathophysiology of Microcalcifications
Microcalcifications are small calcium deposits in thyroid nodules. The pathophysiology is complex, involving many cellular processes. Studies show they are often found with psammoma bodies, a sign of papillary thyroid carcinoma.
Psammoma Bodies in Papillary Carcinoma
Psammoma bodies are concentric calcifications seen in papillary thyroid carcinoma. They are a key feature of this cancer and help in diagnosis. The presence of psammoma bodies is closely tied to microcalcifications.
The American Thyroid Association says finding psammoma bodies in biopsies boosts diagnosis accuracy for papillary thyroid carcinoma.
Distinguishing Features on Imaging
On ultrasound, microcalcifications show up as hyperechoic foci in thyroid nodules. These signs are vital for telling apart dangerous nodules from harmless ones. They help in assessing risk and planning treatment.
The link between microcalcifications and papillary thyroid carcinoma highlights the need for careful imaging and diagnosis. Understanding microcalcifications helps doctors better detect and treat thyroid cancer.
Key Fact #3: Benign Causes of Thyroid Calcification
Calcification in the thyroid gland can sometimes worry about cancer. But, many non-cancerous conditions also lead to this issue. Knowing these causes is key for the right diagnosis and treatment.
Colloid Nodules and Calcification
Colloid nodules are a common, non-cancerous thyroid issue. They often come from long-term thyroid problems. These nodules can turn into calcified areas, known as macrocalcifications.
Calcification in a colloid nodule is usually not a sign of cancer. But, how the nodule looks on scans is important. It helps decide if more tests are needed.
Hashimoto’s Thyroiditis
Hashimoto’s thyroiditis is an autoimmune disease that harms the thyroid. It causes inflammation and can lead to calcification. The chronic inflammation in Hashimoto’s can deposit calcium, showing up as calcification on scans.
It’s important to know Hashimoto’s can cause thyroid calcification. This helps avoid thinking it’s cancer when it’s not.
Post-inflammatory Calcification
Calcification can also happen after thyroiditis or other inflammation. It’s part of the healing process, where calcium builds up in inflamed areas. While usually harmless, it’s important to look at the whole picture and scan details to tell it apart from other causes.
In summary, thyroid calcification can have many non-cancerous reasons. These include colloid nodules, Hashimoto’s thyroiditis, and post-inflammatory calcification. Accurate diagnosis comes from a mix of doctor’s checks, scans, and sometimes lab tests to figure out what’s going on with the thyroid calcification.
Key Fact #4: Diagnostic Imaging of Calcified Thyroid Nodules
Diagnostic imaging is key in checking calcified thyroid nodules. It gives important details about their type and risks. The right imaging method is vital for accurate diagnosis and treatment.
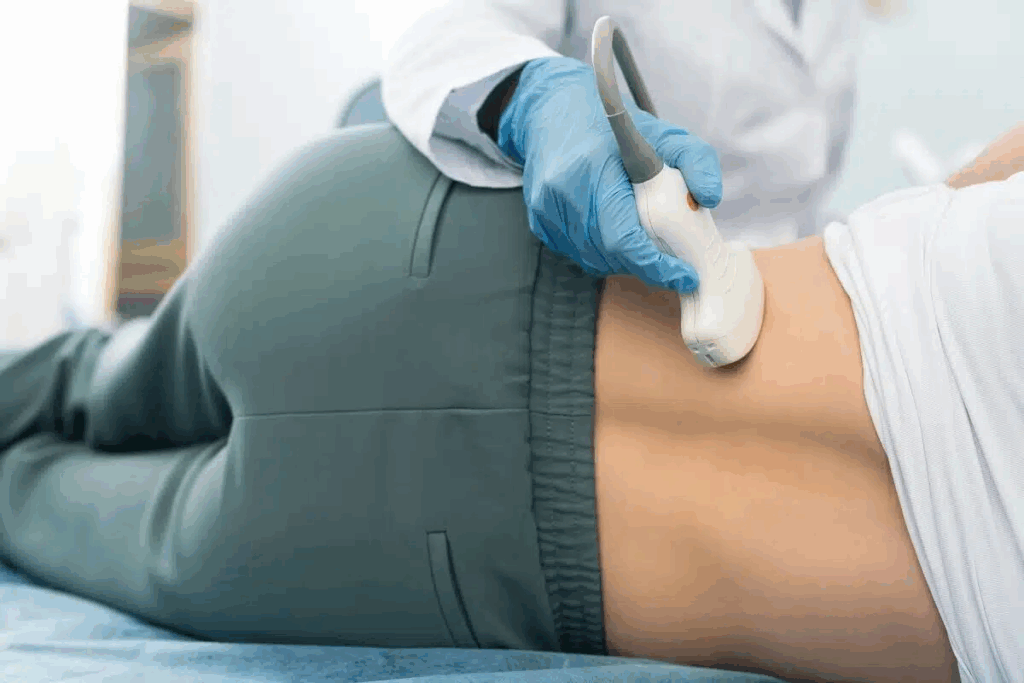
Ultrasound as the Gold Standard
Ultrasound is the top choice for looking at thyroid nodules, including calcified ones. It’s great at spotting microcalcifications, which might mean cancer. Ultrasound is also good because it shows images in real-time and doesn’t use harmful radiation.
Ultrasound can see how blood flows in nodules and spot suspicious signs like hypoechogenicity. It’s a detailed tool. Guidelines say ultrasound should be the first step in checking thyroid nodules.
Thyroid Calcification on X-ray
X-ray can sometimes find calcified thyroid nodules, but it’s not the main tool. X-ray is more for checking the throat and can spot big calcifications or thyroid cartilage calcification. But, it’s not as good at finding small calcifications or soft tissue details.
Advanced Imaging Techniques
CT and MRI are used alongside ultrasound for calcified thyroid nodules. CT scans show how big the calcification is and if it’s near other areas. MRI is better at seeing soft tissues, helping to understand nodule details and if it’s spread.
Choosing between these methods depends on the situation and what’s needed. Advanced imaging is helpful when there’s a chance of cancer spreading or big lymph nodes.
Key Fact #5: Evaluation Protocol for Calcified Nodule in Thyroid Gland
When a calcified nodule is found in the thyroid gland, a detailed evaluation is needed. This helps figure out what the nodule is and what to do next.
Fine Needle Aspiration Biopsy Indications
Fine-needle aspiration biopsy (FNAB) is key in checking calcified thyroid nodules. It’s done based on the nodule’s size, makeup, and any odd features seen on scans. Nodules that look suspicious on ultrasound, like microcalcifications or irregular shapes, usually get a FNAB.
Laboratory Assessment
After FNAB, the sample is checked in a lab. It looks for any unusual cells and uses the Bethesda System for reporting. This system helps figure out the risk and what to do next.
TIRADS Classification System
The Thyroid Imaging Reporting and Data System (TIRADS) sorts thyroid nodule risks based on ultrasound. TIRADS ranges from TR1 (safe) to TR5 (very likely cancer), helping doctors decide if FNAB or more tests are needed.
Follow-up Recommendations
What to do next with calcified thyroid nodules depends on the first check-ups. Nodules seen as safe on FNAB might need ultrasound checks later. But those looking suspicious or cancerous might need surgery. The timing and how often to check up vary based on each patient’s risk.
In summary, checking calcified thyroid nodules involves FNAB, lab tests, and TIRADS. These steps help doctors make the right choices and ensure the right care for each patient.
Key Fact #6: Treatment Approaches for Calcified Thyroid Nodules
Treatment for calcified thyroid nodules varies a lot. It can range from watching the nodule to surgery, based on several factors. The size, type, and symptoms of the nodule, along with the patient’s health, play a big role.
Observation Criteria
Many patients with calcified thyroid nodules are advised to watch them closely. This is best for small, benign nodules without symptoms. Regular ultrasounds help track the nodule’s size and changes.
Key considerations for observation include:
- Nodule size less than 1 cm
- Benign cytology on biopsy
- Absence of suspicious ultrasound features
- Patient’s preference for a conservative approach
Surgical Management Options
Surgery is needed for nodules that are likely cancerous, too big, or causing problems. The surgery type depends on the nodule’s size and the disease’s extent. It can be a simple removal of one lobe or a total thyroidectomy.
| Surgical Option | Indications | Considerations |
| Lobectomy | Solitary nodule, benign or indeterminate cytology | Preserves thyroid function, less risk of complications |
| Total Thyroidectomy | Malignant nodules, multiple nodules, significant thyroid disease | Requires lifelong thyroid hormone replacement, higher risk of complications |
“The decision to proceed with surgery should be made after careful consideration of the nodule’s characteristics, the patient’s health status, and the possible risks and benefits of the surgical procedure.”
— Endocrinology Guidelines
Non-surgical Interventions
For those not suited for surgery or who prefer not to have it, there are other options. Ethanol ablation for cystic nodules and radiofrequency ablation for solid nodules are available. These methods aim to shrink the nodule and ease symptoms.
Managing calcified thyroid nodules needs a personalized plan. It considers the nodule’s details, the patient’s health, and their wishes. Knowing the different treatment options helps doctors give the best advice for each patient.
Key Fact #7: Calcification of Thyroid Cartilage vs. Thyroid Gland
It’s important to know the difference between calcification in the thyroid cartilage and the thyroid gland. Both are part of the thyroid area but have different roles. They react differently to calcification.
Anatomical Distinctions
The thyroid gland is shaped like a butterfly and sits in the neck, around the trachea. It has two lobes joined by an isthmus. The thyroid cartilage, or Adam’s apple, is part of the larynx. It protects the vocal cords and other important structures.
Calcification in these areas means different things. Calcification in the thyroid gland might point to nodules or thyroiditis. But, calcification in the thyroid cartilage is more common with age.
Age-related Cartilage Calcification
As we get older, the thyroid cartilage can calcify more. This is a common change with age. But, it can sometimes look like other issues on scans.
“The prevalence of thyroid cartilage calcification increases with age, and it is more common in men than in women.”
Clinical Significance and Differentiation
Telling the two types of calcification apart is key for correct diagnosis and treatment. Calcification in the thyroid gland, with nodules, might need more tests to check for cancer.
| Characteristics | Thyroid Cartilage Calcification | Thyroid Gland Calcification |
| Location | Laryngeal skeleton | Thyroid gland tissue |
| Common Causes | Aging | Thyroid nodules, thyroiditis |
| Clinical Significance | Generally benign | May indicate malignancy or other thyroid pathology |
In conclusion, knowing the difference between calcification in the thyroid cartilage and gland is critical. It helps healthcare providers make the best decisions for their patients.
Recent Advances in Understanding Thyroid Calcification
The study of thyroid calcification has made big strides in recent years. This has helped us understand this condition better. It has also led to better ways to diagnose and treat it.
Molecular insights have been key in these advancements. Scientists have found specific molecules linked to calcified nodules. These could be used to predict or diagnose the condition.
Molecular Markers Associated with Calcified Nodules
Discovering markers for calcified thyroid nodules is a big leap. These markers can tell if a nodule is likely to be benign or cancerous. This could mean fewer surgeries are needed.
Recent studies have shown how certain proteins and genetic changes cause calcification. For example, the presence of psammoma bodies in some cancers is linked to microcalcifications. This helps doctors diagnose these cancers more accurately.
Emerging Diagnostic Technologies
New imaging and molecular diagnostic tools are changing how we look at thyroid calcification. Ultrasound elastography and contrast-enhanced ultrasound give more detailed views of nodules.
Also, new biopsy and molecular analysis methods are making diagnoses more accurate. These technologies promise to help tailor treatments better to each patient.
Predictive Models for Risk Stratification
Creating predictive models is a major step forward in managing thyroid calcification. These models use data from clinical, imaging, and molecular studies. They help guess the chance of a nodule being cancerous.
Risk stratification is vital for choosing the right treatment. Predictive models help doctors make better decisions. This could lead to fewer unnecessary treatments and better results for patients.
Conclusion: Managing Concerns About Thyroid Calcification
Understanding thyroid calcification is key to handling health concerns. A calcified nodule in the thyroid gland can worry people. But, it’s important to know that calcification can be both harmless and harmful.
Dealing with thyroid calcification needs a full approach. This includes getting a proper diagnosis with imaging like ultrasound. Sometimes, a fine-needle aspiration biopsy is needed. The type and look of the calcification help figure out the risk of thyroid nodules.
Knowing the facts can ease worries about thyroid calcification. A calcified thyroid gland might not always be a big deal. But, it’s important to check it out carefully. Whether thyroid calcification is serious depends on several things, like the type of calcification and other health risks.
By staying informed and talking to doctors, people can handle thyroid calcification worries. This way, they can make smart choices about their health care.
FAQ
What is thyroid calcification?
Thyroid calcification is when calcium builds up in the thyroid gland. It can happen in both harmless and cancerous conditions.
What are the different types of calcification in thyroid nodules?
There are several types of calcification in thyroid nodules. These include coarse, microcalcifications, peripheral, and speckled patterns.
Is calcification in the thyroid gland a sign of cancer?
Calcification in the thyroid gland might suggest cancer, but it’s not always the case. The type and look of the calcification can help figure out the risk.
What is the significance of microcalcifications in thyroid nodules?
Microcalcifications increase the chance of papillary thyroid carcinoma. Psammoma bodies, a type of microcalcification, are often seen in this cancer.
Can benign conditions cause thyroid calcification?
Yes, benign conditions like colloid nodules and Hashimoto’s thyroiditis can cause thyroid calcification.
How is calcified thyroid nodule diagnosed?
Diagnosing a calcified thyroid nodule involves imaging like ultrasound. Sometimes, X-ray or CT scans are used. A biopsy might also be done to check the nodule’s nature.
What is the TIRADS classification system used for?
The TIRADS system helps rate the risk of cancer in thyroid nodules. It looks at imaging characteristics, including calcification.
How are calcified thyroid nodules treated?
Treatment for calcified thyroid nodules depends on their type and cancer risk. Options include watching them, surgery, or non-surgical methods.
What is the difference between calcification of the thyroid cartilage and the thyroid gland?
Calcification of the thyroid cartilage is different from thyroid gland calcification. It’s related to aging and has its own implications.
Are there any recent advances in understanding thyroid calcification?
Yes, there have been recent discoveries. These include new markers, diagnostic tools, and predictive models for risk.
Is thyroid calcification serious?
Thyroid calcification can be serious if linked to cancer. But most cases are harmless. Proper diagnosis and care are key to understanding its impact.
References
Huttinger, R. (2023). Spigelian hernia. In StatPearls. National Library of Medicine. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK538290/





