
For those with acute myeloid leukemia, a bone marrow transplant offers hope. It’s a question we all ask: can it cure the disease? At Liv Hospital, we support patients with trust and innovation as they explore new treatments.
Acute myeloid leukemia is a severe blood cancer. It happens when the bone marrow makes bad blood cells. Studies show that bone marrow transplant can help. It can lower the chance of the disease coming back and increase survival chances. Some patients even see their 5-year survival rate jump to nearly 44%.
We look into how bone marrow transplant helps treat acute myeloid leukemia. We discuss the different transplant types and their success rates.
Key Takeaways
- Bone marrow transplant is a key treatment for AML, especially when other treatments fail.
- The process replaces bad stem cells with healthy ones, aiming to cure the disease.
- Recent studies show better survival rates with bone marrow transplant.
- There are various transplant types, each with its own success rates.
- At Liv Hospital, we offer full care for international patients looking for advanced treatments.
Understanding Acute Myeloid Leukemia (AML)
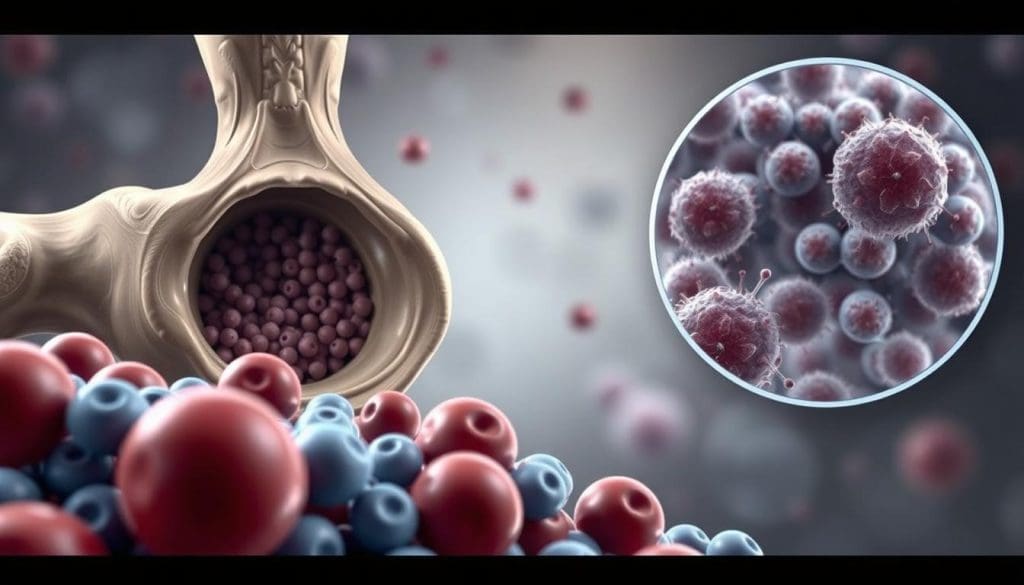
Acute Myeloid Leukemia (AML) is a blood and bone marrow cancer. It needs quick and effective treatments. AML makes abnormal white blood cells grow fast, crowding out normal cells.
What is AML?
AML is a complex disease. It makes abnormal cells grow in the bone marrow and blood. This stops normal blood cell production, causing problems like anemia and infections.
We don’t know the exact cause of AML. But we know some risk factors. These include chemicals, radiation, and genetics.
How AML Affects Bone Marrow Function
The bone marrow makes blood cells. In AML, it’s filled with cancer cells. This stops normal cell production.
- Red Blood Cells: Fewer are made, causing fatigue and weakness.
- White Blood Cells: Not enough are made, making infections more likely.
- Platelets: Fewer are made, leading to bleeding and bruising.
Common Symptoms and Diagnosis
AML symptoms include fatigue, weight loss, and infections. Easy bruising or bleeding is also common. Diagnosis involves:
- Blood tests to find abnormal cells.
- Bone marrow biopsy to look for cancer cells.
- Imaging tests to see how far the disease has spread.
Knowing about AML helps create better treatment plans. This improves patient outcomes.
The Role of Bone Marrow in Blood Cell Production
It’s key to know how bone marrow makes blood cells to understand AML’s effects. Bone marrow is the soft tissue inside some bones. It makes red blood cells, white blood cells, and platelets.
Normal Bone Marrow Function
Bone marrow’s job is to make healthy blood cells. Red blood cells carry oxygen, white blood cells fight infections, and platelets help blood clot. It does this through stem cells turning into different blood cells.
How AML Disrupts This Process
AML messes with bone marrow by making too many immature white blood cells. These cells take over, leaving less room for healthy cells. This leads to fewer normal blood cells.
AML patients often get tired, catch infections easily, and bleed a lot. This is because they don’t have enough healthy red blood cells, white blood cells, and platelets.
Impact on Patient Health
AML’s effect on bone marrow really hurts patients. They might feel tired, get sick often, and bleed easily. They also might have bone pain and discomfort.
Knowing how AML affects bone marrow is vital for treating it. Doctors can then find better ways to help patients and improve their health.
Conventional Treatments for AML
AML treatment often uses chemotherapy and other standard methods. These treatments help manage the disease. But, their success depends on the patient’s health and AML type.
Chemotherapy Approaches
Chemotherapy is key in AML treatment. It uses drugs to kill leukemia cells. Intensive chemotherapy is used to start treatment and induce remission. It can be effective but has side effects.
The choice of chemotherapy depends on the patient’s age, health, and AML subtype. High-dose chemotherapy is used for younger patients or those with certain genetic profiles.
Targeted Therapies
Targeted therapies are also important in AML treatment. They target specific molecules in leukemia cells. This can lead to fewer side effects.
Drugs like FLT3 inhibitors target genetic mutations. Midostaurin is approved for use with chemotherapy in patients with FLT3 mutations.
Why Standard Treatments May Not Be Enough
Chemotherapy and targeted therapies are crucial but may not always work. Resistance to treatment and relapse are big challenges.
In these cases, bone marrow transplantation (BMT) might be considered. BMT can replace diseased bone marrow with healthy donor marrow. It aims to cure the leukemia.
What is a Bone Marrow Transplant?
A bone marrow transplant is a complex process. It starts with preparation and ends with care after the transplant. This treatment can cure patients with Acute Myeloid Leukemia (AML).
The BMT Procedure Explained
A bone marrow transplant replaces the patient’s sick bone marrow with healthy stem cells. This can come from a donor or the patient themselves. First, the patient gets conditioning therapy. This is high-dose chemotherapy and/or radiation to kill the old bone marrow.
Conditioning Regimens: The conditioning regimen is key. It kills the bad cells and weakens the immune system. This helps the new stem cells not be rejected.
Pre-Transplant Preparation
Getting ready for a transplant involves many steps. These include:
- Checking the patient’s health to see if they can have a transplant.
- Finding and matching a donor, if needed.
- Psychological counseling for the patient and their family.
- Help with the financial costs of the transplant.
It’s important for patients to know the risks and benefits of BMT. This helps them make the best treatment choice.
Post-Transplant Care
Aftercare is vital for a successful transplant. It includes:
- Watching for signs that the new bone marrow is working.
- Dealing with possible problems like graft-versus-host disease (GVHD) and infections.
- Using medicines to stop GVHD.
- Supportive care like nutrition and counseling.
As one expert said,
“The care after a bone marrow transplant is as important as the transplant itself. It needs a team effort to meet the complex needs of these patients.”
| Phase | Key Activities | Goals |
|---|---|---|
| Pre-Transplant | Medical evaluation, donor matching, psychological counseling | Prepare patient for BMT, select suitable donor |
| Transplant | Conditioning regimen, stem cell infusion | Eradicate diseased marrow, infuse healthy stem cells |
| Post-Transplant | Monitoring, managing complications, supportive care | Ensure engraftment, prevent complications, support recovery |
Understanding the bone marrow transplant process helps patients. It lets them make informed decisions about their care.
Types of Bone Marrow Transplants for AML
For AML patients, knowing about bone marrow transplants is key. The right transplant type depends on health, donor options, and AML details.
Allogeneic Transplants
An allogeneic transplant uses stem cells from a donor. It’s great for AML because it can fight the leukemia with the donor’s immune cells.
Key benefits:
- Potential for a cure through the graft-versus-leukemia effect
- Donor cells can help eliminate remaining cancer cells
Considerations:
- Risk of graft-versus-host disease (GVHD)
- Need for a compatible donor
Autologous Transplants
An autologous transplant uses the patient’s own stem cells. It’s good for those in remission with stored stem cells.
Key benefits:
- Lower risk of GVHD
- Faster recovery of blood counts
Considerations:
- Risk of reintroducing cancer cells
- Not suitable for all patients, especially those with high-risk AML
Haploidentical Transplants
Haploidentical transplants use a half-match donor, often a family member. They’re gaining popularity for their benefits.
Key benefits:
- Almost everyone has a potential haploidentical donor among family members
- Rapid donor availability
Considerations:
- Higher risk of GVHD and other complications
- Requires advanced medical technology and expertise
Cord Blood Transplants
Cord blood transplants use stem cells from umbilical cord blood. They’re useful when a traditional donor isn’t available.
Key benefits:
- Rapid availability of cord blood units
- Lower risk of GVHD
Considerations:
- Limited cell dose, which can lead to slower engraftment
- May not be suitable for larger adult patients
Each transplant type has its pros and cons. Choosing the right one depends on the patient’s condition, donor availability, and health.
The Science Behind AML BMT Success Rates
Understanding BMT’s role in AML treatment is key. It’s a complex process with several important factors. These factors help make BMT a promising cure for AML.
How BMT Targets Leukemic Cells
BMT replaces the patient’s sick bone marrow with healthy cells. This can come from the patient (autologous transplant) or a donor (allogeneic transplant). In allogeneic transplants, the donor’s immune cells attack and kill the patient’s cancer cells.
This attack is crucial in lowering the chance of cancer coming back after the transplant. The graft-versus-leukemia effect is a major reason for allogeneic BMT’s success. It helps get rid of the cancer cells, making it less likely for the cancer to return.
The Graft-Versus-Leukemia Effect
The graft-versus-leukemia effect is when the donor’s immune cells fight the leukemia in the recipient. This effect is stronger in allogeneic transplants. It’s a big reason why BMT can be so effective in treating AML.
Research shows that this effect can greatly increase survival rates and lower the chance of cancer coming back in AML patients. Choosing the right donor and matching them well is key to getting the most benefit from this effect.
Recent Advances in Transplant Technology
There have been big improvements in BMT technology lately. These include better HLA typing, conditioning regimens, and care after the transplant. These advancements have made BMT more successful by reducing problems and boosting the graft-versus-leukemia effect.
One big step forward is using haploidentical donors. This has made it easier for patients to find a donor, especially for those from diverse backgrounds. Finding a matched donor can be hard for some patients.
Also, better care after the transplant has helped AML patients do better. This includes managing graft-versus-host disease and infections more effectively.
Patient Eligibility for Bone Marrow Transplant
To see if a patient can get a bone marrow transplant, we check their health and disease details. This check is key to see if BMT can help and if the patient can handle it.
Age Considerations
Age matters when deciding if someone can get a bone marrow transplant. Older people might face more risks because of less energy and health issues. We look at each patient’s age, health, and how well they can handle things to decide if BMT is right for them.
Younger people usually do better with tough treatments and might get BMT more often. But, every person is different, and some older folks might still be good candidates for BMT.
Health Status Requirements
A patient’s health is very important for BMT eligibility. We check their heart, lungs, liver, and kidneys to make sure they can handle the treatment and transplant.
- Cardiac function: Patients need a strong heart to get through the treatment.
- Pulmonary function: Good lung health is important to avoid breathing problems.
- Hepatic and renal function: Healthy liver and kidneys are needed for handling medicines and the transplant.
Genetic and Disease Factors
The genes of a patient’s AML and its current state are key for BMT eligibility. Those with risky genes or in remission might get BMT to lower relapse chances.
We also look at how well the patient has responded to past treatments and if there’s still disease left. These things help us figure out if BMT will likely work well.
Finding a Suitable Donor
Finding the right donor is key for a bone marrow transplant to work for AML. It starts with understanding Human Leukocyte Antigen (HLA) matching.
HLA Matching Process
HLA matching helps avoid graft-versus-host disease (GVHD) and makes the transplant successful. We test for HLA genes in both the donor and the patient. The closer the match, the lower the risk of problems.
Tests check for HLA-A, HLA-B, HLA-C, HLA-DRB1, and HLA-DQB1 genes. A perfect match means the donor and patient have the same genes at these locations.
Family Members vs. Unrelated Donors
Family members are first choices because of their genetic similarity. Siblings have a 25% chance of being a match. But, not everyone has a family donor.
When family members don’t work, we look for unrelated donors. Worldwide registries offer many potential matches. Finding a donor depends on the patient’s HLA type and ethnicity.
Donor Registries and Resources
Many registries and resources help find donors. They list donors who have had their HLA typed.
We team up with these registries to find donors and make the donation process smoother. New HLA typing methods help find better matches.
| Donor Type | Match Probability | Advantages | Disadvantages |
|---|---|---|---|
| Sibling | 25% | Higher match probability, potentially lower risk of GVHD | Limited availability, potential emotional involvement |
| Unrelated | Varies by HLA type | Large donor pool, diverse HLA types available | Lower match probability, potentially higher risk of GVHD |
Finding a donor is complex, involving HLA matching, availability, and risks. Using family and unrelated donors, along with new HLA typing, boosts transplant success for AML patients.
Success Rates and Survival Statistics
It’s important to know the success rates and survival stats for AML patients getting BMT. Recent data shows that some AML patients can have a 5-year survival rate of nearly 44% after BMT.
5-Year Survival Rates After BMT
The 5-year survival rate is a key measure of BMT’s long-term success in AML patients. This rate changes based on the patient’s age, health, and AML type.
Recent research shows that better BMT techniques and care have led to higher survival rates. For example, a study found that patients getting BMT from HLA-matched donors had a much higher 5-year survival rate than those with mismatched donors.
Factors Affecting Outcomes
Many things can affect how well BMT works for AML patients. These include:
- The patient’s age and health at transplant time
- The AML’s stage and type
- The HLA match between donor and recipient
- Any other health issues
As a leading expert says, “BMT success depends on many factors. Knowing these is crucial for better patient outcomes.”
Relapse Rates and Management
Relapse is a big worry after BMT. The relapse rate changes based on the factors mentioned earlier. Managing relapse involves:
- Keeping a close eye on patients after transplant
- Starting treatment early if relapse signs appear
- Trying new treatments and targeted therapies
“Handling relapse after BMT needs a proactive and tailored approach, using the newest AML treatments,” a recent clinical guideline says.
By knowing the success rates, survival stats, and what affects outcomes, doctors can give better advice to AML patients thinking about BMT. This can help improve their treatment chances.
Potential Complications and Side Effects
BMT can save lives but comes with challenges. Serious complications and side effects are part of the journey. Knowing these risks is key for patients and their caregivers.
Graft-Versus-Host Disease
GVHD is a big risk with allogeneic BMT. It happens when the donor’s immune cells attack the patient’s body. This can affect the skin, liver, and stomach.
Acute GVHD shows up early, causing skin issues, liver problems, or stomach troubles.
Chronic GVHD can last years. It brings more serious and widespread symptoms.
Infection Risks
People getting BMT face high infection risks. This is because their immune system is weakened. It takes time for the new immune system to kick in.
- Bacterial infections are common early on.
- Viral infections, like CMV, are a big risk.
- Fungal infections can be deadly and need special treatment.
Long-term Health Considerations
BMT survivors may deal with long-term health issues. These include:
- Organ problems, like heart or lung issues.
- Increased risk of new cancers from the treatment.
- Hormonal imbalances and fertility problems.
Here’s a quick look at complications and how to manage them:
| Complication | Management Strategy |
|---|---|
| GVHD | Immunosuppressive drugs, supportive care |
| Infections | Prophylactic antimicrobials, monitoring |
| Organ Dysfunction | Regular follow-up, organ-specific interventions |
It’s vital to know about BMT’s complications and side effects. This helps doctors take better care of patients. By understanding these risks, we can improve outcomes for AML patients getting BMT.
Advanced Treatment Protocols at Specialized Centers
Advanced treatment protocols at specialized centers offer new hope for AML patients. At Liv Hospital, we aim to provide top-notch healthcare. We follow the latest academic protocols and care pathways, meeting international standards.
Multidisciplinary Approach to AML Treatment
Our AML treatment is a team effort. Hematologists, oncologists, radiologists, and support staff work together. They create personalized treatment plans for each patient.
This team approach considers all aspects of a patient’s health. It leads to better treatment outcomes.
We use advanced diagnostic techniques to assess patients accurately. Our team includes nutritionists, psychologists, and rehabilitation specialists. They play a key role in patient care and recovery.
Implementation of Current Academic Protocols
At Liv Hospital, we lead in medical advancements. We use the latest academic protocols in BMT for AML. This includes stem cell treatments for blood disorders, a key part of BMT.
Our commitment to current academic protocols ensures our patients get the best treatments. We update our protocols with the latest research and clinical trials. This way, our patients benefit from the newest advancements in the field.
International Standards in BMT for AML
Following international standards in BMT is vital for quality care in AML. We follow guidelines from leading hematology and oncology organizations. This ensures our BMT procedures are safe and effective.
| Aspect of Care | International Standards | Our Implementation |
|---|---|---|
| Donor Selection | HLA matching, donor health assessment | Strict HLA matching, comprehensive donor evaluation |
| Transplant Procedure | Standardized protocols for conditioning and transplant | Personalized conditioning regimens, advanced transplant techniques |
| Post-Transplant Care | Monitoring for complications, graft-vs-host disease management | Comprehensive follow-up care, early intervention for complications |
By following these international standards and updating our protocols, we ensure our patients get the best care for AML through BMT.
Conclusion: Is BMT a Cure for AML?
Bone Marrow Transplant (BMT) gives many AML patients a good chance at long-term remission or even a cure. It’s not a sure thing for everyone, but it’s a strong option for those with AML.
The success of BMT in treating AML depends on several things. These include if the patient is eligible, if a donor is available, and the type of AML they have. Knowing these details helps patients make better choices about their treatment.
New advancements in transplant technology and the graft-versus-leukemia effect have made BMT more effective for AML patients. As we keep improving BMT, the hope for curing AML grows stronger.
In the end, whether BMT can cure AML varies from person to person. But with the right patient and donor match, BMT can be a powerful cure for many. It gives them a second chance at life.
What is Acute Myeloid Leukemia (AML)?
Acute myeloid leukemia (AML) is a serious blood cancer. It happens when the bone marrow makes bad blood cells.
Can bone marrow transplant cure AML leukemia?
Bone marrow transplant (BMT) is a big help for AML. It’s especially useful when other treatments don’t work. It can lead to long-term remission or even a cure.
What are the different types of bone marrow transplants available for AML?
There are many BMT types, like allogeneic, autologous, haploidentical, and cord blood transplants. Each has its own benefits and uses.
How does AML affect bone marrow function?
AML messes up the bone marrow’s job of making healthy blood cells. This leads to health problems.
What is the role of HLA matching in finding a suitable donor?
HLA matching is key to finding a good donor for BMT. It checks the donor and recipient’s HLA genes for compatibility.
What are the potential complications and side effects of BMT?
BMT can cause problems like graft-versus-host disease (GVHD), infections, and long-term health issues.
What is the graft-versus-leukemia effect?
The graft-versus-leukemia effect is when the transplanted cells fight the cancer cells. This can help get rid of the leukemia.
How do conventional treatments like chemotherapy and targeted therapies work in managing AML?
Chemotherapy and targeted therapies are key in fighting AML. Chemotherapy kills cancer cells, and targeted therapies target specific cancer molecules.
What are the factors that influence patient eligibility for BMT?
Who can get BMT depends on age, health, genetics, and the disease itself.
What are the success rates and survival statistics for BMT in AML?
BMT success and survival rates vary. They depend on the transplant type, patient health, and disease details. Some patients can live up to 5 years after BMT.
What is the significance of stem cell transplant for AML?
Stem cell transplant, or BMT, is a major treatment for AML. It offers a chance for long-term remission or cure.
Can leukemia be cured with bone marrow transplant?
BMT can cure AML in some cases. It depends on the patient’s health, donor availability, and disease specifics.
References
- Li, Y., & Zhou, F. (2023). Efficacy of bone marrow transplantation in treating acute myeloid leukemia: a systematic review and meta-analysis. American Journal of Translational Research, 15(1), 1–12.https://pmc.ncbi.nlm.nih.gov/articles/PMC9908463/
- National Marrow Donor Program (NMDP). Acute myeloid leukemia (AML) Treatment | Blood & Marrow Transplant.https://www.nmdp.org/patients/understanding-transplant/diseases-treated-by-transplant/acute-myeloid-leukemia
- American Association for Cancer Research (AACR). (2024, March 22). Outcomes After Stem Cell Transplant in Elderly Patients With Acute Myeloid Leukemia Have Improved Since 2000. https://www.aacr.org/about-the-aacr/newsroom/news-releases/outcomes-after-stem-cell-transplant-in-elderly-patients-with-acute-myeloid-leukemia-have-improved-since-2000/
- PDQ® Adult Treatment Editorial Board. (2025, May 16). Acute Myeloid Leukemia Treatment (PDQ®)–Patient Version. National Cancer Institute. https://www.cancer.gov/types/leukemia/patient/adult-aml-treatment-pdq




































