Last Updated on October 20, 2025 by
For those with acute myeloid leukemia (AML), bone marrow transplantation is a hopeful cure.
New ways to match donors and care after the transplant have made AML treatment better. This is true even for those 60 and older, who now have a higher chance of living five years after treatment.
At Liv Hospital, we focus on our patients. We use the latest technology and care methods to help them get the best results.
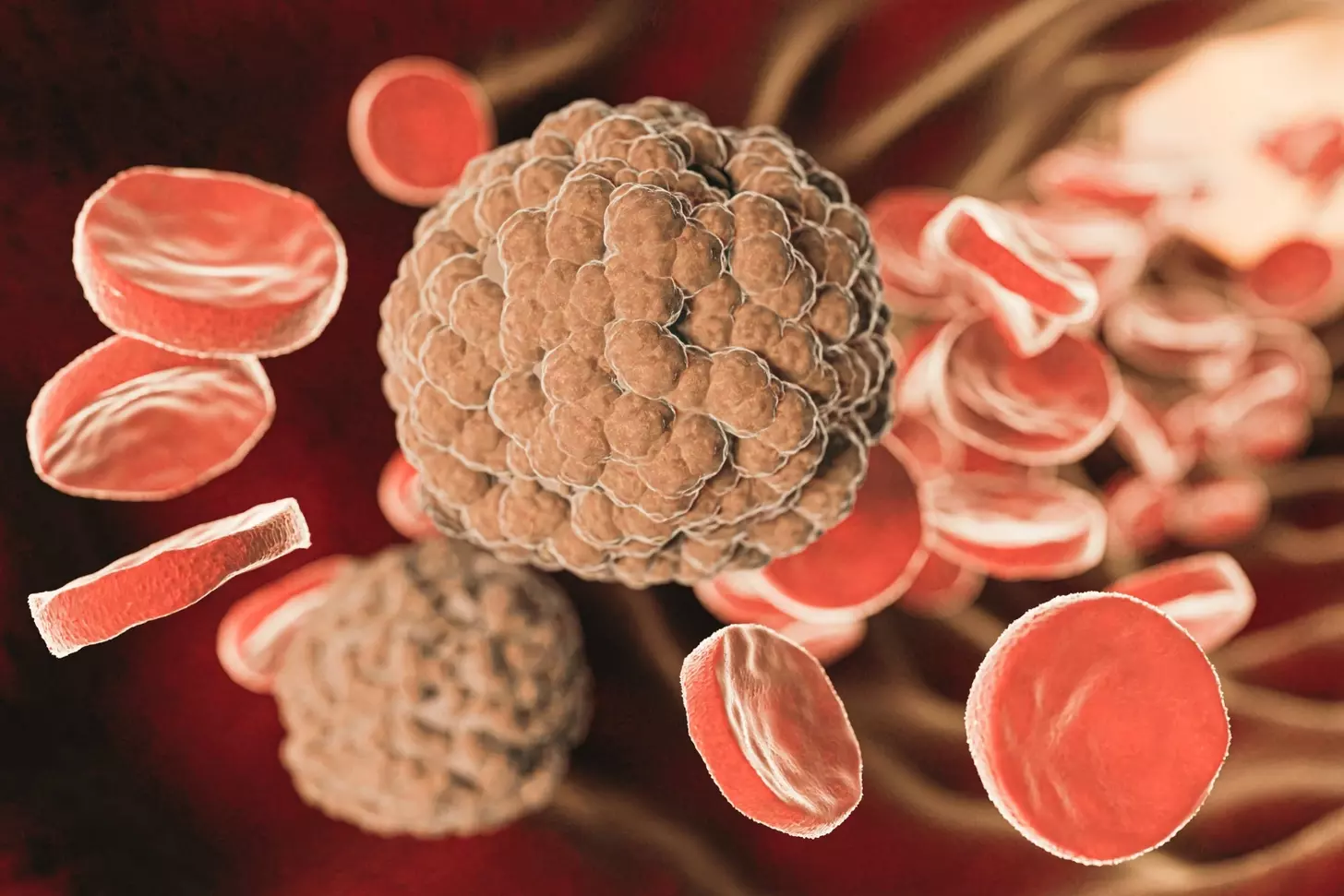
Learning about bone marrow transplant in leukemia treatment starts with knowing about leukemia. Leukemia is a cancer that affects the blood and bone marrow. It’s caused by abnormal white blood cells. Acute Myeloid Leukemia (AML) is a fast-growing type that needs quick treatment.
Leukemia is a term for many blood cancers. It happens when the bone marrow makes bad white blood cells. This makes it hard for the body to fight off infections. Understanding leukemia means knowing its different types and how to treat them.
AML grows fast and fills the bone marrow and blood with bad cells. It messes up blood cell production, causing anemia, infections, and bleeding. Symptoms of AML can appear quickly, like fatigue, weight loss, and infections.
AML treatment often includes chemotherapy, targeted therapy, and sometimes bone marrow transplantation. Chemotherapy kills leukemia cells. Targeted therapy attacks specific molecules in leukemia cells. Bone marrow transplantation can cure by replacing bad marrow with healthy stem cells.
It’s important for patients to understand leukemia and AML. Knowing their condition and treatment options helps them make better choices in their care.
Bone marrow transplantation is a complex process. It replaces damaged bone marrow with healthy stem cells to fight leukemia. This method is key for those with Acute Myeloid Leukemia (AML).
Healthy bone marrow makes blood cells like red and white blood cells, and platelets. It’s found in bones like the hips and thighbones. Stem cells in the bone marrow grow into different blood cells, each with its own job. For example, red blood cells carry oxygen, and white blood cells fight infections.
Leukemia is a cancer that harms the blood and bone marrow. It makes the bone marrow produce bad white blood cells. Acute Myeloid Leukemia (AML) is a fast-growing leukemia that needs quick treatment. Leukemia cells in the bone marrow can lower healthy blood cell production, causing anemia, infections, and bleeding.
Bone marrow transplantation uses chemotherapy and/or radiation to kill the bad bone marrow. Then, healthy stem cells are given. These stem cells can be from a donor or the patient. The aim is to replace the sick bone marrow with healthy one, so the body can make normal blood cells. A study showed that the success of bone marrow transplantation in AML patients depends on disease risk and how well the disease is controlled, as seen in a study on long-term outcomes in AML patients.
Knowing how bone marrow transplantation works helps patients and doctors understand this treatment for leukemia better.
It’s important to know about the different bone marrow transplant types for AML treatment. We’ll look at the main options, their benefits, and possible downsides.
Allogeneic hematopoietic stem cell transplantation uses stem cells from a donor. It’s a common choice for AML patients. This method can cure the disease by replacing damaged bone marrow with healthy cells from a donor.
The graft-versus-leukemia effect is key here. The donor’s immune cells fight any leukemia cells left behind.
For more info on other stem cell transplant options, check out Liv Hospital’s guide on autologous vs. allogeneic.
Autologous stem cell transplants use the patient’s own stem cells. First, the patient’s stem cells are harvested. Then, they get high-dose chemotherapy, and the stem cells are reinfused to help the bone marrow heal.
Autologous transplants are easier on the patient than allogeneic ones. But, they have a higher risk of relapse because they might reinfuse cancer cells.
Both transplant types have their own strengths and weaknesses. Allogeneic transplants can cure and have a graft-versus-leukemia effect. But, they also carry risks like graft-versus-host disease (GVHD).
Autologous transplants have less GVHD risk but might have a higher chance of relapse.
Choosing the right bone marrow transplant for AML patients depends on several factors. These include the patient’s health, the AML’s characteristics, and donor availability. We carefully consider these to tailor the treatment to each patient’s needs.
Understanding allogeneic and autologous stem cell transplants helps us navigate AML treatment. This way, we can make informed decisions about the best transplant type for each patient.
The bone marrow transplant journey has many steps. These include checking the patient’s health before the transplant, the treatment to prepare the body, and the recovery after. This detailed process needs careful planning and dedicated care to help patients with Acute Myeloid Leukemia (AML) get better.
Before a bone marrow transplant, patients go through a detailed check-up. This check-up looks at their health, the AML, and if they match with a donor. Checking this early is key to finding risks and planning how to avoid them.
Patients and their families also learn about the transplant, possible problems, and how to follow care instructions after. This learning is important to make sure patients are ready physically and emotionally for the transplant.
The conditioning regimen is a key part of the transplant process. It uses strong chemotherapy and/or radiation to kill the bad bone marrow. This treatment also weakens the immune system, making infections more likely.
“The conditioning regimen is designed to kill the cancer cells and make room for new stem cells to grow and make healthy blood cells.”
On transplant day, the patient gets the stem cells through an IV, like a blood transfusion. The stem cells go to the bone marrow to start making new blood cells. The transplant itself is fast, but getting better and making new blood cells takes weeks to months.
After the transplant, care is very important to manage problems and help the patient get better. Patients are watched for signs of graft-versus-host disease (GVHD), infections, and other issues. They get support like medicines, food help, and emotional support to get through this tough time.
| Post-Transplant Care Aspect | Description | Importance |
|---|---|---|
| Monitoring for GVHD | Regular check-ups and symptom assessment | High |
| Infection Prevention | Prophylactic antibiotics and isolation measures | High |
| Nutritional Support | Dietary counseling and supplements | Medium |
| Emotional Counseling | Psychological support for patients and families | High |
Knowing about the transplant process and the care needed helps patients and families. With the right care and support, many patients can have a good outcome and a better life after a bone marrow transplant.
Bone marrow transplantation is a key treatment for Acute Myeloid Leukemia (AML). It depends on the patient’s age and health. Knowing the success rates and survival stats is vital for both patients and doctors.
Bone marrow transplantation is a main treatment for AML. It offers a chance for a cure for many. The success rate varies based on the patient’s age, AML type, and health.
Younger patients and those in better health tend to do better. For example, younger AML patients in first remission have better outcomes than older ones or those with advanced disease.
AML patients over 60 see a big improvement in 5-year survival with bone marrow transplant. Yet, older patients face higher risks of side effects and death.
We weigh the benefits and risks of bone marrow transplant for older patients. We consider their health, function, and AML type.
Many factors affect the success of bone marrow transplantation in AML patients. These include:
Relapse is a big worry after bone marrow transplant for AML. The risk depends on the disease status at transplant and minimal residual disease presence.
| Disease Status at Transplant | Relapse Rate | 5-Year Survival Rate |
|---|---|---|
| First Remission | 20-30% | 50-60% |
| Advanced Disease | 50-60% | 20-30% |
Many AML patients can achieve long-term remission with bone marrow transplant, mainly those transplanted in first remission.
Recovering from a bone marrow transplant comes with many challenges. This treatment can save lives but comes with risks. It’s important to know what these risks are.
Graft-Versus-Host Disease (GVHD) is a serious issue after some stem cell transplants. It happens when the donor cells attack the recipient’s healthy cells. This can cause symptoms in the skin, liver, and stomach.
Managing GVHD means using medicines to calm down the immune system. Catching it early and treating it fast is key to avoiding lasting harm.
After a bone marrow transplant, infections are a big worry because the immune system is weak. It takes a long time for the immune system to get better, sometimes up to a year or more. Patients can get sick from bacteria, viruses, and fungi.
To lower these risks, doctors give antibiotics and teach patients how to stay safe from infections. Watching for signs of infection and treating them quickly is very important.
Long-term effects of bone marrow transplants can include damage to organs, new cancers, and other problems. The chance of these issues depends on many things, like the treatment used, the patient’s age, and their health before the transplant.
Regular follow-up care is key to spotting and dealing with these long-term effects. This means seeing doctors often, checking how organs are working, and looking for new cancers.
Handling the side effects of bone marrow transplants well needs a team effort. It’s not just about treating immediate problems but also watching for long-term issues and helping patients live better lives.
A team of doctors, nurses, and specialists work together to care for these patients. They have the knowledge and experience needed to help bone marrow transplant patients.
The field of bone marrow transplantation is evolving fast. New methods in donor matching, conditioning, and care after transplant are making a big difference. These changes are leading to better results for patients.
Donor matching has gotten much better. High-resolution HLA typing is now common. This means donors and recipients are matched more accurately. This has cut down the risk of graft-versus-host disease (GVHD), a big problem with allogeneic transplants.
We can now find donors more easily, even if they’re not related. This has opened up more options for patients. It helps those who don’t have a related donor.
Reduced-intensity conditioning (RIC) regimens are another big step forward. They are less harsh than old methods. This makes transplant possible for older patients or those with health issues who couldn’t get it before.
RIC regimens are safer but keep the good effects of the transplant. They help fight leukemia without harming the patient too much.
After transplant, care has improved a lot. We watch patients closely and tackle problems early. This includes checking for cancer cells and using targeted therapies to stop cancer from coming back.
We also have new ways to deal with GVHD. This is a big problem with transplants from someone else.
New studies aim to make transplants even safer and more effective. Researchers are looking into using haploidentical donors and cord blood transplants. These options are for patients without a matched donor.
They’re also working on better ways to help the immune system recover after transplant. And they want to lower the chance of cancer coming back. For more on who can get a bone marrow transplant, check out Liv Hospital’s resource page.
After a bone marrow transplant, patients face many challenges. These include physical, emotional, and psychological issues. Getting back to health is a long journey that needs both medical care and personal strength.
Recovering physically is key after a transplant. Patients often feel tired, weak, and more prone to infections. A good rehabilitation program helps them get stronger. This includes therapy, nutrition advice, and doctor checks.
It’s important to have a rehabilitation plan that fits each patient. This helps them smoothly return to their daily lives.
The emotional and psychological effects of a transplant are big. Patients might feel anxious, depressed, or worried about getting sick again. Support from loved ones and mental health experts is key to dealing with these feelings.
Emotional and psychological support is just as important as physical care. Our team works hard to provide the right support and resources.
As patients get better, they can start doing things they love again. This includes going back to work, enjoying hobbies, and reconnecting with friends. Slowly getting back to normal helps them find their identity and purpose.
It’s important for patients to talk to their doctors about when to start doing things again. This helps them avoid pushing themselves too hard.
Many patients who had bone marrow transplants have amazing recovery stories. These stories show the power of the human spirit and the progress in medical care.
These success stories inspire us. They remind us of the value of caring for patients fully during their transplant journey.
Bone marrow transplantation is a promising cure for Acute Myeloid Leukemia (AML). It works best for those with advanced or relapsed disease. This treatment has shown great promise in achieving long-term remission.
This method can be very effective in treating AML. It gives a new immune system to fight cancer cells. The success of the transplant depends on the patient’s health, disease stage, and donor compatibility.
Whether bone marrow transplant cures leukemia varies by individual. For some, it’s a cure, while for others, it’s not as effective. Ongoing research aims to improve donor matching, reduce treatment intensity, and enhance care after the transplant.
Bone marrow transplant is a key option for AML patients. Understanding its benefits and risks helps patients make informed choices. Advances in care offer new hope for a leukemia cure.
Bone marrow transplantation is a key treatment for AML, mainly for those at high risk or who have relapsed. It replaces damaged bone marrow with healthy stem cells from a donor or the patient.
Yes, bone marrow transplantation can cure many leukemia patients, including those with AML. But, the transplant’s success depends on the patient’s health and their leukemia type.
There are two main types for AML: allogeneic and autologous. Allogeneic uses a donor’s stem cells, while autologous uses the patient’s own.
Allogeneic transplants offer a cure by using a donor’s healthy stem cells. Autologous transplants are easier but riskier for relapse.
GVHD is a risk with allogeneic transplants, where donor cells attack the patient’s tissues. Effective management is key for recovery and quality of life.
Long-term side effects include infertility, secondary cancers, and organ damage. Patients need ongoing monitoring and care to manage these issues.
Advances like better donor matching, reduced conditioning regimens, and post-transplant care have improved AML patient outcomes and reduced complications.
The 5-year survival rate varies by age and health. While challenging, transplantation has boosted survival rates, even for those over 60.
Yes, bone marrow transplantation can cure many leukemia patients. Success depends on the patient’s health and leukemia specifics.
Stem cell leukemia involves targeting leukemia stem cells, which start and progress AML. This is critical for effective treatment.
AML bone marrow transplant replaces damaged marrow with healthy stem cells. This aims to restore healthy blood cell production.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!