Chemotherapy is a key treatment for many cancers. But, it can also lead to rare secondary cancers, like leukemia. The American Cancer Society says some chemotherapy drugs have been linked to different kinds of second cancers. This includes myelodysplastic syndrome (MDS) and acute myelogenous leukemia (AML).
We look into how lifesaving cancer treatments might increase the risk of leukemia. While most patients benefit greatly from chemotherapy, knowing the risks is key. It helps in making better care choices.
We aim to give detailed info on therapy-related blood cancers. This way, patients and doctors can understand the risks and benefits of chemotherapy. Explore the dangerous truth: can chemotherapy cause cancer (secondary malignancy). Crucial facts about this powerful risk.
Key Takeaways
- Chemotherapy drugs can rarely lead to secondary malignancies like leukemia.
- The American Cancer Society has linked certain chemotherapy drugs to MDS and AML.
- Understanding the risks and benefits of chemotherapy is key for informed care decisions.
- The benefits of chemotherapy far outweigh the risks for most patients.
- Patients and healthcare providers must be aware of the risks linked to chemotherapy.
Understanding Chemotherapy and Its Role in Cancer Treatment
Chemotherapy is a key treatment for cancer. It targets cells that grow fast. It’s often used with surgery and radiation to fight cancer.

How Chemotherapy Works to Fight Cancer
Chemotherapy uses drugs to kill cancer cells. These drugs target cells that grow quickly, like most cancer cells. But, they can also harm healthy cells, causing side effects like hair loss and nausea.
The success of chemotherapy depends on many things. These include the cancer type, its stage, and the patient’s health. Knowing how chemotherapy works helps us understand its benefits and risks, like the chance of getting secondary cancers like leukemia.
Common Types of Chemotherapy Drugs
Chemotherapy drugs are grouped by how they work and their effect on cancer cells. Here are some common types:
- Alkylating agents, which damage DNA to stop cancer cells from growing.
- Antimetabolites, which block DNA and RNA production, stopping cancer cell growth.
- Anthracyclines, a type of antibiotic that stops cancer cells from replicating by altering DNA.
- Topoisomerase inhibitors, which disrupt the enzyme topoisomerase needed for DNA replication.
Knowing about different chemotherapy drugs helps us understand how they can lead to secondary cancers, like leukemia. The risk of getting leukemia from chemotherapy depends on the drug type and dose.
What Is Leukemia? Types and Characteristics
Leukemia is a cancer where white blood cells grow too much. It affects the blood and bone marrow, causing problems. Knowing about leukemia helps us see the dangers of chemotherapy.
Leukemia is not just one disease. It’s a group of blood cancers starting in the bone marrow. Each type is based on the cell type and how fast it grows.
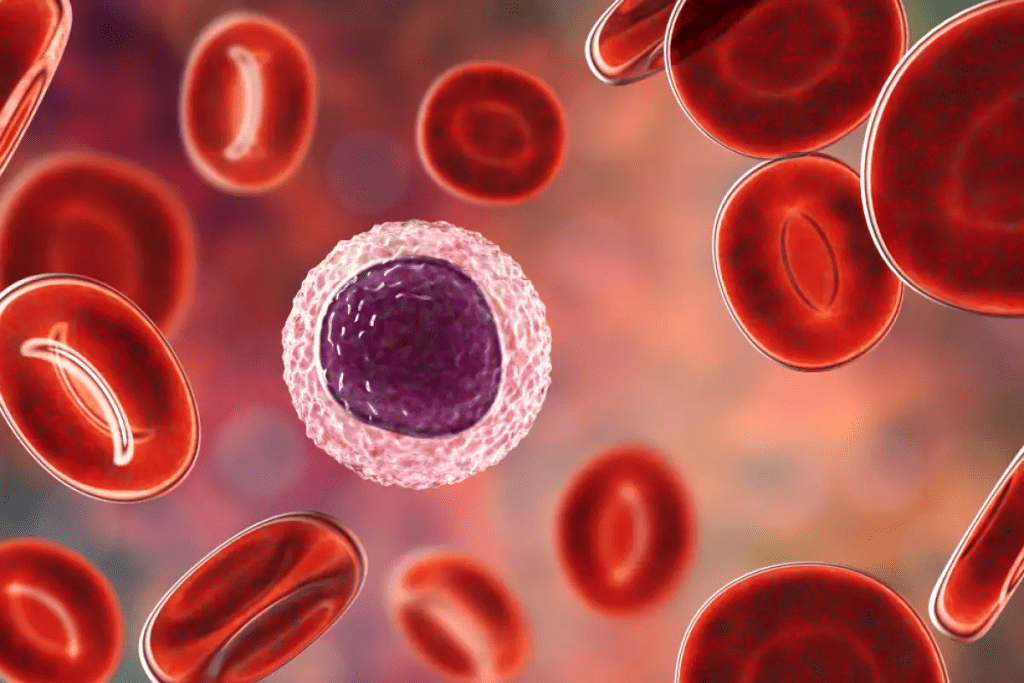
Acute vs. Chronic Leukemia
Leukemia is split into acute and chronic types. Acute leukemia grows fast, with young blood cells. Chronic leukemia grows slower, with older blood cells.
Acute leukemia needs quick treatment because it’s aggressive. Chronic leukemia might be watched for a while before treatment starts. Knowing the difference helps choose the right treatment.
Myeloid vs. Lymphocytic Leukemia
Leukemia can also be divided by the blood cell type affected. Myeloid leukemia deals with cells making red blood cells and platelets. Lymphocytic leukemia affects immune system cells.
Knowing if it’s myeloid or lymphocytic leukemia is key. It affects treatment and how well you might do. For example, some chemotherapy can lead to acute myeloid leukemia (AML).
Understanding leukemia’s types and traits helps us see the risks of chemotherapy. It shows why careful treatment planning is so important.
Can Chemotherapy Cause Cancer? The Paradoxical Risk
Many patients wonder to know, can chemotherapy cause cancer? Chemotherapy is a key treatment for cancer, but it can also raise the risk of new cancers. This includes leukemia. It works by killing cancer cells but can harm healthy cells too, leading to new cancers.
“The risk of secondary malignancies after chemotherapy is a big concern,” says a top oncologist. “It’s important to weigh the benefits and risks of chemotherapy carefully.”
The Concept of Secondary Malignancies
Secondary malignancies are cancers that come from previous treatments, like chemotherapy and radiation. They can show up months or years after treatment ends. This is a worry because more people are surviving their first cancer thanks to good treatments.
Some chemotherapy drugs are more likely to cause these cancers. For example, alkylating agents can lead to therapy-related leukemia.
Therapy-Related Leukemia: Definition and Prevalence
Therapy-related leukemia happens after getting chemotherapy or radiation. It’s a rare but serious side effect of cancer treatment. The chance of getting it depends on the chemotherapy type, dose, and how long it’s used.
Studies show that high doses of chemotherapy, like alkylating agents or topoisomerase II inhibitors, increase the risk. Knowing these risks helps us find ways to lower them.
As we keep improving cancer survival rates, we must also tackle the long-term risks of chemotherapy. By understanding both the risks and benefits, we can create safer, more effective treatments. This will help reduce the chance of secondary malignancies.
Mechanisms Behind Chemo-Induced Leukemia
Chemotherapy can lead to leukemia by affecting our DNA and bone marrow. It targets fast-growing cancer cells but also hits other fast-growing cells, like those in the bone marrow.
DNA Damage and Genetic Mutations
Chemotherapy drugs can harm the DNA in bone marrow cells. This harm can create abnormal cells that might turn into leukemia. Alkylating agents and topoisomerase II inhibitors are types of drugs linked to a higher risk of leukemia.
Genetic changes from chemotherapy can mess with genes that control cell growth and division. For example, mutations in genes that manage the cell cycle or DNA repair can lead to leukemia. Knowing about these genetic changes helps us find ways to lower the risk of therapy-related leukemia.
Bone Marrow Suppression and Recovery
Chemotherapy can weaken the bone marrow, reducing blood cell production. This effect is usually temporary but can sometimes harm bone marrow stem cells for a long time. The bone marrow’s recovery after chemotherapy can bring out abnormal cells that might turn into leukemia.
We’re studying how the bone marrow reacts to chemotherapy and how to make it safer. Research aims to create new treatments that don’t damage DNA as much. This could lower the chance of getting leukemia from treatment.
High-Risk Chemotherapy Agents and Treatments
Some chemotherapy agents can increase the risk of leukemia. It’s important to know which treatments are most risky. This knowledge helps in choosing the best cancer treatment.
Alkylating Agents and Their Effects
Alkylating agents are a type of chemotherapy drug. They are linked to a higher risk of leukemia. These drugs damage DNA in both cancer and healthy cells, which can lead to new cancers. Research shows a high risk of leukemia from these drugs, mainly in the first 5-10 years after treatment.
Topoisomerase II Inhibitors and Leukemia Risk
Topoisomerase II inhibitors are another risky group of chemotherapy drugs. They block an enzyme needed for DNA replication. This can cause genetic changes that may lead to leukemia, with a high risk for acute myeloid leukemia (AML).
Does Radiation Therapy Cause Cancer? Combined Treatment Risks
Radiation therapy is used to treat many cancers, often with chemotherapy. While it saves lives, it can also cause secondary cancers. The risk of leukemia may increase when chemotherapy and radiation are used together. We need to weigh these risks when choosing treatments and find ways to reduce them.
In summary, knowing the risks of certain chemotherapy agents and treatments is key to managing leukemia risk. By identifying high-risk treatments, we can aim to reduce these risks while treating cancer effectively.
Timeline and Risk Factors for Developing Secondary Leukemia
Chemotherapy is a lifesaver but also carries a risk of secondary leukemia. This risk changes over time. It’s key for patients and doctors to know this to make smart treatment choices.
Typical Latency Period After Chemotherapy
The time it takes to develop secondary leukemia after chemo is 5 to 10 years. This time is important for watching and catching the disease early. Regular check-ups with doctors are vital during this period.
Patient-Specific Risk Factors
Many things can affect a person’s risk of getting secondary leukemia. These include genetic predispositions, age, and other health issues. Knowing these can help figure out a person’s risk.
Cumulative Dose and Treatment Duration Considerations
The amount and length of chemotherapy matter a lot. Higher doses and longer treatments raise the risk. This shows why it’s important to watch and plan chemo carefully.
Looking at these factors helps us understand secondary leukemia risk better. Knowing the typical time, individual risks, and the effects of chemo dose and length helps manage this risk.
Statistical Analysis: How Common Is Therapy-Related Leukemia?
It’s important for patients and doctors to know about therapy-related leukemia. This rare side effect of chemotherapy has been studied a lot. Researchers want to know how likely it is and how it affects cancer survivors.
Absolute Risk Compared to General Population
Research shows that 0.5% to 1% of patients treated with chemotherapy might get secondary leukemia. This means less than 1 in 100 patients could develop it. Even though the risk is low, it’s not the same for all chemotherapy treatments.
The risk changes based on the chemotherapy drugs, how much is used, and for how long. For example, certain drugs increase the risk of secondary leukemia. Knowing this helps in making better treatment choices.
Survival Rates and Prognosis for Secondary AML and MDS
Therapy-related AML and MDS are common secondary cancers. They often have a worse prognosis than primary ones. Survival depends on the patient’s age, the leukemia’s genetics, and how well it responds to treatment.
Studies show that therapy-related AML’s 5-year survival rate is between 10% and 20%. This is much lower than primary AML. Therapy-related MDS also has a tough prognosis, with a high chance of turning into AML and a short median survival.
Patients who have had chemotherapy should be watched closely for signs of secondary cancers. Catching them early and treating them right can make a big difference.
Monitoring and Early Detection After Chemotherapy
After chemotherapy, it’s key to watch for signs of secondary cancers like leukemia. This time is very important for patients. We need to keep a close eye to avoid long-term problems. By following up closely, we can help patients do better.
Recommended Follow-Up Protocols
Good follow-up care means regular visits, blood tests, and sometimes bone marrow biopsies. We suggest a follow-up plan that fits each patient’s needs and risks. This way, doctors can catch problems early.
Key components of follow-up protocols include:
- Regular blood tests to monitor blood cell counts
- Periodic bone marrow biopsies to check for abnormalities
- Imaging tests as necessary to monitor overall health
Warning Signs and Symptoms to Watch For
It’s important for patients to know the signs of secondary leukemia. We stress the need to catch these symptoms early. Look out for ongoing tiredness, frequent infections, and unexplained bleeding or bruising.
It’s vital for patients to tell their doctors about any unusual symptoms right away.
The Role of Healthcare Providers in Long-term Monitoring
Healthcare providers are key in watching over patients after chemotherapy. We work with patients to create follow-up plans that fit their needs. This helps manage long-term effects and improves life quality for cancer survivors.
By keeping a close eye and catching problems early, we can lower the risk of therapy-related leukemia. This helps improve patient outcomes and supports future cancer treatments.
The Future of Cancer Treatment: Reducing Secondary Cancer Risks
New ways to fight cancer are being developed to lower the risk of therapy-related leukemia and other cancers. Our growing knowledge of cancer helps us create better treatments. These treatments aim to reduce long-term risks while keeping or improving their effectiveness.
Targeted Therapies with Lower Leukemia Risk
Targeted therapies are a big step forward in cancer treatment. They are different from traditional chemotherapy, which can harm DNA and increase cancer risk. Targeted therapies aim to attack cancer cells directly, possibly lowering the risk of leukemia.
Examples of targeted therapies include:
- Monoclonal antibodies that target specific proteins on cancer cells
- Tyrosine kinase inhibitors that block signals promoting cancer cell growth
- Proteasome inhibitors that disrupt protein processing in cancer cells
These therapies have shown promise in lowering secondary cancer risks compared to traditional chemotherapy. For example, a study found that patients treated with certain targeted therapies had a much lower risk of developing MDS and AML. This is compared to those who received traditional chemotherapy.
Personalized Medicine Approaches to Treatment Selection
Personalized medicine is also key in reducing secondary cancer risks. By looking at a patient’s genetic profile, we can find the best treatments with the least side effects.
Key aspects of personalized medicine include:
- Genetic testing to identify mutations that can guide treatment choices
- Pharmacogenomics to predict how a patient will metabolize certain drugs
- Risk assessment models to estimate the likelihood of developing secondary malignancies
By tailoring treatments to each patient, we can avoid harmful therapies. This approach improves treatment results and lowers the risk of long-term problems, like leukemia.
As we move forward in oncology, combining targeted therapies and personalized medicine will be vital. It will help make cancer treatment safer and more effective for people all over the world.
Conclusion: Understanding and Managing the Risk of Chemo-Induced Leukemia
We’ve looked into how chemotherapy and leukemia are connected. We talked about the risks, how it happens, and ways to lower the chance of getting leukemia from treatment. It’s key for patients and doctors to work together to get the best results.
The worry about getting leukemia after chemotherapy is real. Knowing the factors that increase this risk is important. We can manage this risk better by planning treatments carefully and keeping a close eye on patients.
As we keep improving cancer treatments, we must weigh the good and bad of chemotherapy. This way, we can help patients do better and lower the chance of getting leukemia from treatment. Managing cancer treatment well means looking at all the risks and benefits of chemotherapy.
FAQ
Can chemotherapy cause leukemia?
Yes, chemotherapy can raise the risk of secondary leukemia, though it’s rare. Certain drugs, like alkylating agents and topoisomerase II inhibitors, carry a higher risk.
What is therapy-related leukemia?
Therapy-related leukemia is leukemia caused by cancer treatment, often chemotherapy or radiation. It’s a secondary cancer type.
How does chemotherapy cause leukemia?
Chemotherapy can damage bone marrow cells’ DNA, leading to genetic mutations and leukemia. It also affects bone marrow recovery, increasing the risk of therapy-related leukemia.
What are the risk factors for developing secondary leukemia after chemotherapy?
Several factors influence the risk of secondary leukemia, including the chemotherapy type and dose, treatment length, and patient characteristics.
Can radiation therapy cause cancer?
Yes, radiation therapy can increase the risk of secondary cancers, including leukemia. This risk is higher when combined with chemotherapy.
How can the risk of therapy-related leukemia be minimized?
Minimizing therapy-related leukemia risk involves using targeted therapies with lower risks. Personalized medicine and careful monitoring after treatment are also key.
What are the warning signs and symptoms of leukemia after chemotherapy?
Look out for fatigue, weight loss, frequent infections, and easy bleeding or bruising. Regular check-ups with healthcare providers are vital for early detection.
Can chemotherapy drugs give you cancer?
While chemotherapy aims to kill cancer cells, some drugs can increase the risk of secondary cancers, including leukemia.
How common is therapy-related leukemia?
Therapy-related leukemia is rare but varies based on chemotherapy type and patient factors.
What is the prognosis for secondary AML and MDS?
Secondary AML and MDS prognosis depends on patient health and disease characteristics.
Can PRP (Platelet-rich plasma) cause cancer?
There’s no conclusive evidence that PRP causes cancer. Discussing risks and benefits with a healthcare provider is essential.
What is the future of cancer treatment in reducing secondary cancer risks?
Future cancer treatments aim to use targeted therapies and personalized medicine. This aims to improve outcomes while reducing long-term risks.
References
- Morton, L. M., et al. (2013). Evolving risk of therapy-related acute myeloid leukemia following chemotherapy for adult cancers. Blood, 121(15), 2996-3004.https://ashpublications.org/blood/article/121/15/2996/31344/Evolving-risk-of-therapy-related-acute-myeloid
- Valentini, C. G., et al. (2011). Incidence of acute myeloid leukemia after breast cancer. BMC Cancer, 11, 470.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3248346/