Hepatoblastoma is a rare liver cancer mostly found in children. It can come back, which is a big worry. Even with better treatments, about a third of cases see it return. It’s important to know what makes it come back.
The recurrence of hepatoblastoma affects how long patients can live. This shows we need to keep working on new treatments and ways to manage it. Knowing the symptoms and prognosis of hepatoblastoma helps find it early and treat it fast.
Key Takeaways
- Understanding hepatoblastoma recurrence is key to better survival rates.
- Risk factors are big in making a come back.
- New treatments are being made to fight recurrence.
- Finding it early and acting fast is vital in managing hepatoblastoma.
- We must keep researching to help patients more.
What is Hepatoblastoma: An Overview
Hepatoblastoma is a rare and aggressive liver cancer found mainly in children. It’s important to know about it to catch it early and treat it effectively.
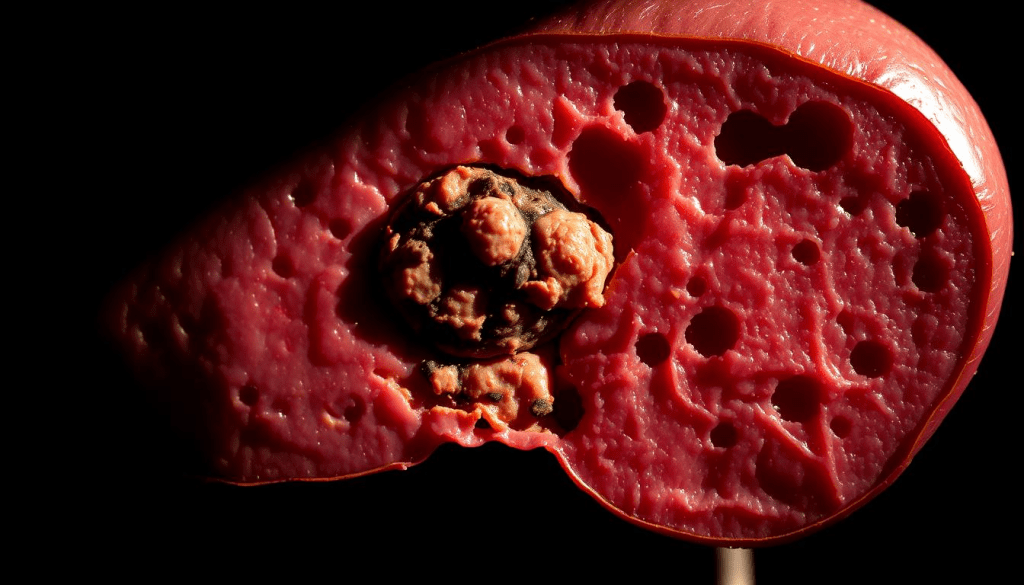
Definition and Classification
Hepatoblastoma starts in immature liver cells and is a cancer. It’s divided into types based on how it looks under a microscope. These include:
- Epithelial type
- Mixed epithelial and mesenchymal type
- Other rare subtypes
Knowing the type of hepatoblastoma helps doctors plan the best treatment. Accurate diagnosis is key to figuring out the type.
Epidemiology in Children
Hepatoblastoma mostly hits kids under 3. It’s a rare cancer, affecting about 1.5 in a million kids under 15. This shows why it’s vital to watch for it in young patients.
Important facts about hepatoblastoma include:
- Age: Most cases are found in the first 18 months.
- Gender: Boys are slightly more likely to get it.
- Genetic links: Some genetic conditions raise the risk.
Standard Treatment Approaches for Hepatoblastoma
Managing hepatoblastoma often needs a mix of surgical management and chemotherapy protocols. This childhood liver cancer treatment is complex. It involves a team of specialists working together.
Surgical Management
Surgery is key in treating hepatoblastoma. The main goal is to remove the tumor completely. Modern surgery techniques help in precise removals, leading to better results. Sometimes, liver transplantation is considered for tumors that can’t be removed.
Chemotherapy Protocols
Chemotherapy is used alongside surgery to treat hepatoblastoma. The type of chemotherapy depends on the disease’s stage and risk. Common drugs include cisplatin, vincristine, and 5-fluorouracil. Chemotherapy before surgery can make tumors smaller, making them easier to remove.
Combining chemotherapy and surgery has greatly improved treatment outcomes for children with hepatoblastoma. A team approach ensures all disease aspects are covered, leading to better results.
Understanding Hepatoblastoma Recurrence Patterns
It’s key to know how hepatoblastoma comes back to help patients better. This liver cancer in kids can return after treatment. Knowing when and how it comes back helps doctors plan better care and treatments.
Recurrence Statistics
Research shows that hepatoblastoma can come back in 20% to 30% of cases. Several things affect how likely it is to come back. These include the cancer’s first stage, how well the surgery went, and how the chemotherapy worked.
Recurrence Rates:
| Study | Recurrence Rate |
| Study A | 25% |
| Study B | 28% |
| Study C | 22% |
Sites of Recurrence
Hepatoblastoma can come back in the liver or in other parts of the body. The most common places for it to spread are the lungs, lymph nodes, and sometimes other organs.
Local recurrence happens when not all cancer is removed or when tiny bits are left behind. Distant recurrence usually means the cancer has spread through the blood.
Knowing where and how it comes back is important. It helps doctors plan better for watching for and treating any return of the cancer.
Risk Factors That Increase Chance of Hepatoblastoma Return
Knowing what increases the risk of hepatoblastoma coming back is key to better care. Hepatoblastoma is a rare liver cancer mostly found in kids. It can come back if not managed well.
Patient-Related Factors
Some things about the patient can raise the risk of hepatoblastoma coming back. For example, how old the patient is when they get diagnosed matters. A study in PLOS ONE found that age and other personal details can affect how well a patient does.
Table 1: Patient-Related Risk Factors for Hepatoblastoma Recurrence
| Risk Factor | Description | Impact on Recurrence |
| Age at Diagnosis | Younger than 1 year or older than 3 years | Increased risk |
| Genetic Predisposition | Presence of genetic syndromes | Potential increase |
Disease-Related Factors
How big the tumor is and if it has spread are also important. If the tumor is big or has spread, it’s harder to treat and more likely to come back.
The size of the tumor and if it has spread are big factors in whether it will come back. Knowing this helps doctors plan better treatments to help patients.
Detecting Recurrent Hepatoblastoma
Finding recurrent hepatoblastoma needs a mix of steps. We look at symptoms, use new imaging, and check tumor markers. Catching it early is key to better care and results.
Clinical Manifestations
Signs of recurrent hepatoblastoma can be hard to spot. Symptoms like belly pain, losing weight, and feeling tired are common. Sometimes, you can feel a lump in the belly.
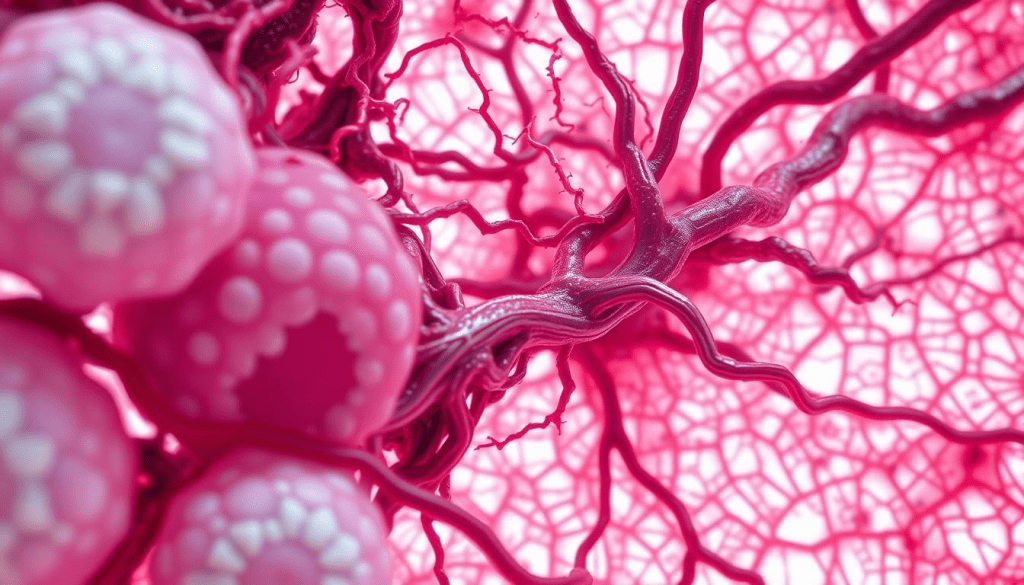
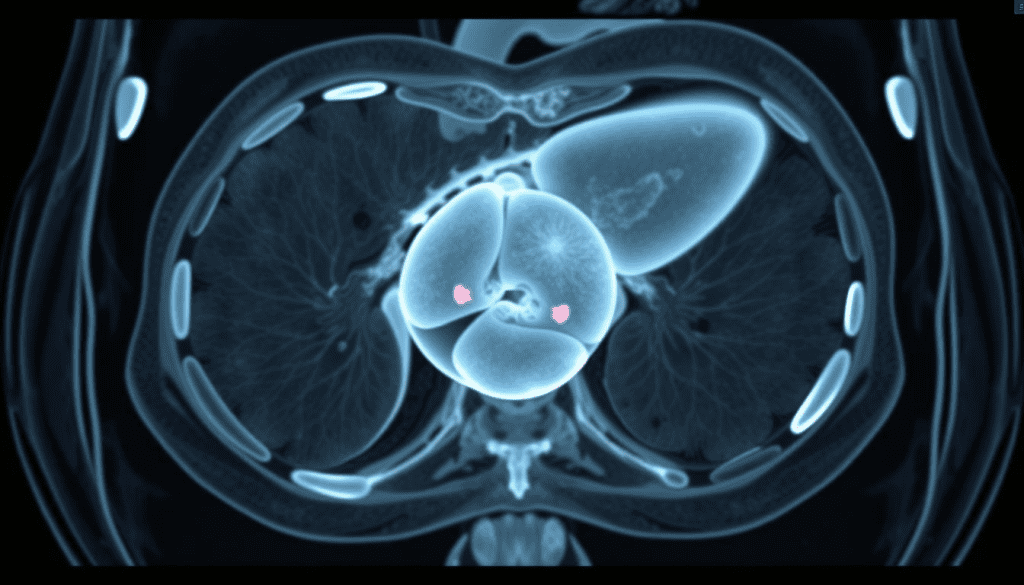
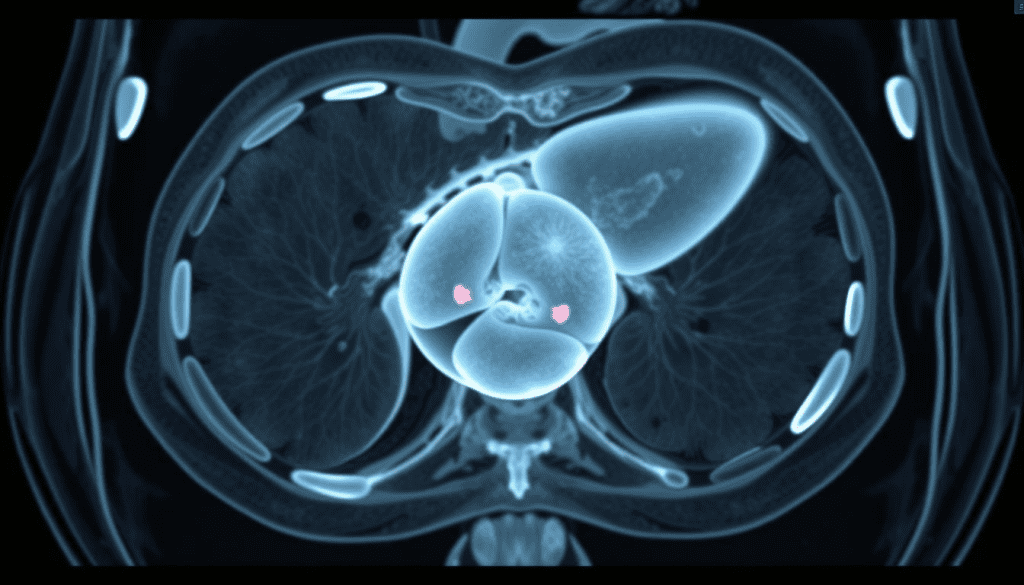
Imaging Techniques
MRI and CT scans are key for spotting this cancer again. They help see how big, where, and how far the tumor has spread.
Tumor Marker Elevation
Alpha-fetoprotein (AFP) levels rising is a big sign of this cancer coming back. Keeping an eye on AFP is important. A jump in AFP means we should look closer with scans.
| Detection Method | Description | Importance |
| Clinical Manifestations | Identifying symptoms such as abdominal pain and weight loss | Initial clue to possible recurrence |
| Imaging Techniques | Using MRI and CT scans to find tumor recurrence | Very important for knowing how far it has spread |
| Tumor Marker Elevation | Watching AFP levels for signs of coming back | Early sign of possible recurrence |
Post-Treatment Surveillance Strategies
After treatment, watching for signs of hepatoblastoma is key. It helps catch any return early. This means doctors can act fast.
Recommended Follow-up Schedules
Patients see their doctors often after treatment. How often depends on their risk and treatment. They get regular imaging and lab tests to watch for signs of the cancer coming back.
Surveillance Modalities
Doctors use ultrasound, CT scans, and MRI to keep an eye on patients. The choice depends on the patient’s risk and the doctor’s view. They also watch AFP levels closely. These levels can show if the cancer is coming back.
Risk-Adapted Surveillance
Surveillance plans are made for each patient. Those at higher risk get checked more often and with more detailed tests. This helps find and treat any return early.
Using a careful plan for watching patients helps doctors catch cancer early. This leads to better care and outcomes for patients.
Treatment Options for Recurrent Hepatoblastoma
When hepatoblastoma comes back, treatment needs to change. It’s about finding new and personal ways to fight the disease. This means using many different treatments together to tackle the cancer effectively.
Salvage Chemotherapy Regimens
Salvage chemotherapy is key for treating recurring hepatoblastoma. It uses a mix of drugs, chosen based on the patient’s past treatments and the tumor’s details. For example, ifosfamide, carboplatin, and etoposide (ICE) are sometimes used.
“The role of salvage chemotherapy in recurrent hepatoblastoma is to achieve tumor control, potentially rendering the tumor resectable or improving survival outcomes.”
Surgical Approaches for Relapse
Surgery is also very important for managing recurring hepatoblastoma. It’s most useful when the cancer is in one place. Doctors might remove the tumor or do a liver transplant. The choice depends on how far the cancer has spread and the patient’s health.
| Surgical Approach | Indications | Outcomes |
| Tumor Resection | Localized recurrence | Potential for cure or improved survival |
| Liver Transplantation | Unresectable disease or extensive liver involvement | Offers a chance for long-term survival in selected patients |
Innovative and Experimental Therapies
New treatments are giving hope to those with recurring hepatoblastoma. These include targeted therapies, immunotherapy, and other new methods being tested in trials. Joining these trials can give patients access to the latest treatments and help improve care for others in the future.
Dealing with recurring hepatoblastoma is a big challenge. It needs a team effort to find the best treatment. By using chemotherapy, surgery, and new therapies, doctors can create plans that fit each patient’s needs.
Survival Outcomes After Hepatoblastoma Recurrence
Hepatoblastoma recurrence is a big challenge, but new treatments have helped improve survival rates. It’s important to know what affects survival to manage the disease well.
Statistical Prognosis
The outlook for patients with recurrent hepatoblastoma depends on several things. These include where the cancer comes back, how long it takes, and the first treatment. Research shows survival rates can be between 30% and 70% based on these factors.
| Recurrence Site | Time to Recurrence | 5-Year Survival Rate |
| Liver | Early (<6 months) | 40% |
| Liver | Late (>6 months) | 60% |
| Extrahepatic | Early (<6 months) | 20% |
| Extrahepatic | Late (>6 months) | 50% |
Prognostic Factors
Several factors are key in predicting survival for patients with recurrent hepatoblastoma. These include how well the cancer responded to the first treatment, if it spread, and the patient’s health.
- Initial Treatment Response: Patients who responded well to the first treatment tend to do better when it comes back.
- Metastatic Disease: If the cancer has spread, it makes the outlook worse.
- Patient’s Health Status: The patient’s overall health and how well they can handle treatment are very important.
Recent Improvements in Outcomes
In recent years, there have been big steps forward in treating recurrent hepatoblastoma. New chemotherapy and surgical methods have been developed. These have helped patients live longer.
Using a team approach and tailoring treatment to each patient has also made a big difference. This has led to better survival rates and a better quality of life for patients.
Multidisciplinary Approach to Recurrent Disease
Dealing with recurrent hepatoblastoma gets better with a team effort. This team makes sure every part of the disease is handled well. This leads to better results for patients.
Team Composition
A team for recurrent hepatoblastoma includes doctors, surgeons, and radiologists. Working together, they create a detailed treatment plan.
Role of Specialized Treatment Centers
Specialized centers are key in fighting recurrent hepatoblastoma. They offer new treatments and clinical trials. These can greatly help patients.
| Center Type | Services Offered | Benefits |
| Specialized Cancer Centers | Advanced chemotherapy, surgical options, and clinical trials | Access to innovative treatments |
| Pediatric Oncology Units | Specialized care for children, family support services | Comprehensive care for young patients |
Personalized Treatment Planning
Personalized plans are key for treating recurrent hepatoblastoma. They are made to fit each patient’s needs and disease.
With a team effort, doctors can give personalized and complete care. This helps patients with recurrent hepatoblastoma get better treatment chances.
Livhospital’s Approach to Hepatoblastoma Management
At Livhospital, treating hepatoblastoma is a team effort. We use innovative treatments and focus on family-centered care. Our goal is to help patients and support their families every step of the way.
Comprehensive Care Pathways
Livhospital creates comprehensive care pathways for each patient. These plans include surgery, chemotherapy, and follow-up care. They help manage hepatoblastoma effectively and smoothly.
Innovative Treatment Access
Patients at Livhospital get access to innovative treatments. We use the latest in chemotherapy and surgery. Our aim is to give patients the best care possible.
Family-Centered Support Services
Livhospital knows how hard hepatoblastoma is on families. That’s why we offer family-centered support services. We provide counseling, nutritional advice, and psychological support to help families through tough times.
“The care we received at Livhospital was exceptional. The team was supportive and knowledgeable, making a difficult journey much more manageable.”
By combining all these elements, Livhospital is leading the way in treating hepatoblastoma. We focus on care, innovation, and family support.
Conclusion
Hepatoblastoma is a rare liver cancer in kids that can come back. Knowing the risks is key to managing it well. The disease’s patterns and treatments, like chemotherapy and surgery, show we need a team effort.
A good treatment plan, with new therapies and care tailored to each child, can help more kids live. We must keep studying hepatoblastoma to find better ways to fight it. This helps us understand and treat childhood liver cancer better.
Managing hepatoblastoma well needs teamwork from doctors, researchers, and families. Together, we can give kids with this disease a better chance at life. This summary shows why we must keep researching and personalizing care for kids with liver cancer.
FAQ
What is hepatoblastoma?
Hepatoblastoma is a rare liver cancer in kids. It happens in the first few years of life. It starts in the liver’s early cells.
What are the symptoms of hepatoblastoma?
Signs include a big belly from a growing tumor, less hunger, and weight loss. Sometimes, kids get jaundice. Finding it early is key to treating it well.
How is hepatoblastoma diagnosed?
Doctors use ultrasound, CT scans, or MRI to see the tumor. They also check blood for alpha-fetoprotein (AFP). AFP is a marker for this cancer.
What are the treatment options for hepatoblastoma?
Treatment includes surgery to remove the tumor and chemotherapy to kill cancer cells. The plan depends on the tumor’s size, where it is, and the child’s health.
Can hepatoblastoma recur after treatment?
Yes, it can come back. The chance of it coming back depends on the tumor’s size, how well the first treatment worked, and if it spread.
What is the prognosis for children with recurrent hepatoblastoma?
The outlook varies. It depends on where the cancer came back, how long it took to come back, and how well it responds to treatment. New treatments have helped some kids.
How is recurrent hepatoblastoma detected?
Doctors use regular tests and check tumor markers like AFP. Symptoms like belly pain or a growing belly can also show it’s back.
What is the role of a multidisciplinary team in managing hepatoblastoma?
A team of doctors, including oncologists and surgeons, is key. They work together to diagnose, treat, and manage the disease. This ensures the best care for the child.
Reference
Li, F., et al. (2021). Factors influencing recurrence after complete remission in hepatoblastoma: A retrospective study. Frontiers in Oncology, 11, 1582.


































