Last Updated on November 26, 2025 by Bilal Hasdemir

Can I Drive After Chemotherapy? What to Know About Living Independently
Chemotherapy is a challenging journey, especially for those living alone. Studies show that nearly one in five cancer patients undergo treatment without daily support ” making independence and safety even more important.
If you’re wondering, “can I drive after chemotherapy?, the answer depends on how your body responds to treatment. Some people experience fatigue, dizziness, or concentration issues after chemo sessions, which can make driving unsafe. It’s always best to assess how you feel and consult your doctor before getting behind the wheel.
Living independently during chemotherapy requires planning ” from arranging transportation on treatment days to organizing help for meals and household tasks. Understanding your limits and preparing ahead can help you stay safe, comfortable, and confident throughout your treatment.
Key Takeaways
- Assessing your support system is key before starting chemotherapy.
- Creating a care plan helps manage treatment side effects.
- Keeping a daily routine boosts your well-being.
- Staying in touch with loved ones is essential.
- Seeking professional help is a sign of strength.
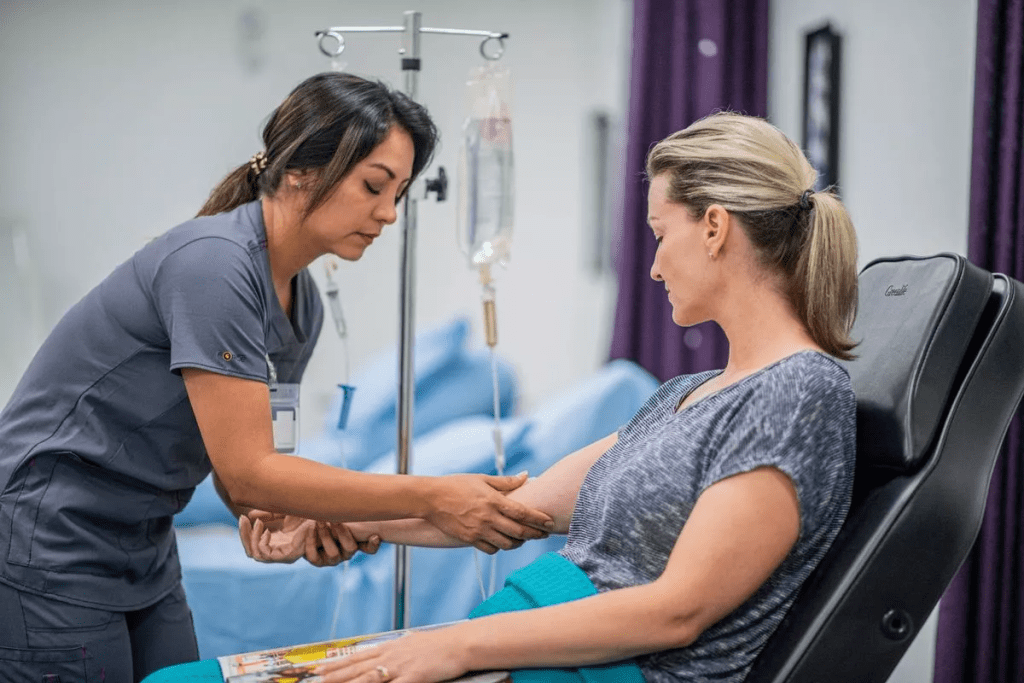
The Reality of Chemotherapy Treatment

Chemotherapy is a key treatment for cancer but comes with many side effects. It’s important for patients to know about these side effects. This knowledge helps them prepare for the challenges they will face.
Common Side Effects and Their Severity
Chemotherapy side effects differ from person to person. They can include fatigue, nausea, hair loss, and increased risk of infection. Some side effects are mild, while others are severe.
The severity of side effects depends on the chemotherapy drugs, dosage, and the patient’s health. For example, some drugs cause severe nausea, while others lead to significant hair loss.
| Side Effect | Severity Level | Impact on Daily Life |
| Fatigue | Moderate to Severe | Reduces ability to perform daily tasks |
| Nausea | Mild to Severe | Affects nutrition and energy levels |
| Hair Loss | Moderate to Severe | Can impact self-esteem and body image |
How Side Effects Impact Daily Independence
Chemotherapy side effects can greatly affect a patient’s daily life. For instance, fatigue makes it hard to do everyday tasks. Nausea can also lower energy levels by affecting nutrition.
To lessen these effects, patients and caregivers can plan rest, adjust diets, and use wigs or headscarves. These steps help patients stay independent during treatment.
Evaluating Your Ability to Live Independently During Treatment
Deciding to live alone during chemotherapy is a big choice. It involves looking at your health and who can help you. Chemotherapy affects people differently, so knowing how it will affect you is key.
Medical Factors to Consider
Your health and cancer treatment type are important. The stage of your cancer and how intense your chemotherapy is also matters a lot.
Some things to think about include:
- The type and stage of your cancer
- The chemotherapy regimen and its side effects
- Any other health issues that might make treatment harder
Personal Support Assessment
Having people you can count on is very important during chemotherapy. Think about who in your family or friends can help you out.
Consider the following:
| Support Type | Description | Frequency |
| Emotional Support | Encouragement and companionship | Daily/Weekly |
| Practical Support | Help with grocery shopping, cooking, and household chores | Weekly |
| Medical Support | Assistance with medication management and accompanying you to appointments | As needed |
Questions to Ask Your Oncologist About Independent Living
Talking to your oncologist about living alone during chemotherapy is important. You should ask them questions like:
- What are the most common side effects of my chemotherapy regimen, and how might they impact my daily life?
- Are there specific tasks or activities that I should avoid during treatment?
- How often should I check in with your office or have someone check on me?
By looking at your health, support system, and talking to your oncologist, you can decide if living alone during chemotherapy is right for you.
Preparing Your Home for Solo Living During Chemotherapy
Getting your home ready for chemotherapy is more than just buying supplies. It’s about making your home safe and comfy. During treatment, your home will be your safe place, helping you both physically and emotionally.
Creating a Chemo-Friendly Environment
A chemo-friendly home reduces stress and boosts comfort. Start by tidying up to avoid falls and make cleaning simpler. Think about your home’s temperature and lighting, as chemo can make you feel cold or light-sensitive.
Adjust your thermostat and use soft, adjustable lights to make your home cozy.
Safety Modifications to Consider
When living alone during chemo, safety is key. Think about making your home safer to prevent accidents. For example, installing handrails in bathrooms and hallways can offer support. Non-slip mats in the shower or bathtub can also prevent falls.
Also, make sure your home is well-lit, in places you often visit like the kitchen and bathroom. A medical alert system can be a lifesaver in emergencies.
Essential Supplies Checklist
Having the right supplies can greatly improve your comfort and safety. Here’s a list of must-haves:
| Supply Category | Items to Consider |
| Comfort and Hygiene | Cozy blankets, comfy clothes, adult diapers (if needed), and hygiene wipes |
| Nutrition | Easy meals, nutritional supplements, and lots of water |
| Medication Management | Pill boxes, medication calendars, and emergency contact numbers |
| Safety and Emergency | First aid kit, flashlight, and a medical alert device |
By making your home chemo-friendly, adding safety features, and having the right supplies, you can improve your life during chemo. Remember, being prepared helps you stay independent and safe during this tough time.
Building a Support Network When Living Alone
Living alone during chemotherapy can be tough. But, having a strong support network can really help. It means you don’t have to face treatment alone.
Creating a good support system is key for your well-being and safety. It includes several important parts. These parts work together to help you during treatment.
Creating an Emergency Contact System
First, make an emergency contact list. Choose people you trust who can help in emergencies or urgent situations.
- Family members or close friends who can check in on you regularly
- Neighbors who know about your treatment and can help if needed
- Healthcare professionals who can offer guidance and support
Make sure these contacts know your treatment schedule and any side effects to watch for.
Scheduling Regular Check-ins
Regular check-ins with your support network are important. They offer emotional support and help keep an eye on your health. Try to schedule regular phone calls or visits with your loved ones.
| Check-in Method | Frequency | Benefits |
| Phone Calls | Daily or Every Other Day | Emotional Support, Monitoring of Condition |
| In-Person Visits | Weekly or Bi-Weekly | Physical Assistance, Social Interaction |
| Video Calls | As Needed | Visual Check-ins, Flexibility |
Virtual and In-Person Support Groups
Joining support groups, online or in-person, can offer more emotional support and practical advice. You’ll get to share experiences and advice with others going through similar things.
Benefits of Support Groups:
- Sharing experiences and advice with others who understand your situation
- Receiving emotional support and reducing feelings of isolation
- Gaining insights into managing treatment side effects and daily challenges
Building a strong support network helps you deal with chemotherapy’s challenges, even when you live alone. We suggest exploring these options and creating a support system that fits your needs.
Managing Daily Activities During Chemotherapy
Chemotherapy patients need to adjust their daily routines due to treatment side effects. It’s important to plan carefully to stay independent and maintain a good quality of life. We’ll look at ways to manage daily tasks during this time.
Meal Preparation Strategies
Meal prep can be tough during chemotherapy. Here are some tips to make it easier:
- Prepare meals ahead of time to save energy.
- Choose simple, healthy recipes.
- Look into meal delivery services or get help from loved ones.
Energy Conservation Techniques
It’s key to save energy during chemotherapy. Here are some tips:
- Focus on important tasks first, based on your energy.
- Take breaks to rest often.
- Do gentle exercises to keep strong without getting too tired.
When to Ask for Help with Tasks
It’s important to know when to ask for help. You might need assistance with:
- Grocery shopping and carrying heavy bags.
- Household chores that are hard to do.
- Getting to and from treatment appointments.
Can I Work While on Chemo?
Many people on chemotherapy wonder if they can keep working. It depends on the type of chemo, your job, and your health.
Some, have kept working during chemo. But, it takes careful planning and talking to your boss. We’ll look at the challenges, the importance of talking to your boss, and the benefits you might get.
Balancing Treatment and Employment
Working while on chemo can be tough. Your treatment schedule, side effects, and energy can affect your job. You should think about your job and talk to your boss about changes.
Here are some ways to balance work and chemo:
- Flexible work arrangements, such as telecommuting or flexible hours
- Modifying job duties to reduce physical or mental strain
- Taking regular breaks to manage fatigue
As cancer survivors say, “Being proactive and talking openly with your boss is key to working during chemo.”
“I had to adjust my work schedule significantly during my chemotherapy treatment. My employer was very understanding and accommodating, which made a huge difference.” – Cancer Survivor
Communicating with Your Employer
Talking to your boss is very important. Tell them about your treatment and any side effects. This helps them understand and make changes.
| Communication Strategy | Benefits |
| Regular updates on treatment progress | Helps employer plan for your absence or adjust workload |
| Discussing possible side effects | Allows employer to make necessary accommodations |
| Providing a doctor’s note or medical documentation | Supports your need for accommodations or leave |
FMLA and Disability Benefits
The Family and Medical Leave Act (FMLA) and disability benefits can help financially. FMLA lets eligible employees take up to 12 weeks off for medical reasons, like cancer treatment.
To get FMLA benefits, you need to show medical proof. Also, know about your company’s disability benefits and how they can help during treatment.
Knowing your rights and benefits can help you work during chemo. By balancing work and treatment, talking to your boss, and using benefits, you can keep your job and manage treatment well.
Can I Drive After Chemotherapy?
Whether you can drive after chemotherapy depends on several things. These include the type of treatment and how you react to it. Chemotherapy can change how you feel and think, which might affect your driving.
Immediate Effects of Treatment on Driving Ability
Chemotherapy can have immediate effects that might make driving hard. These effects include:
- Fatigue: Feeling very tired or weak, making it hard to focus on driving.
- Dizziness or Lightheadedness: Feeling dizzy or lightheaded, which can raise the risk of accidents.
- Numbness or Tingling: Neuropathy causing numbness or tingling in hands and feet, which might affect your ability to drive.
Understanding these effects is key to knowing if you can drive during chemotherapy.
Medication Side Effects That Impact Driving
Some chemotherapy medications can affect your driving. Common side effects include:
- Cognitive Impairment: Trouble concentrating or memory problems that can slow your reaction time while driving.
- Vision Changes: Blurred vision, double vision, or light sensitivity, which can make driving unsafe.
- Reaction Time: Slower reaction times due to medication or treatment side effects.
Knowing about these side effects can help you decide if you should drive during chemotherapy.
What Your Oncologist Wants You to Know About Driving
Your oncologist is a great source of information on how chemotherapy affects driving. They can give you advice tailored to your treatment and health. It’s important to talk to your oncologist about:
- The specific risks of your chemotherapy regimen and driving.
- Any precautions or adjustments to your treatment to reduce driving risks.
- When it’s safe to start driving again after treatment.
By talking to your oncologist, you can make smart choices about driving during and after chemotherapy.
Driving Restrictions After Chemo: What to Expect
Chemotherapy patients often face driving restrictions. Knowing what to expect can help them navigate this challenging period. It’s important to consider the factors that affect a patient’s ability to drive safely.
Typical Timeframes for Driving Limitations
The time when driving is limited varies. It depends on the chemotherapy type, dosage, and how the patient responds. Usually, patients are told not to drive for 24 to 48 hours after treatment. This is because some medications can make you feel drowsy or dizzy.
It’s vital to follow your healthcare provider’s advice. They can give you personalized guidance based on your treatment.
Treatment-Specific Driving Considerations
Different chemotherapy treatments have different side effects. For example, treatments that cause neuropathy can make it hard to drive. This is because numbness or tingling in your hands and feet can slow down your reaction times.
Patients who feel very tired or have cognitive changes may also need to adjust their driving habits.
- Assess your physical condition before driving.
- Consider having someone accompany you on trips.
- Avoid driving during peak fatigue hours.
Legal and Insurance Implications
Driving after chemotherapy is not just about personal safety. It also has legal and insurance implications. Patients must tell their insurance provider if their medical condition affects their driving. Not doing so could mean insurance claims are denied if there’s an accident.
Also, laws about driving with medical conditions vary by place. So, it’s important to know the specific laws in your area.
By understanding the driving restrictions after chemotherapy and taking precautions, patients can stay safe and independent during treatment.
Chemotherapy and Driving Safety Tips
Understanding how chemotherapy affects your driving is key for your safety and others’. It can change how you feel physically and mentally. This makes it important to be extra careful when driving.
Assessing Your Fitness to Drive
Before you drive, check if you’re fit to do so. Chemotherapy can make you feel tired, dizzy, and slow to react. These changes can make driving unsafe.
- Watch how your body reacts to chemotherapy and adjust your driving plans.
- Be aware of side effects like feeling sleepy or seeing things blurry.
- Talk to your oncologist if you’re not sure if you can drive safely.
Key Factors to Consider When Assessing Fitness to Drive:
| Factor | Impact on Driving |
| Fatigue | Slowed reaction times, decreased alertness |
| Dizziness or Lightheadedness | Increased risk of losing control of the vehicle |
| Vision Changes | Blurred vision, sensitivity to light |
Planning Safe Routes and Times
Plan your route and drive at safe times to reduce risks. Try to avoid driving in busy times or heavy traffic when you’re tired or feeling side effects.
Tips for Safe Driving:
- Choose routes with less traffic and no construction.
- Don’t drive at night or early morning if you’re tired.
- Keep your phone charged and ready for emergencies.
Alternative Transportation Options
If you’re not sure you can drive safely, look into other ways to get around. Many places offer rides for cancer patients. Some healthcare providers also help with transportation.
Alternative Transportation Options:
- Public transportation
- Ride-sharing services
- Cancer patient transportation services
- Friends and family
By checking if you’re fit to drive, planning safe times, and looking at other ways to travel, you can stay safe while driving during chemotherapy.
Can You Die From Chemotherapy? Understanding the Risks
Chemotherapy is a double-edged sword. It can save lives but also carries risks. Knowing these risks is key for patient safety and making informed decisions.
Distinguishing Between Side Effects and Complications
Chemotherapy patients often face side effects, from mild to severe. It’s important to know the difference between common side effects and serious complications. Side effects might include nausea, fatigue, and hair loss. Complications, on the other hand, can involve infections, organ damage, or severe allergic reactions.
For example, febrile neutropenia is a serious condition. It’s characterized by a low white blood cell count and fever. Knowing the difference between side effects and complications is critical for timely medical help.
Warning Signs That Require Immediate Medical Attention
Certain symptoms need immediate medical attention. These include:
- Fever above 100.4 °F (38 °C)
- Severe abdominal pain
- Unusual bleeding or bruising
- Shortness of breath or difficulty breathing
- Chest pain or rapid heartbeat
- Severe headache or confusion
Patients should watch for these warning signs and seek help quickly. Delaying treatment can lead to severe consequences, as shown by a patient’s severe complications.
Realistic Perspective on Treatment Risks
Chemotherapy risks are significant, but it’s important to keep things in perspective. For many, the benefits of chemotherapy outweigh the risks. Knowing the possible complications and being alert to warning signs can help reduce these risks.
| Risk Category | Description | Action Required |
| Common Side Effects | Nausea, fatigue, hair loss | Manage with medication and lifestyle adjustments |
| Serious Complications | Infections, organ damage, severe allergic reactions | Seek immediate medical attention |
| Warning Signs | Fever, severe pain, unusual bleeding | Immediate medical evaluation |
Being informed and proactive helps patients safely face chemotherapy’s challenges. It’s about weighing the risks against the benefits and working with healthcare providers to avoid complications.
Technology and Tools for Independent Living During Cancer Treatment
Chemotherapy can feel less lonely with new tech solutions. These tools help patients stay safe and independent. They make a big difference during tough times.
Medication Management Apps and Devices
Managing meds alone is hard for cancer patients. Medication management apps are a big help. They send reminders and track doses. Apps like Medisafe and MyMedSchedule keep patients on track.
There are also devices for managing meds. Pill dispensers with reminders are great for those with memory problems from chemo.
Remote Monitoring Solutions
Remote monitoring is a big step forward. It lets doctors check on patients from afar. Wearable devices track important health signs and send data to doctors in real-time.
“Remote monitoring technologies have the power to change cancer care. They let doctors act fast, even when they can’t be there.” –
An Oncologist
Smart Home Features for Cancer Patients
Smart home tech is also key for cancer patients. It makes life easier with voice control and safety features. For example, smart lights and thermostats adjust automatically.
- Voice assistants like Alexa or Google Assistant help with daily tasks.
- Smart lights adjust to the day, helping keep a normal routine.
- Smart thermostats keep homes comfy while saving energy.
These tech tools help cancer patients stay independent. They improve life quality during treatment.
Financial Navigation for Solo Cancer Patients
Dealing with the financial side of cancer treatment can be tough, even more so for those living alone. The cost of chemotherapy and the loss of income can really hit a patient’s wallet hard.
As a solo cancer patient, knowing about the financial help out there is key. We’ll look at important steps to take when dealing with chemotherapy costs.
Insurance Coverage Considerations
It’s important to understand your insurance. Check your policy to see what’s covered and what’s not. Key aspects to consider include:
- Coverage for chemotherapy drugs and related treatments
- Out-of-pocket costs, including deductibles and copays
- Maximum out-of-pocket limits
- Network providers and possible out-of-network costs
Talking to your healthcare provider’s billing team can also help. They can explain the financial side of your treatment plan.
Patient Assistance Programs
Many groups offer patient assistance programs (PAPs) to help with cancer treatment costs. These programs can give financial help, free or discounted meds, and more.
To get into these programs, patients usually need to:
- Find out if the drug company has a PAP
- Meet the program’s income and insurance criteria
- Apply with the needed financial documents
Planning for Unexpected Expenses
Cancer treatment can bring up unexpected costs, like travel and lodging for appointments. It’s smart to budget for these costs.
| Expense Category | Estimated Cost | Potential Assistance |
| Transportation | $100-$500 per month | Gas cards, public transportation vouchers |
| Lodging | $500-$1000 per month | Hotel discounts, cancer patient lodging programs |
| Food and Nutrition | $200-$500 per month | Meal delivery services, nutrition assistance programs |
By understanding insurance, using patient assistance programs, and planning for surprises, solo cancer patients can manage chemotherapy’s financial hurdles.
Success Stories: Thriving Alone During Chemotherapy
Cancer survivors who lived alone during chemotherapy share inspiring stories. Their experiences offer practical tips for staying independent and managing treatment challenges.
Practical Strategies from Cancer Survivors
They stress the value of being prepared, having a support network, and taking care of oneself. For example, making your home chemo-friendly can help deal with treatment side effects.
Practical tips from survivors include:
- Preparing meals in advance to conserve energy
- Creating an emergency contact system for immediate support
- Utilizing medication management apps to stay on track with treatment
- Engaging in virtual or in-person support groups for emotional support
How to Adapt These Approaches to Your Situation
Every person’s experience with chemotherapy is different. Yet, the strategies used by solo survivors can be tailored to fit various needs. It’s key to consider your personal situation, including your support network, home, and health.
To adapt these approaches:
- Evaluate your current living situation and identify any necessary modifications to enhance safety and comfort.
- Develop a support plan, including emergency contacts, regular check-ins, and transportation.
- Look into resources like patient assistance programs and smart home technologies to help with independent living.
Learning from cancer survivors who thrived alone during chemotherapy can help you prepare. It allows you to face treatment challenges while keeping your independence.
Conclusion: Making the Right Decision for Your Chemotherapy Journey
Living alone during chemotherapy needs careful planning. Understanding the challenges and preparing your home is key. Building a support network and using technology can help you stay independent.
It’s important to follow post-chemo driving guidelines for your safety and others’. This article provides strategies and guidelines to help you navigate chemotherapy treatment confidently.
Deciding on your care and daily life during chemotherapy is critical. Talk to your healthcare provider about your specific needs. This ensures the best outcome for your journey.
FAQ
Can I live alone while undergoing chemotherapy?
Yes, many people live alone during chemotherapy. But, it’s important to think about your health, support, and home. Make sure you can live safely alone.
How do chemotherapy side effects impact daily independence?
Side effects like fatigue and nausea can make daily tasks hard. Knowing these effects and planning can help you stay independent.
What questions should I ask my oncologist about living alone during chemotherapy?
Talk to your oncologist about your cancer and side effects. Ask about managing them and emergency plans. Also, find out about support services.
How can I prepare my home for solo living during chemotherapy?
Make your home comfortable and safe. Stock up on important supplies. A well-prepared home helps you stay independent.
Can I continue working while undergoing chemotherapy?
Many people work during chemotherapy. But, you need to plan and talk to your employer. Know your rights and benefits.
Can I drive after chemotherapy?
Driving after chemotherapy depends on your treatment. Some meds can affect your driving. Always follow your oncologist’s advice.
What are the driving restrictions after chemotherapy?
Driving rules vary with treatment. You might not drive for a while or at all. Always follow your doctor’s advice.
How can I ensure driving safety during and after chemotherapy?
Check if you can drive safely. Plan your routes and times. Use safe transportation options. Your safety is key.
Can you die from chemotherapy?
Chemotherapy is lifesaving but has risks. Know these risks and how to manage them. This can help avoid complications.
How can technology support independent living during cancer treatment?
Tools like apps and smart homes can help. They manage your meds and keep you safe. Technology is a big help.
What financial considerations should I be aware of as a solo cancer patient?
Know your insurance and look for help. Plan for extra costs. Understanding finances is tough, but it’s key.
Are there any success stories from cancer survivors who lived alone during chemotherapy?
Yes, many have thrived alone during treatment. Their tips and stories offer hope and help.
What are some tips for managing daily activities during chemotherapy?
Plan meals and save energy. Know when to ask for help. These tips can make a big difference.
How can I build a support network while living alone during chemotherapy?
Create a contact list and check in with loved ones. Join support groups. A strong network is vital for your well-being.
References
Benoot, C., Deschepper, R., Saelaert, M., Grypdonck, M., & Bilsen, J. (2015). Informal support needs of cancer patients who are living alone: a qualitative insight. Psycho-Oncology, 24(9), 1066“1072. https://pubmed.ncbi.nlm.nih.gov/25676614/





