For many couples, In Vitro Fertilization (IVF) is a beacon of hope in their journey to parenthood. Yet, the risk of ectopic pregnancy is a big concern. Ectopic pregnancies happen in about 1.4 to 5.4 percent of IVF cycles. This poses serious health risks if not caught early.
At Liv Hospital, we know how to balance IVF’s benefits with its risks. Our approach uses advanced reproductive technology and gives detailed patient counseling. We also use proven prevention strategies to help prospective parents on their journey.
Understanding the connection and risk factors for the question: can ivf cause ectopic pregnancy?
Key Takeaways
- Understanding the risks associated with IVF and ectopic pregnancy.
- The importance of early detection of ectopic pregnancy in IVF cycles.
- Strategies for preventing ectopic pregnancy during IVF.
- The role of advanced reproductive technology in managing risks.
- Comprehensive support for patients undergoing IVF treatment.
Understanding Ectopic Pregnancy Basics

To understand ectopic pregnancy, we need to know what it is and where it happens. An ectopic pregnancy is when a fertilized egg implants outside the uterus. This is a serious condition that needs quick medical help.
What is an Ectopic Pregnancy?
An ectopic pregnancy happens when a fertilized egg grows outside the uterus. This kind of pregnancy is not possible and can be very dangerous. The most common place for an ectopic pregnancy is the fallopian tube. But it can also happen in the ovary, cervix, or the abdominal cavity.
Common Locations for Ectopic Implantation
Ectopic pregnancies usually happen in the fallopian tube, which is about 90% of cases. The fallopian tube is not made for a growing embryo. As the embryo grows, it can cause the tube to burst, leading to severe bleeding.
Other places for ectopic implantation include:
- The ovary
- The cervix
- The abdominal cavity
These places are less common but can be very dangerous if not treated right.
General Risk Factors in All Pregnancies
There are several risk factors that can make an ectopic pregnancy more likely. Knowing these risk factors helps us find and prevent ectopic pregnancies early. Some common risk factors include:
| Risk Factor | Description |
|---|---|
| Previous ectopic pregnancy | Having had a previous ectopic pregnancy increases the risk. |
| Tubal damage or surgery | Damage to the fallopian tubes or previous tubal surgery can increase the risk. |
| Infertility | Women experiencing infertility, or those using assisted reproductive technology, are at higher risk. |
| Pelvic inflammatory disease | Infections such as pelvic inflammatory disease can cause tubal damage. |
By knowing these basics and risk factors, we can better spot who is at risk. This helps us understand why ectopic pregnancies happen. It also helps us work towards preventing and catching them early.
The Prevalence of Ectopic Pregnancy in IVF vs. Natural Conception
Ectopic pregnancy rates vary between IVF and natural conception. It’s important to understand these differences. This knowledge helps manage risks and make informed fertility treatment choices.
Statistical Comparison: 1.4-5.4% in IVF vs. 1-2% in Spontaneous Pregnancies
Research shows IVF pregnancies face a higher ectopic pregnancy risk. This risk ranges from 1.4% to 5.4%. In contrast, natural pregnancies have a risk of 1% to 2%. This difference emphasizes the need for close monitoring and risk assessment in IVF patients.
| Conception Method | Ectopic Pregnancy Rate |
|---|---|
| IVF | 1.4-5.4% |
| Natural Conception | 1-2% |
Why the Difference in Rates Exists
Several factors contribute to the higher ectopic pregnancy rate in IVF. These include underlying fertility issues, the IVF procedure, and the population undergoing IVF.
Underlying fertility issues often involve tubal damage or blockage. This increases the risk of ectopic pregnancy. The IVF procedure, including the embryo transfer technique, may also play a role. This is an area of ongoing research.
Recent Trends in Ectopic Pregnancy Rates with Modern IVF Techniques
Recent IVF advancements have improved pregnancy outcomes. This includes a possible decrease in ectopic pregnancy rates. The use of single embryo transfer has been key. It reduces the risk of multiple pregnancies and their complications.
As IVF technology evolves, it’s vital to continue research and monitoring. This will help understand and lower the risk of ectopic pregnancy in IVF patients.
Can IVF Cause Ectopic Pregnancy? The Scientific Perspective
The link between IVF and ectopic pregnancy is complex. We need to understand the science behind it. This involves looking at how IVF affects where an embryo implants.
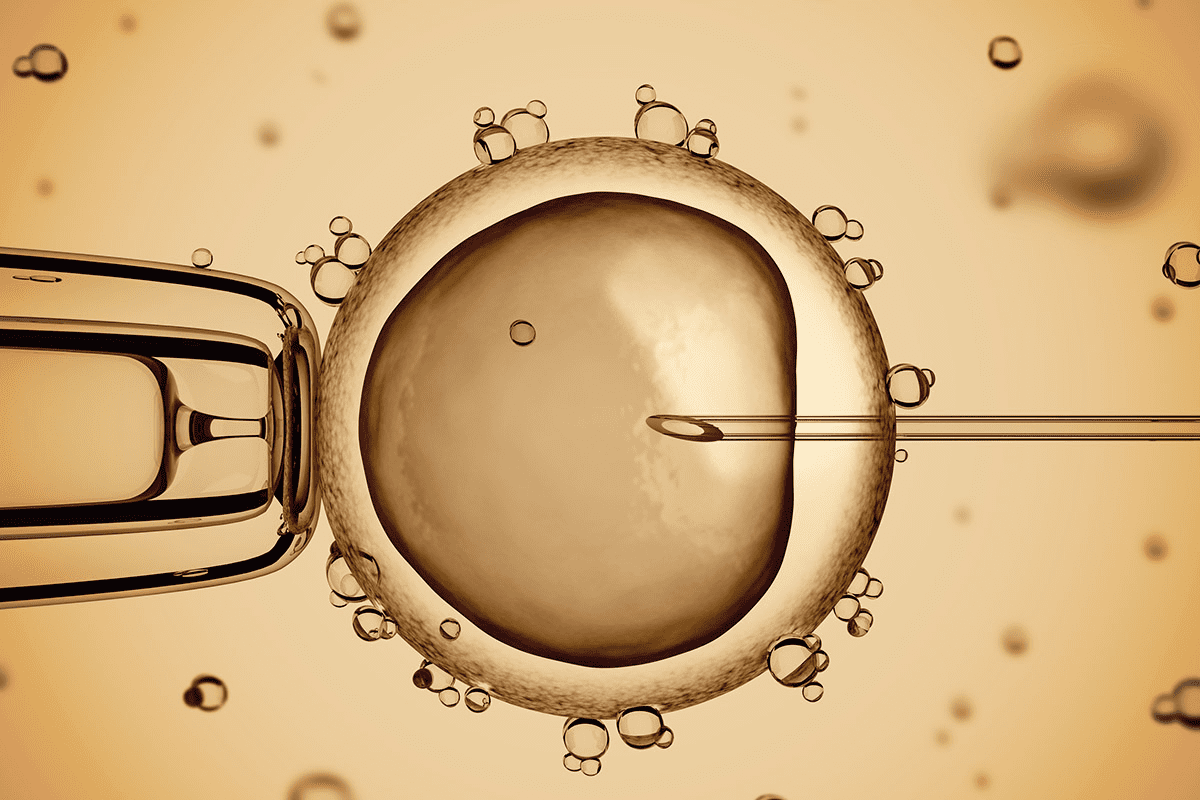
The Mechanism of Embryo Transfer in IVF
IVF involves putting embryos into the uterus with a catheter. This process is detailed and can affect the risk of ectopic pregnancy. The accuracy of the embryo transfer is key for the embryo’s development.
How Embryo Migration Occurs Despite Uterine Placement
Even with direct placement in the uterus, IVF can lead to ectopic pregnancy. Studies show that embryo migration can happen. This is due to uterine contractions, tubal damage, and other factors.
- Uterine contractions can displace the embryo.
- Tubal damage may facilitate ectopic implantation.
- Other anatomical or physiological factors can also play a role.
Correlation vs. Causation in IVF-Related Ectopic Pregnancies
It’s important to know the difference between correlation and causation. Seeing more ectopic pregnancies after IVF doesn’t mean IVF causes them. The fertility issues leading to IVF might also increase the risk of ectopic pregnancy.
Looking at the science behind IVF and ectopic pregnancy helps us understand the issue better. We see how embryo transfer works, the chance of embryo migration, and the difference between correlation and causation. This gives us a clearer view of the complex factors at play.
Primary Risk Factors for Ectopic Pregnancy During IVF
Several key risk factors can lead to ectopic pregnancy during IVF. Knowing these factors helps in preventing and managing the condition.
Tubal Factor Infertility
Tubal factor infertility is a big risk for ectopic pregnancy in IVF. Damage or blockage in the fallopian tubes, often from pelvic inflammatory disease or endometriosis, is common. The risk of ectopic implantation goes up because the embryo might implant in the tube instead of the uterus.
“The risk of ectopic pregnancy is higher in women with a history of tubal damage or disease,” studies show. This makes pre-IVF screening very important.
Decreased Ovarian Reserve
Lower ovarian reserve also raises the risk of ectopic pregnancy during IVF. Women with lower reserve might need more intense stimulation, which can affect embryo quality. Monitoring ovarian response closely is key to reducing these risks.
Previous Ectopic Pregnancy History
Having had an ectopic pregnancy before increases the risk of it happening again, even after IVF. Patients with a previous ectopic pregnancy should be counseled about their increased risk and closely monitored during IVF treatment.
Medical experts say, “A previous history of ectopic pregnancy should prompt careful evaluation and monitoring to prevent future occurrences.”
Understanding these primary risk factors helps healthcare providers advise IVF patients better. They can then take steps to lower the risk of ectopic pregnancy.
Additional Risk Factors in IVF Treatment
It’s important to know the extra risks linked to IVF treatment to lower the chance of ectopic pregnancy. IVF is a top choice for those struggling with infertility. But, some conditions and how treatment is done can up the risk of ectopic implantation.
Endometriosis with Prior Surgery
Endometriosis, with past surgery, is a big risk for ectopic pregnancy in IVF patients. This condition can cause adhesions and shape changes that might mess with where the embryo implants. Women with endometriosis and past surgeries need close watch during IVF.
Polycystic Ovary Syndrome (PCOS)
PCOS also ups the risk of ectopic pregnancy in IVF. The hormonal and ovulation issues in PCOS might make ectopic implantation more likely. Managing PCOS well during IVF, with careful hormone control, is key.
Thin Endometrium Concerns
A thin endometrium can make IVF tricky, possibly raising ectopic pregnancy risk. The endometrium’s thickness and how ready it is for implantation are vital. Looking into ways to make the endometrium thicker and more receptive is important.
Multiple Embryo Transfer Risks
Transferring more than one embryo in IVF is a risk for ectopic pregnancy, as well as for heterotopic pregnancy. While it might up the chance of getting pregnant, it also raises the risk of ectopic implantation. Choosing to transfer just one embryo is often advised to lower this risk.
Knowing these extra risks helps doctors and patients take steps to lower the chance of ectopic pregnancy in IVF. By tackling these risks, we can make IVF safer and more effective.
- Endometriosis: Increases risk due to possible adhesions and shape changes.
- PCOS: Hormonal imbalances might raise the risk of ectopic pregnancy.
- Thin Endometrium: Issues with implantation can increase ectopic risk.
- Multiple Embryo Transfer: Raises the risk of ectopic and heterotopic pregnancies.
Is Ectopic Pregnancy Hereditary or Genetic?
Many people wonder if ectopic pregnancy runs in families. We need to look into what we know about it and its possible genetic links.
Debunking Common Misconceptions
Some think ectopic pregnancy is passed down through genes. But, studies show it’s more about physical and health issues than genes.
Ectopic pregnancy is not seen as a genetic issue by doctors. It’s linked to things like past damage to the tubes, endometriosis, or other issues with the tubes.
The Non-Genetic Nature of Ectopic Pregnancy
Research shows ectopic pregnancy isn’t usually passed down. It happens due to:
- Tubal damage or issues
- Previous pelvic surgery
- Endometriosis
- In vitro fertilization (IVF) procedures
These factors can raise the risk, but they’re not genetic.
Why Family History May Be Relevant
Even though ectopic pregnancy isn’t genetic, some conditions that might lead to it can be. For example:
| Condition | Potential Genetic Link | Impact on Ectopic Pregnancy Risk |
|---|---|---|
| Endometriosis | Yes, can run in families | Increases risk due to possible tubal damage |
| Tubal abnormalities | Possible genetic component | Can increase the chance of ectopic implantation |
| Polycystic Ovary Syndrome (PCOS) | Has a genetic predisposition | May raise risk through hormonal effects |
Knowing these factors helps us understand the risk better. It also helps in taking steps to prevent it.
It’s important to remember that family history can influence the risk of ectopic pregnancy. But it’s not the direct cause.
Understanding the causes and risks helps us manage our reproductive health better. It allows us to make informed choices about our care.
Why Ectopic Pregnancies Occur: Anatomical and Physiological Factors
It’s important to know why ectopic pregnancies happen. They occur when a fertilized egg implants outside the uterus, often in the fallopian tube. This is due to a mix of anatomical and physiological factors.
Tubal Damage and Its Impact
Tubal damage is a big risk for ectopic pregnancy. Damage can come from pelvic inflammatory disease, surgeries, and endometriosis. When the fallopian tubes are damaged, the embryo can’t reach the uterus, leading to ectopic implantation.
Key factors contributing to tubal damage include:
- Pelvic inflammatory disease
- Previous tubal surgery
- Endometriosis
- History of sexually transmitted infections
Altered Tubal Function and Ciliary Movement
The fallopian tubes help move the embryo through ciliary movement and muscular contractions. If these functions are altered, the embryo can’t pass through normally. This increases the risk of ectopic pregnancy.
A study in the Journal of Assisted Reproduction and Genetics shows how important tubal function is. It says, “The complex movements of cilia and muscular contractions are key for embryo transport to the uterus.”
Impaired Uterine Environment and Receptivity
The uterine environment is vital for embryo implantation. If it’s not right, like a thin endometrium or poor receptivity, ectopic pregnancy risk goes up. IVF tries to improve this environment, but some conditions can remain risky.
| Uterine Factor | Impact on Ectopic Pregnancy Risk |
|---|---|
| Thin Endometrium | Increased risk due to reduced implantation site |
| Adenomyosis | Altered uterine environment affecting embryo implantation |
| Uterine Fibroids | Potential distortion of uterine cavity |
Hormonal Influences on Embryo Transport
Hormones play a big role in embryo transport and implantation. Hormonal imbalances or changes during IVF can disrupt the reproductive system. This can lead to ectopic pregnancy.
“Hormonal influences on the reproductive system are complex and multifaceted, affecting various aspects of embryo transport and implantation.”
Understanding these factors helps us manage and prevent ectopic pregnancies in IVF. It’s key to assess individual risks and create personalized strategies to lower ectopic pregnancy risk.
Early Detection of Ectopic Pregnancy in IVF Patients
Spotting an ectopic pregnancy early is key in IVF treatments. With more people turning to IVF, knowing the risks and signs is vital. This knowledge helps both patients and doctors.
Warning Signs and Symptoms to Monitor
IVF patients need to watch for signs of ectopic pregnancy. Look out for abdominal pain, vaginal bleeding, and dizziness. If you notice these, see a doctor right away.
Common symptoms to watch for:
- Abdominal pain, often on one side
- Vaginal bleeding or spotting
- Dizziness or fainting
- Shoulder tip pain
- Nausea and vomiting
Diagnostic Procedures and Timeline
To find an ectopic pregnancy, doctors use ultrasound and hCG level checks. The first ultrasound is at 4-5 weeks after the transfer. Then, they watch hCG levels closely.
| Diagnostic Procedure | Timeline | Purpose |
|---|---|---|
| Initial Ultrasound | 4-5 weeks post-transfer | To locate the pregnancy |
| hCG Level Checks | Every 48 hours initially | To assess the rise in hCG levels |
| Follow-up Ultrasound | 6-7 weeks post-transfer | To confirm the location and viability of the pregnancy |
The Importance of Early Monitoring After IVF
Monitoring early after IVF is vital for spotting ectopic pregnancies. We urge patients to keep up with their follow-up appointments. This helps catch any problems early.
By knowing the signs and getting regular tests, IVF patients can do better if they have an ectopic pregnancy. We stress the need for patient education and regular checks for the best care.
Treatment Options for Ectopic Pregnancy After IVF
Treatment for ectopic pregnancy after IVF includes medical and surgical options. The right choice depends on the pregnancy’s size, location, and the patient’s health. It also considers their wish for future fertility.
Medical Management with Methotrexate
For small, early ectopic pregnancies, methotrexate is often used first. This drug stops the growth of fast-dividing cells. It’s given by injection, and its success is checked with blood tests and ultrasounds.
Monitoring is key because methotrexate can have side effects. Sometimes, more doses or other treatments are needed. Patients taking methotrexate should avoid certain medicines and foods.
Surgical Interventions: Laparoscopy vs. Laparotomy
When the ectopic pregnancy is advanced or medical treatment fails, surgery is needed. There are two main surgical methods: laparoscopy and laparotomy.
- Laparoscopy uses small incisions for a camera and tools. It’s chosen for its quick recovery and less pain.
- Laparotomy uses a bigger incision for direct access. It’s for complex cases or when there’s a lot of bleeding.
Recovery and Follow-up Care
After treatment, follow-up care is vital. It checks if the ectopic pregnancy is gone and watches the patient’s healing. This includes blood tests to see hCG levels drop.
Patients are told about signs of complications like heavy bleeding or severe pain. They also get help for emotional issues.
Emotional Support and Counseling
Having an ectopic pregnancy can be tough, even after IVF. Counseling and emotional support are key. They help patients deal with their feelings and plan for future fertility treatments.
We focus on the whole person, treating both body and mind during this hard time.
How to Prevent Ectopic Pregnancy During IVF Treatment
To lower the risk of ectopic pregnancy during IVF, we use thorough screening and the best embryo transfer methods. Understanding what causes ectopic pregnancy helps us find ways to prevent it. This way, IVF patients can lower their risk of this serious issue.
Pre-IVF Screening and Risk Assessment
Before starting IVF, a detailed screening is key. We check the fallopian tubes, look at ovarian health, and review any past ectopic pregnancies. This helps us make a treatment plan that reduces the risk of ectopic pregnancy.
| Risk Factor | Assessment Method | Mitigation Strategy |
|---|---|---|
| Tubal Damage | Hysterosalpingography (HSG) or laparoscopy | Consider tubal surgery or IVF with careful embryo placement |
| Decreased Ovarian Reserve | Blood tests for AMH and FSH levels | Optimize ovarian stimulation protocols |
| Previous Ectopic Pregnancy | Review medical history | Close monitoring during IVF, consider single embryo transfer |
Optimizing Embryo Transfer Techniques
The way we transfer embryos is very important. We use ultrasound to place the embryo exactly where it should be in the uterus. We also avoid using too much force or touching the top of the uterus during transfer to lower the risk of ectopic pregnancy.
Single vs. Multiple Embryo Transfer Considerations
Choosing between single or multiple embryo transfer is a big decision. While multiple embryos increase the chance of pregnancy, they also raise the risk of ectopic pregnancy. We often recommend single embryo transfer, which balances success with safety, for those at higher risk.
Personalized Risk Management Strategies
Every patient’s situation is different, so we tailor our approach to manage ectopic pregnancy risk. We work with our patients to create strategies that fit their needs. This might include adjusting the IVF protocol, monitoring the pregnancy closely, or other preventive steps.
By taking a detailed and personalized approach to preventing ectopic pregnancy during IVF, we can greatly reduce the risk. This helps improve the success rate of the treatment for our patients.
Conclusion: Navigating IVF Treatment with Awareness of Ectopic Pregnancy Risk
Understanding the risks of ectopic pregnancy is key when going through IVF. Knowing these risks helps both patients and doctors work together. This teamwork aims to avoid complications and ensure success.
When it comes to IVF, the risk of ectopic pregnancy is a big concern. Patients can take steps to lower this risk. This includes getting checked before IVF, using the best ways to transfer embryos, and choosing to transfer one embryo at a time.
Our talk has shown how important it is to be aware and manage risks well. By tailoring risk management to each person, we can make IVF more successful. This helps patients on their journey to having a baby.
To successfully navigate IVF, patients and doctors must work together. By staying informed and collaborative, we can reduce risks. This way, we can make IVF a success for everyone involved.
FAQ
What is an ectopic pregnancy?
An ectopic pregnancy happens when a fertilized egg implants outside the uterus, often in a fallopian tube. This type of pregnancy is not viable and can be life-threatening if not treated promptly.
Are ectopic pregnancies hereditary?
Ectopic pregnancies are generally not hereditary. While there might be some family tendencies, ectopic pregnancy is mostly linked to individual health conditions, not genetics.
Is ectopic pregnancy genetic?
Ectopic pregnancy is not caused by genetics. But, some conditions like tubal damage or endometriosis, which can lead to ectopic pregnancy, might have a genetic link.
Why does an ectopic pregnancy happen?
Ectopic pregnancy occurs due to several reasons. These include tubal damage, altered tubal function, and hormonal influences that affect embryo transport and implantation.
Can IVF cause ectopic pregnancy?
IVF itself doesn’t directly cause ectopic pregnancy. But, it might increase the risk due to factors like embryo quality, transfer technique, and patient characteristics.
What are the risks of ectopic pregnancy with IVF?
The risk of ectopic pregnancy with IVF is higher than natural conception. It ranges from 1.4% to 5.4%. This increased risk is due to tubal factor infertility and previous ectopic pregnancy history.
How to prevent an ectopic pregnancy during IVF?
To prevent ectopic pregnancy during IVF, pre-IVF screening is key. Also, optimizing embryo transfer techniques and considering single embryo transfer are important. Personalized risk management strategies are also essential.
What are the warning signs of an ectopic pregnancy after IVF?
Warning signs of an ectopic pregnancy after IVF include abdominal pain, vaginal bleeding, shoulder pain, and dizziness. Patients should seek medical attention promptly if they experience these symptoms.
How is ectopic pregnancy diagnosed after IVF?
Diagnosis of ectopic pregnancy after IVF involves ultrasound and monitoring of beta-hCG levels. Early detection is critical for effective management and minimizing complications.
What are the treatment options for ectopic pregnancy after IVF?
Treatment options for ectopic pregnancy after IVF include medical management with methotrexate and surgical interventions like laparoscopy or laparotomy. The choice depends on the severity and individual patient circumstances.
Can you have an ectopic pregnancy with IVF?
Yes, it’s possible to have an ectopic pregnancy with IVF. While IVF is a controlled process, the risk of ectopic pregnancy exists, mainly in patients with certain risk factors.
Who is at risk of ectopic pregnancy during IVF?
Patients with tubal factor infertility, previous ectopic pregnancy history, endometriosis, and those undergoing multiple embryo transfer are at higher risk of ectopic pregnancy during IVF.
How to minimize the risk of ectopic pregnancy during IVF?
To minimize the risk of ectopic pregnancy during IVF, careful patient selection is key. Optimizing embryo transfer techniques and adopting personalized risk management strategies, including single embryo transfer, are also important.
References:
National Center for Biotechnology Information. IVF and Ectopic Pregnancy: Risks and Prevention. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5362426/)