Last Updated on November 20, 2025 by Ugurkan Demir
Sickle cell anemia is a genetic disorder that affects how red blood cells are made. It makes these cells misshapen and prone to breaking down. This can lead to anemia, blood clots, and organ damage.
Many people wonder, can sickle cell anemia cause blood clots? Recent studies have found that sickle cell anemia does increase the risk of clot formation. These clots often form in veins, which can lead to serious health complications. Understanding this link is key to managing and treating the condition effectively.
Key Takeaways
- Sickle cell anemia is a genetic disorder affecting hemoglobin production.
- It increases the risk of blood clots due to irregularly shaped red cells.
- Inflammatory changes in blood vessels also contribute to clot risk.
- Understanding the condition’s impact on blood clotting is key.
- Managing sickle cell anemia can help prevent serious complications.
Understanding Sickle Cell Anemia: The Basics
Learning about sickle cell anemia is key to understanding its effects globally. It’s a genetic disorder that changes red blood cells, making them sickle-shaped. This shape makes it hard for them to move through blood vessels, causing health problems.
What Is Sickle Cell Anemia?
Sickle cell anemia happens when red blood cells make abnormal hemoglobin, called hemoglobin S. This makes the cells stiff and sickle-shaped, mainly when there’s less oxygen. The sickle shape leads to early cell death and health issues like anemia and pain.
Genetic Factors and Inheritance Patterns
Sickle cell anemia is passed down in an autosomal recessive pattern. This means you need two bad genes, one from each parent, to have the disease. Carriers have one bad gene and usually don’t show symptoms but can pass the gene to their kids.
Carriers have a 50% chance of passing the mutated gene to each child. If both parents are carriers, there’s a 25% chance with each pregnancy that the child will have sickle cell anemia. Knowing this helps families with a history of the disease.
Global Prevalence and Demographics
Sickle cell anemia is common in tropical and subtropical areas, like Africa, the Mediterranean, and the Middle East. In the U.S., it affects many ethnic groups, but most in African Americans. It’s linked to malaria, as the sickle cell trait protects against it.
The World Health Organization says sickle cell anemia affects millions worldwide, mostly in sub-Saharan Africa. In the U.S., about 1 in 500 African Americans have sickle cell disease, and 1 in 12 carry the trait.
People with sickle cell disease or the trait are at higher risk of venous thromboembolism. Knowing who’s at risk helps with public health planning and awareness.
The Normal Blood Clotting Process

Blood clotting is key to stopping bleeding when a blood vessel gets hurt. It’s a complex process where many factors and cells work together to form a clot.
How Blood Normally Clots
When a blood vessel is damaged, the body first constricts it to reduce blood flow. Then, platelets, small cell fragments in the blood, are activated. They stick to the injury site and clump together, forming a platelet plug.
The coagulation cascade starts, leading to the formation of fibrin, a protein that strengthens the platelet plug. This creates a stable clot. This process is tightly regulated to ensure clotting only happens when needed and stays at the injury site.
Key Components of the Clotting Cascade
The clotting cascade involves many clotting factors, proteins in blood plasma. These factors are labeled with Roman numerals (I through XIII). They work in a sequence to form a clot. The main components include:
- Fibrinogen (Factor I): Converted into fibrin to form the clot.
- Prothrombin (Factor II): Converted into thrombin, which then converts fibrinogen into fibrin.
- Tissue Factor (Factor III): Starts the extrinsic pathway of coagulation.
| Clotting Factor | Function |
| Fibrinogen | Forms fibrin clot |
| Prothrombin | Precursor to thrombin |
| Tissue Factor | Initiates extrinsic pathway |
Regulatory Mechanisms for Normal Clotting
To avoid too much clotting, the body has several checks. Anticoagulant proteins like antithrombin and protein C stop clotting factors. Fibrinolysis, the process of dissolving clots, also plays a role.
Keeping the balance between clotting and dissolving is vital. If this balance is off, it can lead to either too much clotting or bleeding problems.
Does Sickle Cell Cause Blood Clots? The Connection Explained
Sickle cell disease is linked to a higher risk of blood clots. Research shows people with sickle cell disease or the sickle cell trait face up to a 1.45 times higher chance of venous thromboembolism.
Statistical Evidence of Increased Clotting Risk
Studies show sickle cell disease patients are at a higher risk of blood clots. The evidence is clear, making it important to be aware and take preventive steps.
- Increased risk of venous thromboembolism in SCD patients
- Higher incidence of deep vein thrombosis (DVT) in SCD
- Research findings indicating a strong link between SCD and clotting risk
The 1.45x Higher Risk of Venous Thromboembolism
People with sickle cell disease face a significantly higher risk of venous thromboembolism. This is a key factor in managing SCD, as it can lead to serious complications.
Key findings include:
- A 1.45 times higher risk of venous thromboembolism in SCD patients
- Increased risk of recurrence in patients with a history of thromboembolic events
- The need for tailored anticoagulation strategies in SCD patients
Research Findings on Sickle Cell and Clotting
Research has shed light on why SCD increases clotting risk. Knowing these mechanisms is key to creating effective prevention and treatment plans.
Some key research findings include:
- The role of chronic inflammation in promoting clotting
- The impact of abnormal blood cell adhesion on vascular occlusion
- The possibility of new therapies targeting specific SCD-related clotting pathways
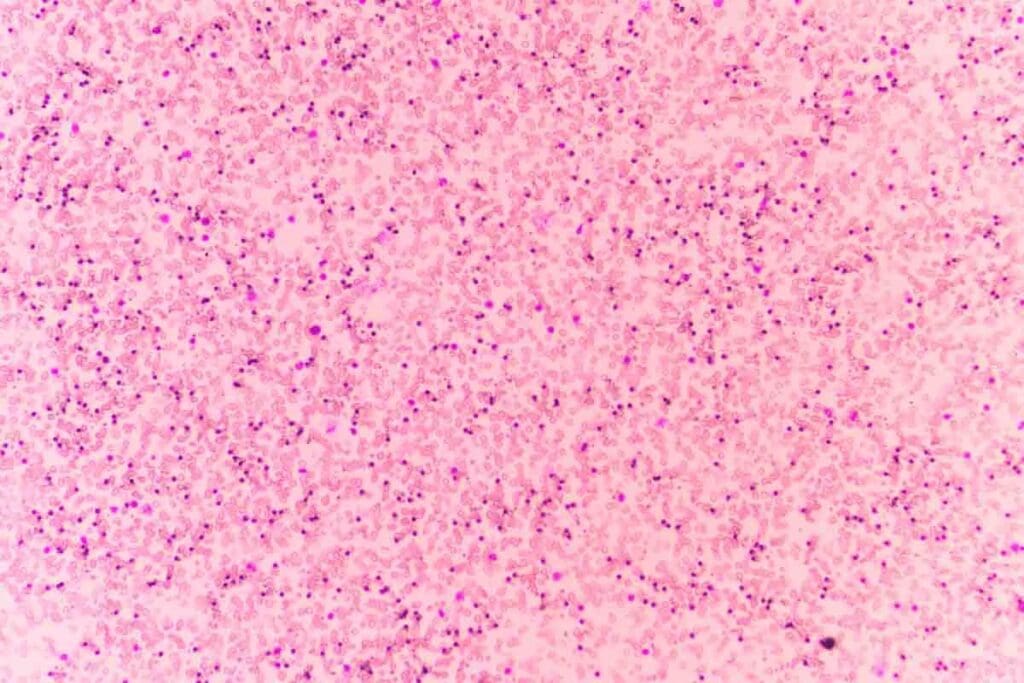
Structural Changes in Sickle Blood Cells
Sickle cell anemia changes red blood cells in big ways. It makes them sickle-shaped because of abnormal hemoglobin, called hemoglobin S.
The Sickling Process and Cell Deformation
Red blood cells deform into sickle shapes when oxygen levels are low. This happens because of hemoglobin S polymerization. It changes their normal shape.
The sickling process is reversible at first. But, repeated episodes cause permanent damage. This makes cells more likely to break down and live shorter lives.
How Abnormal Cell Shape Affects Blood Flow
The sickle shape of red blood cells affects blood flow a lot. These cells are stiff and often get stuck in small blood vessels. This blocks blood flow and causes pain and tissue damage.
Vaso-occlusion can happen in many organs, like the spleen, lungs, and kidneys. It can damage these organs over time. The reduced blood flow also leads to chronic inflammation in sickle cell patients.
Cellular Adhesion and Vessel Occlusion
Sickled red blood cells stick more to blood vessel walls. This is because of adhesion molecules. It’s a big part of why sickle cell disease causes vaso-occlusive crises.
The stickiness and shape of sickled cells cause blood vessels to block. This blocks blood flow and starts an inflammatory response. It makes the condition worse.
Understanding how sickle blood cells change is key to understanding sickle cell anemia. Research on these changes helps find new treatments to lessen the disease’s effects.
Inflammatory Pathways in Sickle Cell Disease
Sickle cell disease is characterized by chronic inflammation. This inflammation affects many parts of the disease. It’s not just a result of the disease but also a cause of its complications, like blood clots.
Chronic Inflammation and Its Effects
Chronic inflammation in sickle cell disease causes damage to organs and systems. It activates inflammatory cells and releases pro-inflammatory cytokines. These actions worsen the disease.
This inflammation impacts not just the blood system but also causes problems with blood vessels. It raises the risk of blood clots.
Inflammatory Markers in Sickle Cell Patients
Patients with sickle cell disease have high levels of inflammatory markers. These include:
- C-reactive protein (CRP)
- Interleukin-6 (IL-6)
- Tumor necrosis factor-alpha (TNF-alpha)
These markers show the disease is active. They also predict possible complications, like vaso-occlusive crises and blood clots.
How Inflammation Contributes to Clotting
Inflammation plays a big role in the clotting problems seen in sickle cell disease. Inflammatory cytokines and mediators make endothelial cells and monocytes produce tissue factor. This starts the coagulation process.
Inflammation also activates platelets and releases pro-coagulant microparticles. This makes clotting worse.
The link between inflammation and coagulation creates a cycle that increases the risk of blood clots in sickle cell disease. Understanding this is key to finding effective treatments for the disease and its complications.
Vascular Endothelial Dysfunction in Sickle Cell Anemia
The vascular endothelium in sickle cell anemia patients is not working right. This leads to many problems, like a higher chance of blood clots.
Damage to Blood Vessel Linings
Sickle cell anemia harms the blood vessel linings, called the endothelium. Sickled red blood cells stick to these cells, causing inflammation and damage. This makes the endothelium work poorly, which is bad for blood vessels.
Endothelial damage in sickle cell anemia means more adhesion molecules and pro-inflammatory cytokines. This makes sickled red blood cells, white blood cells, and platelets stick to the endothelium. This worsens the damage to blood vessels.
Endothelial Activation and Clotting Risk
Endothelial activation is a big problem in sickle cell disease. When the endothelium is activated, it makes more pro-coagulant factors. This increases the risk of blood clots.
The activation of endothelial cells also releases von Willebrand factor and other pro-thrombotic factors. These factors make sickle cell patients more likely to form blood clots.
“The activation of endothelial cells and the subsequent release of pro-coagulant factors play a critical role in the development of thrombotic complications in sickle cell disease.” –
A leading researcher in hematology
Nitric Oxide Depletion and Its Consequences
Nitric oxide (NO) is important for blood vessels. It helps control blood flow and prevents platelet activation. In sickle cell anemia, NO is lost because of hemoglobin from lysed red blood cells. This loss causes blood vessels to constrict and platelets to activate more, raising the risk of blood clots.
| Mechanism | Effect on Vascular Health | Consequence |
| Endothelial Damage | Impaired vascular function | Increased risk of blood clots |
| Endothelial Activation | Pro-coagulant state | Hypercoagulability |
| Nitric Oxide Depletion | Vasoconstriction and platelet activation | Thrombotic events |
The vascular endothelial dysfunction in sickle cell anemia is complex. Understanding these mechanisms is key to finding effective treatments for the disease and its complications.
Deep Vein Thrombosis (DVT) and Sickle Cell Disease
People with sickle cell disease face a higher risk of deep vein thrombosis. It’s important to know why and how to manage this risk. Deep vein thrombosis happens when blood clots form in deep veins, usually in the legs. If not treated quickly, it can lead to serious problems like pulmonary embolism.
Prevalence of DVT in Sickle Cell Patients
Research shows that sickle cell disease patients are more likely to get DVT than others. The numbers are alarming, showing the need for early detection and prevention.
| Population | Prevalence of DVT |
| General Population | 0.1-0.2% |
| SCD Patients | 1-2% |
Risk Factors and Triggers for SCD with DVT
Several factors increase DVT risk in SCD patients. These include chronic inflammation, endothelial dysfunction, and hypercoagulability. Other factors like immobility, surgery, and previous history of DVT also play a role.
Diagnostic Challenges in Sickle Cell Patients
Diagnosing DVT in SCD patients is tough. Symptoms can be similar to other SCD issues, like vaso-occlusive crises. Doctors must use a mix of clinical checks, lab tests, and imaging to make an accurate diagnosis.
Key Diagnostic Considerations:
- Clinical evaluation
- D-dimer testing
- Ultrasound imaging
Pulmonary Embolism: A Serious Complication
Sickle cell disease patients are at a higher risk of pulmonary embolism. This is a serious condition where a blood clot blocks blood flow to the lungs. It’s life-threatening and needs quick diagnosis and treatment.
Increased Risk Factors
Sickle cell disease changes how blood cells work. It makes them stick together and block vessels, leading to pulmonary embolism.
The sickling process in sickle cell disease increases the risk of pulmonary embolism. Abnormal red blood cells can block small blood vessels. This causes tissue ischemia and inflammation, leading to blood clot formation.
Distinguishing PE from Acute Chest Syndrome
Managing sickle cell disease can be tricky. It’s hard to tell pulmonary embolism from acute chest syndrome because they share similar symptoms. Accurate diagnosis is key because treatment differs.
Acute chest syndrome is a big problem for sickle cell disease patients. It’s characterized by a new lung problem on chest X-rays, fever, and respiratory symptoms. While it’s mainly treated with supportive care, pulmonary embolism might need anticoagulation therapy.
PE Complications in Sickle Cell Disease
Pulmonary embolism can cause serious problems in sickle cell disease patients. It can lead to right ventricular failure because of the strain on the right heart. It can also cause hypoxemia, making the sickling process worse.
Management Approaches for PE in Sickle Cell Disease
Managing pulmonary embolism in sickle cell disease patients is complex. It involves anticoagulation therapy to stop more clots. Choosing the right anticoagulant and treatment length is important, considering bleeding risks and other health issues.
A medical expert says,
“The management of pulmonary embolism in sickle cell disease requires a delicate balance between preventing further thrombotic events and minimizing the risk of bleeding complications.”
Prevention is key, including staying hydrated and exploring new treatments. These steps help reduce the risk of pulmonary embolism in these patients.
Can Anemia Cause Blood Clots? The Paradoxical Relationship
Anemia and blood clots have a complex relationship. Anemia, which is a lack of red blood cells, can lead to blood clots. This happens because the body tries to make up for the lack of red blood cells in different ways.
Compensatory Mechanisms in Chronic Anemia
When anemia lasts a long time, the body tries to fix it. It does this by pumping more blood and growing new blood vessels. These changes can affect how blood clots form.
- More blood being pumped can make blood flow faster. This can damage the lining of blood vessels and lead to clotting.
- New blood vessels can form in strange ways. This can also increase the risk of blood clots.
Hypoxia and Its Effects on Blood Clotting
Chronic anemia often means tissues don’t get enough oxygen. This lack of oxygen can change how blood clots form. It makes the body more likely to form clots.
Key effects of hypoxia on blood clotting include:
- Hypoxia makes the body produce more factors that help clots form.
- It also makes the lining of blood vessels stick more to platelets, helping clots form.
- Hypoxia can damage the lining of blood vessels, making them more likely to clot.
Anemia and Blood Clots in Legs: Special Considerations
Anemia can make blood clots in the legs more likely. This is called deep vein thrombosis (DVT). Changes in blood flow and damage to blood vessel linings in the legs can raise the risk of DVT in people with anemia.
Special considerations include:
- Being unable to move can cause DVT and is often seen in people with anemia because they are tired.
- Anemia can make heart problems worse. Heart problems can increase the risk of DVT.
Can Blood Clots Cause Anemia? Reverse Causality
Blood clots can greatly affect anemia by causing blockages in blood vessels. It’s important to grasp this relationship to manage anemia effectively.
Mechanisms of Clot-Induced Anemia
When blood clots block blood flow, it can damage tissues and lower red blood cell counts. This makes it harder for organs to get the oxygen they need.
The main reasons for clot-induced anemia include:
- Reduced blood flow due to clot obstruction
- Increased inflammation from tissue damage
- Impaired red blood cell production due to chronic disease
Tissue Damage from Vascular Occlusion
Blood clots can cause serious damage by blocking oxygen and nutrients. This leads to cell death and organ failure.
The damage can affect many organs and systems, such as:
- The kidneys, leading to chronic kidney disease
- The spleen, resulting in splenic infarction
- The lungs, potentially causing pulmonary embolism
The Cycle of Clotting and Worsening Anemia
Blood clots can start a cycle that makes anemia worse. As clots block blood flow, they cause more tissue damage, leading to more severe anemia.
Breaking this cycle is hard because clotting and anemia are linked. A thorough approach is needed to tackle both issues.
It’s key to understand how blood clots and anemia interact. By tackling the root causes of clot-induced anemia, doctors can help patients better.
Sickle Cell Trait vs. Disease: Differing Clotting Risks
People with sickle cell trait and those with sickle cell disease face different risks of blood clots. Sickle cell trait means having one sickle cell gene. Sickle cell disease means having two, leading to more serious health issues.
Understanding Sickle Cell Trait
Sickle cell trait is usually harmless but can cause problems in extreme situations. It doesn’t lead to the same level of anemia or pain as sickle cell disease.
Clotting Risk with Sickle Cell Trait
Studies show that sickle cell trait lowers the risk of blood clots compared to sickle cell disease. This is important for understanding the health risks of each condition. Even though the risk is lower, some factors can increase the chance of clotting in those with sickle cell trait.
Special Considerations for Athletes with Trait
Athletes with sickle cell trait need special care because of their intense physical activities. Exertion-related complications can happen. It’s important for them to know their trait status and take precautions. This includes staying hydrated, avoiding extreme conditions, and getting medical checks.
It’s key to understand these differences to manage health risks and provide the right care. Healthcare providers can give specific advice and help to reduce clotting risks based on these differences.
Prevention and Management of Blood Clots in Sickle Cell Patients
It’s important to prevent and manage blood clots in sickle cell patients. Sickle cell anemia increases the risk of blood clots. This is due to abnormal blood cells, chronic inflammation, and damaged blood vessels.
Anticoagulation Approaches and Considerations
Anticoagulation therapy is key in preventing blood clots in sickle cell patients. Anticoagulants like warfarin and heparin help stop new clots and prevent existing ones from growing. The right anticoagulant depends on the patient’s risk of clotting and bleeding.
Monitoring is vital to adjust dosages and avoid bleeding risks. A study in the Journal of Clinical Oncology emphasizes the importance of balancing clotting and bleeding risks.
“The management of anticoagulation therapy in patients with sickle cell disease is complex and requires a tailored approach to minimize risks and maximize benefits.”
Hydration and Its Importance
Hydration is key in preventing blood clots in sickle cell patients. Adequate hydration improves blood flow and reduces sickled red blood cells. This lowers the risk of vaso-occlusive crises and clot formation.
A study shows hydration’s role in managing sickle cell disease. It states that hydration is a simple yet effective way to reduce complications.
Novel Therapies Under Investigation
New therapies are being developed to prevent and manage blood clots in sickle cell patients. These include new anticoagulants and drugs that target the sickling process and clot formation. For example, crizanlizumab, a P-selectin inhibitor, has shown promise in reducing vaso-occlusive crises.
These advancements offer new hope for reducing blood clot risks and improving patient outcomes.
Conclusion: The Complex Relationship Between Sickle Cell Anemia and Blood Clotting
Sickle cell anemia raises the risk of blood clots. This is because of changes in blood cells and inflammation in blood vessels. The link between sickle cell anemia and blood clotting is complex, involving many factors.
The sickling of red blood cells causes them to break down early. They stick to blood vessel walls, making clots more likely. Inflammation and damage to blood vessel walls also play a role. Knowing how these factors work is key to managing blood clot risks in sickle cell patients.
Managing sickle cell anemia includes using anticoagulants, staying hydrated, and exploring new treatments. By understanding the relationship between sickle cell anemia and blood clotting, doctors can help patients better. This can lead to better health outcomes for those with sickle cell anemia.
FAQ
Does sickle cell anemia increase the risk of blood clots?
Yes, sickle cell anemia raises the risk of blood clots. This is due to chronic inflammation and damage to blood vessels. Also, the shape of sickle blood cells plays a role.
Can anemia cause blood clots in legs?
Anemia itself doesn’t directly cause blood clots. But, it can lead to changes that increase clotting risk. Sickle cell anemia, in particular, can cause leg clots due to blood cell changes.
What is the relationship between deep vein thrombosis and sickle cell disease?
People with sickle cell disease face a higher risk of deep vein thrombosis (DVT). This is due to inflammation, blood vessel damage, and blood cell issues.
Can blood clots cause anemia?
Yes, blood clots can lead to anemia. This happens when clots damage tissues and block blood flow. It creates a cycle of clotting and worsening anemia.
Are individuals with sickle cell trait at risk of blood clots?
Those with sickle cell trait face a lower risk of blood clots than those with sickle cell disease. But, intense physical activity can increase their clotting risk.
How can blood clots be prevented and managed in sickle cell patients?
To prevent and manage blood clots in sickle cell patients, anticoagulation, hydration, and new treatments are used. Early diagnosis and treatment are key to avoiding complications.
What is the role of inflammation in sickle cell disease and blood clotting?
Inflammation is key in sickle cell disease and blood clotting. It activates blood vessel walls, raises inflammatory markers, and promotes clotting.
How does vascular endothelial dysfunction contribute to blood clotting in sickle cell anemia?
Vascular endothelial dysfunction in sickle cell anemia damages blood vessel linings. It also reduces nitric oxide, increasing the risk of blood clots.
Can pulmonary embolism be distinguished from acute chest syndrome in sickle cell patients?
It’s hard to tell pulmonary embolism (PE) from acute chest syndrome (ACS) in sickle cell patients. They share similar symptoms. Imaging studies are needed to accurately diagnose and treat these conditions.
What are the complications of pulmonary embolism in sickle cell disease?
Pulmonary embolism can cause serious problems in sickle cell patients. These include respiratory failure, heart strain, and even death. Quick diagnosis and treatment are vital to avoid these outcomes.
References
- World Health Organization (WHO). (2006). Sickle-cell anaemia: Report by the Secretariat. Fifty-Ninth World Health Assembly: https://apps.who.int/gb/ebwha/pdf_files/wha59/a59_9-en.pdf